Raising a child with a limb difference comes with many responsibilities—and unexpected expenses. One of the biggest concerns for families is how to afford a prosthetic hand or arm that fits their growing child. These devices are not just one-time purchases. As children grow, their needs change. Prosthetics must be replaced, adjusted, and maintained regularly. That means ongoing costs that can quickly add up.
The good news is that parents are not alone. Support is available. In India, more families are discovering ways to make prosthetic care affordable through insurance, government schemes, non-profit funding, and even corporate social programs. These financial tools can ease the pressure, giving your child the freedom to move, play, and grow with confidence.

Understanding Insurance Coverage for Pediatric Prosthetics in India
The Basics of Health Insurance and Prosthetic Support
Health insurance is something most families are familiar with, but not everyone knows whether it covers prosthetics, especially for children. In India, the answer isn’t always simple.
Many standard health insurance plans do not openly mention prosthetics in their brochures or benefit outlines. But that doesn’t mean coverage isn’t available. It often depends on how the policy is structured, the insurer, and how the claim is presented.
Some private insurance plans include coverage for external medical devices, especially when they are medically necessary. Prosthetics often fall under this category.
For children with congenital limb differences or those who lose a limb due to illness or injury, prosthetics may be prescribed by a doctor. In such cases, parents can request reimbursement under durable medical equipment (DME) or assistive devices.
However, coverage for pediatric prosthetics is not standard across all policies. Some may only offer partial support.
Others may require pre-authorization or written recommendations from specific types of doctors. This makes it very important for families to review the fine print of their policy or speak directly to their insurer.
Most families don’t find out whether prosthetics are covered until they need them—and by then, the process can feel confusing. That’s why understanding your insurance policy ahead of time can save both money and stress.
How to Talk to Your Insurance Provider
If your child needs a prosthetic hand or arm, the first step is to reach out to your insurance company and ask a few clear questions. Start by explaining the situation.
Let them know the prosthetic is not for cosmetic use—it’s for daily function, mobility, and development. Use the doctor’s prescription as support. If the prosthetic is medically necessary, insurers are more likely to listen.
Ask whether your policy includes coverage for orthopedic appliances or external medical devices. You can also check if the company has a reimbursement clause for out-of-pocket medical expenses.
In some cases, even if prosthetics aren’t clearly listed, families can still submit a claim under miscellaneous benefits or surgical aids.
Documentation is key. Keep everything—prescriptions, evaluations, receipts, and any communication with the prosthetic provider. If your prosthetist can provide a breakdown of the device’s function and necessity, this can further support your claim.
It’s also helpful to be persistent. Sometimes, initial claims are rejected simply because they don’t fit neatly into a listed category.
Appealing the decision with better documentation or a doctor’s letter can make a difference.
If navigating the insurance conversation feels too overwhelming, some prosthetic clinics and providers offer assistance in preparing claims and paperwork. These small steps can help you tap into funding you may not have known was even possible.
Insurance for Government Employees and Public Sector Families
If you or your spouse works for the central or state government, you may have access to specialized insurance schemes like CGHS (Central Government Health Scheme), ESI (Employees’ State Insurance), or state-level health programs.
These often provide better coverage for pediatric prosthetics compared to private insurance.
Under CGHS or ESI, parents can request partial or full reimbursement for prosthetic fittings, especially if the limb difference is linked to a recognized medical condition.
Some schemes also allow annual reviews or renewals, which means families can request new prosthetic devices as their child grows.
The key to accessing this support is submitting a formal application through the correct department. You’ll usually need a recommendation from a registered medical officer or hospital tied to the insurance network.
Once approved, reimbursements are typically sent directly to the parent or credited to the provider if purchased through an approved vendor.
This process may take time, but many families have received substantial help through these public insurance systems.
If you’re part of a government or public sector job, it’s worth checking with your HR department or administrative officer to understand the process better.
Group Insurance and NGO Partnerships
In recent years, a few group health plans and non-profit health initiatives have started to include prosthetic support in their benefits. These are often tied to schools, community organizations, or NGOs that work in the disability space.
They may offer smaller policies or grants specifically designed to support assistive devices for children with physical differences.
These group insurance programs often focus on families from low-income or underserved areas. Instead of complex policies, they may offer simpler reimbursement models or direct subsidies.
For example, a child enrolled in a disability-focused education program may be eligible for a prosthetic fitting supported by the school’s health fund or partnered NGO.
Some larger insurance companies have also started teaming up with non-profits to run pilot programs in inclusive healthcare.
While these partnerships are still growing, they show promise in making prosthetic care more accessible across different regions and income levels.
If you’re connected with a local support group, community health worker, or disability rights NGO, ask whether they are aware of any insurance or subsidy program.
These connections often know where to look for funding that may not be widely advertised.
Challenges Families May Face with Insurance
Despite all the possibilities, getting insurance to cover pediatric prosthetics is not always smooth. Some policies still see prosthetics as luxury items rather than essential medical tools.
Others may have outdated limits that don’t match the real cost of modern prosthetics. This can lead to low reimbursement or delays in approval.
Another challenge is that many policies are designed with adults in mind. They don’t account for how quickly a child outgrows their prosthetic or how often repairs and upgrades are needed.
This is why families must often apply for new claims every year or every time the device needs replacement.
It can also be difficult to find insurance agents or policy documents that explain prosthetic coverage in clear language. This makes it harder for families to plan ahead or know what to expect.
But with growing awareness and advocacy, these systems are slowly changing. Parents who ask questions, stay informed, and push for clear answers are helping shape a system that works better for children with limb differences.
Government Schemes and Financial Aid for Pediatric Prosthetic Care
Why Government Support Matters
For many families in India, private insurance is either not available or does not cover the full cost of a pediatric prosthetic.
And even when insurance does offer some help, it often falls short of covering repeat fittings, repairs, or updated devices as the child grows. This is where government support plays a vital role.
India has several schemes at both central and state levels that provide financial aid for assistive devices like prosthetic arms and hands.
These programs are designed to help children with disabilities lead active, independent lives, regardless of their financial background. While the process of applying may take time, the support provided can be life-changing.
Understanding how these schemes work—and where to begin—can open doors to assistance that many families don’t even realize exists.
The ADIP Scheme: A Central Lifeline for Prosthetic Support
The most well-known government program for assistive devices in India is the Assistance to Disabled Persons for Purchase/Fitting of Aids and Appliances (ADIP) scheme.
This is run by the Ministry of Social Justice and Empowerment and provides free or subsidized prosthetics to eligible individuals, including children.
The ADIP scheme supports children with congenital limb differences or those who have lost a limb due to illness or accidents.
To qualify, the family must meet specific income criteria, and the child must have a disability certificate issued by a government-recognized medical authority.
Once eligibility is confirmed, children can receive prosthetic hands or arms, along with services like fittings, follow-ups, and minor repairs.
The devices are often provided through registered institutions or NGO partners, including well-known organizations like ALIMCO (Artificial Limbs Manufacturing Corporation of India).
Parents applying under the ADIP scheme should gather basic documents, such as proof of income, address, disability certificate, and Aadhaar card.
Many local hospitals or district disability offices also assist with submitting applications and scheduling fitting camps.
These camps are held across India throughout the year, especially in rural and underserved areas.
If there isn’t a scheduled camp nearby, families can also visit designated centers and apply directly.
ADIP not only reduces the cost burden—it often removes it entirely. This makes it one of the most important tools for families who may not have insurance or savings set aside for prosthetic care.
State-Level Disability Welfare Programs
In addition to national programs like ADIP, many Indian states have their own disability welfare departments that provide grants or devices to children in need.
These programs vary by region, but they often work alongside central schemes to extend reach.
For example, states like Tamil Nadu, Maharashtra, Gujarat, and Kerala have active state disability boards that fund prosthetic services for children.
Some offer annual grants, while others organize local camps where children are measured and fitted on-site. These programs may also cover transport costs, follow-up care, and repairs.
To access state-level aid, parents can approach the district disability officer or the local office of the Social Welfare Department.
In many cases, government hospitals serve as the starting point for evaluation and referrals.
Because the process and requirements vary, it helps to speak directly with the local health office or community health worker.
They often know about upcoming camps, application deadlines, or special drives that may not be widely advertised.
These state-level programs are especially helpful in areas where families have difficulty traveling or where private prosthetic services are limited.
Educational and Welfare Boards for Children with Disabilities
Another area of financial support comes through education-linked welfare boards. Children with limb differences who are enrolled in government schools or disability-inclusive learning centers may qualify for support beyond academics.
Some school boards provide aid for assistive devices, transport, or daily needs as part of broader inclusion efforts. These may not be widely publicized, but they often exist as part of district or state-level disability inclusion programs.
In certain areas, school principals or teachers can assist parents in identifying these options and connecting with the right offices.
For example, if a child has difficulty carrying books or writing due to an upper limb difference, schools may recommend a prosthetic solution and support the child’s application for financial assistance.
In some cases, the school itself may receive funding that can be directed toward a child’s specific needs.
This support may not always cover a full prosthetic device, but it can reduce the cost burden for the family or assist with extra accessories or modifications.
As India continues to push for inclusive education, these overlapping systems of support are slowly becoming more structured.
Staying in touch with teachers and school administrators can help parents identify these pathways early on.
Role of Panchayats, Local Health Workers, and Village Clinics
In rural India, families often feel cut off from larger government systems. But small support channels are often closer than they seem.
Local governance bodies like panchayats and village health centers sometimes play a role in connecting families to aid.
In some districts, community health workers or anganwadi staff have been trained to identify children with physical disabilities and help their families apply for medical support.
These workers may also receive updates on upcoming prosthetic camps or new aid programs introduced by the district.
Involving panchayat leaders or local NGOs can also speed up paperwork, increase visibility, and reduce the time it takes to access help.
These local support systems act as bridges—helping rural families reach the larger state and central services available to them.
This community-driven approach works best when parents are proactive in asking questions, visiting local clinics regularly, and keeping copies of all important documents ready.
What to Expect from Financial Aid
One of the most common concerns families have is what financial aid will actually cover. In most government-funded prosthetic programs, the aid covers basic devices that meet safety and functionality standards.
These devices are often mechanical or body-powered prosthetics—durable and functional, though less advanced than custom-designed bionic hands.
That said, these devices are often enough to support important tasks like grasping, lifting, or holding objects. For many children, this is the first step toward confidence and independence.
As they grow and show increased adaptability, families can explore further upgrades or custom options.
Some programs also allow for repeat fittings after a certain period, especially for children under 18.
Growth-based changes are taken into account, which means you can apply again for a larger device or a new fitting every year or two.
While cosmetic customization or AI-enhanced features may not be included under most free aid programs, the support still covers the core function needed to help a child regain daily movement.
For many families, this foundation is enough to begin their journey—and often leads to further support down the road.

Non-Governmental Support and CSR Programs for Pediatric Prosthetic Costs
Where Community Support Steps In
While insurance and government schemes play a major role in helping families manage prosthetic costs, they don’t always meet every need. Children grow fast. Devices break.
Some families may not qualify for subsidies, or they may face delays that hold up treatment. This is where non-governmental support steps in.
Across India, there are dozens of organizations—ranging from small community trusts to national non-profits—that offer help to families of children with limb differences. These groups fill in the gaps.
They often cover what traditional systems cannot, such as travel expenses, advanced prosthetic components, or emotional support services that make the entire experience smoother for parents and children alike.
Many of these organizations were founded by people who understand the struggles firsthand—parents, doctors, therapists, or disability advocates who saw what was missing and decided to do something about it.
That’s why the support they offer is not just financial. It’s often deeply personal, designed around real-life challenges families face when navigating pediatric prosthetic care.
These groups don’t always advertise widely, but they’re there. And with a little digging, they can become strong allies on your child’s journey.
Foundations and Trusts Focused on Disability Inclusion
Several Indian foundations specifically support children with disabilities, including those in need of prosthetic care.
These organizations typically run programs that offer direct financial support, organize free prosthetic fitting camps, or sponsor specific cases through donations from the public or corporate partners.
Some work independently, while others collaborate with medical institutions, prosthetic providers, and rehabilitation centers to streamline the support process.
Depending on the foundation, the support might come in the form of a free device, a grant, or even ongoing care over several years.
To apply, families usually need to provide a basic income statement, the child’s medical report, and a recommendation from a registered professional—often a prosthetist or pediatrician.
Most of these applications are reviewed on a case-by-case basis, and the outcome depends on availability of funds, need level, and timing.
While many of these foundations work quietly, a growing number now offer online applications and publish success stories to raise awareness.
Families are encouraged to reach out directly or speak with local clinics or therapists, who often know which groups are currently accepting applications.
Being open about your situation and asking for help is the first step toward discovering support you may not even know exists.
Corporate Social Responsibility (CSR) and Industry-Led Initiatives
One of the fastest-growing sources of support for pediatric prosthetic care is Corporate Social Responsibility (CSR). As part of their social impact efforts, many Indian companies are now funding healthcare initiatives for children with disabilities.
These CSR programs are usually run in partnership with NGOs, hospitals, or prosthetic developers.
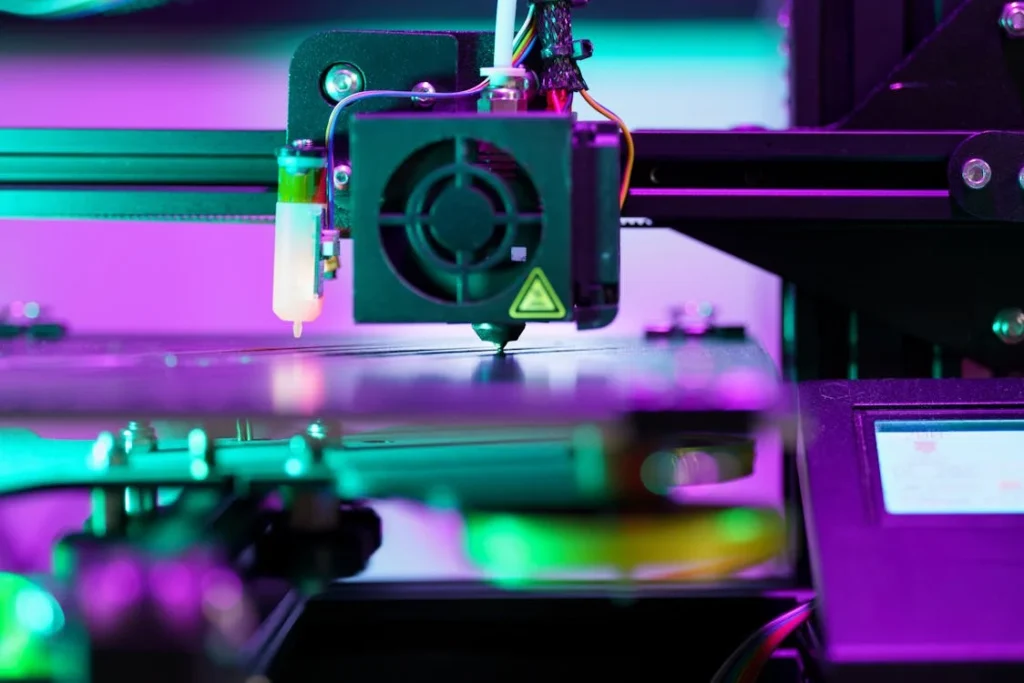
Unlike some government schemes, CSR programs often focus on innovation. This means they may fund more advanced devices, offer custom solutions, or support pilot projects using new technologies like 3D printing or AI-based systems.
This is particularly helpful for children who need more than a basic mechanical prosthetic or who live in areas with limited access to advanced care.
CSR funding is typically directed toward specific campaigns or areas—such as mobility aids for rural children, prosthetics for accident survivors, or technology-enabled learning tools for kids with limb differences.
Families don’t always apply to companies directly, but rather through a partner organization or clinic involved in the program.
Sometimes, these programs are announced through social media, community newsletters, or local health workers. Other times, parents learn about them during medical evaluations or rehab sessions.
Staying in touch with local networks—schools, clinics, and online support groups—can help you find out when such opportunities open.
Companies that support prosthetic care through CSR often do so quietly. But their contributions make a big difference, especially when traditional routes fall short.
Crowdfunding as a Bridge When Options Are Limited
For some families, formal funding channels may not be fast or flexible enough. In these cases, crowdfunding becomes a powerful tool.
Platforms like Milaap, Ketto, and ImpactGuru allow families to share their child’s story, explain their need for a prosthetic device, and raise money directly from the public.
Many families are surprised at how quickly strangers step forward to help, especially when the story is shared with honesty and clarity.
Photos, doctor’s notes, and updates on the child’s progress help build trust and encourage donations.
Crowdfunding is especially helpful for needs that aren’t covered by government aid—such as a second or third fitting in a single year, specialized rehab, or upgrades to a more advanced device.
While it requires effort to set up and promote, it gives families control over the timeline and the message.
Some prosthetic providers also assist with setting up campaigns or spreading the word through their networks. It’s not a guaranteed source of funding, but for many, it becomes the missing piece that makes timely care possible.
Even after the campaign ends, crowdfunding often connects families to long-term supporters, local charities, or future funding sources that were previously unknown.
Peer Networks and Social Media Communities
Sometimes, the best financial help begins with the right advice. Online support groups, parenting communities, and social media forums dedicated to limb difference and prosthetic care can be valuable resources for discovering hidden sources of support.
Parents often share where they found help, which NGO supported them, or what school offered a grant. These networks aren’t formal, but they are powerful.
They save time, guide families toward trusted sources, and provide emotional encouragement that makes a hard journey easier.
In many cities, informal WhatsApp or Facebook groups bring together parents, therapists, and care providers who exchange tips on where to apply, how to write a good application, or what documents are needed.
This kind of community knowledge is hard to find in official brochures or websites. But it can lead you straight to support you might otherwise miss.
When families help each other, they build a shared ecosystem of care that goes beyond money.
They pass on experience, give real-world advice, and remind each other that they’re not alone in this journey.

Planning for Long-Term Pediatric Prosthetic Costs
The True Cost Goes Beyond the First Device
For many parents, the first time their child receives a prosthetic hand or arm is emotional and life-changing. But once the initial fitting is complete, the journey is far from over.
Children grow, develop new abilities, change schools, and explore different interests. As these changes happen, the prosthetic must also evolve.
One of the biggest misunderstandings around pediatric prosthetics is the idea that the cost is one-time. In reality, families can expect to go through multiple fittings, adjustments, repairs, and even replacements during the child’s growing years.
Each stage of development brings new requirements—what worked at age four may not suit a seven-year-old who now needs more dexterity or grip strength.
Because of this, it’s helpful to think of pediatric prosthetics not as a product, but as an ongoing service.
Planning ahead for the long-term financial side of care can make a big difference in managing stress and staying prepared.
Growth, Wear and Tear, and Device Upgrades
Children outgrow their prosthetics just like they outgrow clothes or shoes. On average, a child may need a new prosthetic socket or size adjustment every 12 to 18 months, depending on their growth rate.
If the device includes moving parts, those too may need tightening, lubrication, or replacement over time due to regular use.
For more advanced prosthetics with electronics or sensors, software updates and battery replacements may also be necessary.
These updates are not always free. In many cases, families need to pay service fees or part replacement costs that were not included in the original price.
Children also use their devices in active, unpredictable ways. Falls, knocks, and spills can all cause minor damage.
And because children are still learning how to use the device correctly, they may press too hard, twist it the wrong way, or misuse parts without realizing it. This increases the need for occasional repairs or reinforcement.
Understanding that these adjustments are part of the process—not failures—helps families plan with more confidence.
Instead of being surprised by these extra costs, they can set aside small amounts each month or year to be ready when the time comes.
Planning Around Key Milestones
One useful approach is to plan prosthetic costs around major developmental milestones. These moments—such as entering school, starting sports, or reaching adolescence—often trigger new needs for the prosthetic itself.
For example, a child entering formal schooling may need a more functional device for writing or art. A child joining a sports club might require better grip or more flexible joints.
Rather than reacting when these needs arise, planning ahead can make the transition smoother. If you know your child will likely need a more advanced prosthetic next year, you can begin looking into funding options months in advance.
This avoids rushed decisions or financial strain when the change is finally needed.
It also helps to maintain regular check-ins with your prosthetist. Routine assessments can catch issues early and help schedule upgrades or replacements before the device becomes uncomfortable or non-functional.
Many providers offer maintenance packages or annual review plans that help spread out costs and ensure the device continues to meet the child’s changing needs.
Saving Strategies for Families
For families who do not have full insurance coverage or access to ongoing aid, creating a personal saving strategy is essential. Even small, regular savings can help ease the impact of future expenses.
Some parents open dedicated bank accounts just for medical or prosthetic care, while others use digital tools to track expenses and set reminders for checkups and payments.
It’s also worth keeping a simple notebook or digital record of past costs. This might include dates of fittings, repair costs, travel expenses, and related therapy sessions.
Over time, these records help identify patterns and average costs per year, which can guide future budgeting.
Some families also choose to combine saving with community fundraising. For instance, holding a small donation drive in your school or housing society during a prosthetic upgrade cycle can help raise part of the funds needed.
While this may not cover the full amount, it can fill gaps and reduce financial pressure.
In addition, families can look into medical loans, low-interest schemes, or microfinance options that are specifically structured for health-related needs.
While borrowing should always be done carefully, these tools can help manage larger, unexpected costs when other support is not available.
Preparing Emotionally for Ongoing Investment
It’s not just the financial cost that families need to plan for—there’s also the emotional energy that long-term prosthetic care requires.
Every new fitting, upgrade, or therapy session involves time, travel, adjustment, and patience. Sometimes, it also brings frustration—especially if a child has to relearn how to use a new device or if something breaks right after being fixed.
By accepting that this is a process—not a quick fix—parents can approach each stage with more flexibility.
Preparing for the emotional ups and downs can help reduce tension within the family and create a more supportive environment for the child.
When children see that their parents are calm and prepared, they also develop a more balanced attitude toward prosthetic care.
They begin to understand that devices can improve, grow, and change with them—and that’s a powerful mindset that helps with long-term adaptation.
Support groups, both online and local, can offer emotional guidance and practical tips from families who have walked the same path.
Talking openly with other parents, therapists, or care teams can turn a confusing journey into a shared, more manageable experience.

The Hidden Costs of Accessibility: Travel, Time, and Logistics in Prosthetic Care
The Journey to Care Isn’t Always Local
One of the challenges families face, especially outside major cities, is that pediatric prosthetic care is not always available nearby.
Specialized clinics, trained prosthetists, and advanced device fittings are often concentrated in metro regions or select hospitals. This means that many families must travel long distances just to access services.
While the prosthetic device might be partially or fully funded, the cost of reaching that care is often not. Travel, food, time off work, accommodation, and return visits quickly add up.
In some cases, families make multiple trips over weeks or months—first for evaluation, then for fitting, adjustments, and follow-ups.
For working parents or those with limited flexibility, this often means taking unpaid leave or finding temporary childcare for siblings.
These are costs that don’t show up on a receipt, but they affect a family’s budget and daily rhythm in real, lasting ways.
Even for families in urban areas, logistics like navigating city traffic with a child, arranging transport for wheelchair users, or managing long hospital wait times can be exhausting and expensive.
Understanding these hidden costs helps families plan more realistically and seek support where needed—not just for the device, but for the journey around it.
The Impact of Time on Family Life
Getting a prosthetic isn’t a one-day event. It’s a process that requires careful coordination between doctors, prosthetists, therapists, and the child.
Each of these appointments takes time—time that could otherwise be spent at work, school, or resting.
For many families, this creates a quiet kind of financial strain. One parent may have to reduce work hours or temporarily stop working altogether. In extended families, a grandparent or sibling might need to step in to help with daily responsibilities.
These changes can shift the dynamics at home and affect income, routines, and stress levels.
When visits to clinics stretch across several months—as they often do during the initial adaptation period—parents must balance care responsibilities with everything else life demands.
This hidden cost of time is often felt more deeply than the cost of the prosthetic itself.
That’s why having a realistic timeline, and support systems in place, is just as important as knowing the price tag of the device.
Preparing for the time needed allows families to stay steady and better manage expectations.
Access to Therapy and Training Services
Beyond the prosthetic fitting, children often need physical or occupational therapy to help them learn how to use the device confidently.
But these therapy services are not always included in the cost of the prosthetic, nor are they easily accessible in every town or district.
If the child is learning to use a bionic hand or a mechanical arm, they may require weeks of guided practice, ideally with a therapist who has experience in pediatric cases.
If that professional is located far away, families must factor in additional travel and session costs. In some cases, they may have to pay for private sessions if government or hospital-based slots are unavailable or overbooked.
Home-based therapy is an alternative in some regions, but not all families have access to it. When therapy is delayed, children may struggle to adapt, which can lead to reduced use of the prosthetic and emotional frustration.
That’s why therapy, although often overlooked, is one of the most important pieces of the prosthetic journey—and one of the more unpredictable expenses.
Families who plan ahead for therapy costs, or seek out rehabilitation centers that bundle therapy with prosthetic care, often experience smoother transitions and better outcomes.
Repairs, Maintenance, and Emergency Visits
Even the most well-designed prosthetic devices may need sudden attention. Children are active.
They run, jump, climb, and use their hands in spontaneous ways. A damaged strap, a loose fitting, or a software glitch can bring everything to a halt—especially if it affects a task the child relies on daily, like writing or playing.
When that happens, families may have to rush back to the clinic or provider. If it’s located far away, this means rearranging schedules, arranging transport, and sometimes missing school or work with very little notice.
These emergency trips are often not planned for financially or logistically. And because pediatric prosthetics must be adjusted carefully to match the child’s growth and comfort, quick fixes are not always possible on the spot.
Some clinics offer remote support or guidance, but for physical damage or alignment issues, an in-person visit is usually needed.
Planning for one or two emergency visits per year—financially and time-wise—can reduce stress and avoid delays in care.
Families can also ask their prosthetic provider about nearby service points or partner clinics for easier access when urgent help is needed.
The Emotional and Mental Load of Logistics
The logistical side of prosthetic care doesn’t just affect the calendar and wallet—it impacts mental energy too. Coordinating appointments, remembering follow-ups, chasing documents, and waiting in crowded clinics can be tiring for any parent.
Add to that the emotional weight of caring for a child who may be nervous, resistant, or uncomfortable, and it’s easy to see how overwhelming the journey can become.
This invisible cost of caregiving—called “care fatigue” by some professionals—can lead to burnout, missed appointments, or delayed follow-ups, even in well-intentioned families.
It can affect how consistently the child wears and uses the prosthetic, how well they adapt, and how supported they feel.
One way to ease this burden is to create a simple care schedule with clear reminders, notes from therapists, and key contacts in one place.
This can help reduce the mental juggling that comes with long-term care.
Families can also lean on support networks—siblings, neighbors, school counselors, or disability parent groups—to share tasks, gather advice, and stay emotionally grounded during more demanding phases of the journey.
How Digital Innovation Is Helping Lower the Cost of Pediatric Prosthetics
Rethinking the Way Prosthetics Are Made
Traditional prosthetic manufacturing is a labor-intensive process. It involves several steps—casting, molding, customizing, and assembling—all of which require skilled technicians and expensive materials.
This method, while proven, is often slow and costly. For pediatric users who outgrow their prosthetics quickly, the cycle repeats more frequently, driving up long-term expenses.
Digital innovation is now disrupting that model. Technologies like 3D printing, CAD design, and computer-based fitting simulations are reducing both production time and cost.
These tools allow for faster prototyping, lighter materials, and simpler processes, all while maintaining quality and function.
For example, instead of creating a full arm mold manually, a child’s limb can be scanned digitally, and a custom-fit prosthetic socket can be printed within days.
Adjustments that once took weeks can now be done in hours. This kind of speed and accuracy helps bring costs down for both providers and families.
As more clinics adopt digital fabrication techniques, we’re likely to see prosthetics that are not only more affordable but also easier to replace, repair, and personalize.
Remote Fittings and Virtual Assessments
One of the most promising innovations in pediatric prosthetic care is the move toward remote consultations and digital assessments. For families living far from major cities or prosthetic centers, this is a game changer.
In a typical scenario, a child might have to travel several times just for fitting sessions, measurements, and training. But with the rise of mobile scanning apps and video-based assessments, many of these steps can now be handled remotely.
Parents can send videos, photos, or even 3D scans from home. Prosthetists review the information, design the needed components, and schedule just one visit for final fitting and adjustment.
This model not only saves travel costs but also makes the process less disruptive for children. It also enables specialists to serve more families in a shorter amount of time, improving access without sacrificing care.
As these remote tools become more common, especially in India’s rural and semi-urban areas, they may significantly reduce the indirect costs associated with care—making the overall prosthetic journey more affordable and manageable.
Modular Designs That Grow with the Child
Another smart innovation that helps reduce costs is the use of modular prosthetic systems. These are prosthetics made up of interchangeable parts—sockets, joints, terminal devices—that can be swapped or upgraded without replacing the entire limb.
For children, this is especially useful. Instead of buying a whole new device every time they grow, families can simply replace a few parts. Some designs even include adjustable-length features that can be modified at home or during routine checkups.
This approach lowers material waste and repair time. It also makes advanced features more accessible. For example, a child might begin with a passive hand and later upgrade to a myoelectric terminal device, without needing to replace the entire setup.
When combined with digital manufacturing, modular designs make prosthetic care more flexible and cost-efficient—without compromising quality or performance.
Open-Source Designs and Collaborative Innovation
There’s also a growing movement of open-source prosthetic design communities around the world. These are groups of engineers, designers, and prosthetic users who share designs, tools, and ideas freely online.
The goal is to create high-quality, low-cost prosthetic solutions that anyone can use and adapt locally.
Many of these open-source designs focus on children. They are playful, colorful, and designed for ease of use.
Some have been developed by university students, community inventors, or small non-profits that believe assistive devices should be affordable for all.
In India, organizations and academic institutions have started adopting these designs, customizing them for local needs and using local materials to keep costs low.
When combined with 3D printing and local fabrication, open-source designs offer a new way for families to access prosthetics without relying on expensive, imported models.
These designs are not only budget-friendly, but they also promote independence and creativity.
Some children are even involved in choosing or modifying their own devices, which increases acceptance and daily use.
The Promise of AI-Driven Personalization at Scale
Artificial intelligence is often seen as a high-end feature. But when used correctly, it can help lower long-term costs.
AI-powered software can quickly analyze user data and suggest ideal settings, grip patterns, or adjustments—reducing the need for repeated in-person visits and trial-and-error fittings.
Over time, this data helps create smarter prosthetics that need fewer modifications.
Devices can begin to self-calibrate or notify parents when a part is wearing down, helping families stay ahead of costly breakdowns.
More importantly, AI tools can help scale prosthetic services. A small team of trained professionals can manage a larger group of users remotely, using software to guide each case and alert them to issues before they become serious.
This increases efficiency and keeps care affordable—even as demand grows.
As AI becomes more widely integrated into pediatric prosthetic systems, families may benefit from a model that feels both personalized and scalable, offering better value with fewer ongoing costs.
Conclusion
The cost of pediatric prosthetic care is about more than the device—it includes time, travel, therapy, and ongoing adjustments as children grow. While the expenses can seem overwhelming, families have more options than ever. From insurance policies and government schemes to community aid, CSR funding, and digital innovation, support exists in many forms.
Planning ahead, asking the right questions, and staying informed can make a real difference. As technology continues to evolve—bringing smarter, more affordable solutions—access to quality prosthetic care is becoming less of a privilege and more of a possibility for every child.
The journey is ongoing, but with the right knowledge and support, families can navigate it with confidence. The goal is not just to cover costs—it’s to empower children with the tools they need to move, play, learn, and live fully.



