
Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
For many clinicians, the surgery is only the first step. What happens after the operation
Cancer has a way of forcing hard choices. For doctors, one of the hardest is deciding between saving a limb or removing it to save a life. For patients, it’s a battle between hope and heartbreak — between the dream of keeping their own arm or leg, and the fear of losing it forever.
In oncology, especially in cases of bone and soft tissue cancers like osteosarcoma or Ewing’s sarcoma, this decision is never simple. Medical science today offers incredible tools to remove tumors while preserving limbs. Yet, sometimes, despite the best efforts, limb salvage may not be the safest or most practical option.
That’s where prosthetics come in — not as a last resort, but as a powerful path forward. Modern prosthetic limbs, especially advanced bionic hands and legs, give patients not just mobility but dignity, freedom, and confidence. They allow people to return to daily life, to work, and to the things they love.
This article explores that critical turning point: when doctors should pivot from limb salvage to amputation, and how prosthetics — particularly modern, affordable ones made in India — are transforming lives after cancer.
We’ll look closely at what really goes into the decision-making process, the emotional and medical factors at play, and how prosthetic technology has evolved to become an active part of cancer care rather than an afterthought.
Because sometimes, letting go of a limb is not giving up. It’s choosing to move forward — stronger, freer, and with new possibilities ahead.
Limb salvage surgery aims to remove the cancerous tumor while saving as much of the limb as possible. The idea is simple — eliminate the disease but preserve function, appearance, and emotional well-being.
In practice, though, it’s far from simple. Surgeons must remove the tumor with clean margins to prevent recurrence. That often means cutting close to major nerves, blood vessels, and muscles. Rebuilding what’s left requires complex reconstruction using bone grafts, metal implants, or donor tissue.
These surgeries can last several hours and need months of rehabilitation. While many patients recover mobility, some live with weakness, chronic pain, or limited motion. The risk of infection or non-healing bones is also real, especially when chemotherapy weakens the body.
Limb salvage is therefore not only a surgical decision — it’s a question of long-term quality of life.
There are moments when limb salvage, no matter how advanced the technology, may not be the best path. If the tumor wraps around critical blood vessels or nerves, removing it entirely without losing function becomes nearly impossible.
Sometimes, infection or radiation damage makes reconstruction unsafe. In other cases, repeated surgeries to preserve the limb can leave the patient physically and emotionally drained. For children, growth complications may make limb salvage less practical.
Doctors often balance these realities with one priority — giving the patient the highest chance of living a healthy, active life. If saving the limb threatens that goal, amputation may be the safer, more compassionate choice.
For any patient, hearing the word “amputation” is devastating. The fear of losing a limb feels like losing a part of identity. Many imagine a future filled with limitation, dependency, and stigma.
This emotional storm can be intense. Even families struggle with guilt — wondering if more could have been done to save the limb. That’s why it’s crucial for doctors, psychologists, and prosthetic experts to work together early in the process.
When patients are shown that life with a prosthetic can be active and fulfilling, the fear begins to fade. They start to see amputation not as an ending, but as a beginning of a different, but meaningful, chapter.
Not all cancers behave the same. Osteosarcoma, for example, tends to grow aggressively near the ends of long bones — like the femur or tibia. Ewing’s sarcoma can affect both bone and soft tissue.
If the tumor is localized and doesn’t invade major nerves or arteries, limb salvage may be possible. But if it spreads into critical structures, amputation ensures complete removal and reduces recurrence risks.
Tumor size also matters. Large tumors often mean extensive tissue removal, which can lead to poor limb function afterward. In such cases, amputation can actually lead to faster recovery and better long-term mobility when paired with a good prosthesis.
In many cancers, patients receive chemotherapy or radiation before surgery to shrink the tumor. When these treatments work well, limb salvage becomes more feasible. But if the tumor doesn’t respond, or new lesions appear, amputation might be the safer route.
Chemotherapy also affects healing. It weakens immunity and delays tissue repair, increasing infection risk after complex limb reconstruction. A clean, well-healed amputation stump is often easier to manage than a poorly healing salvaged limb.
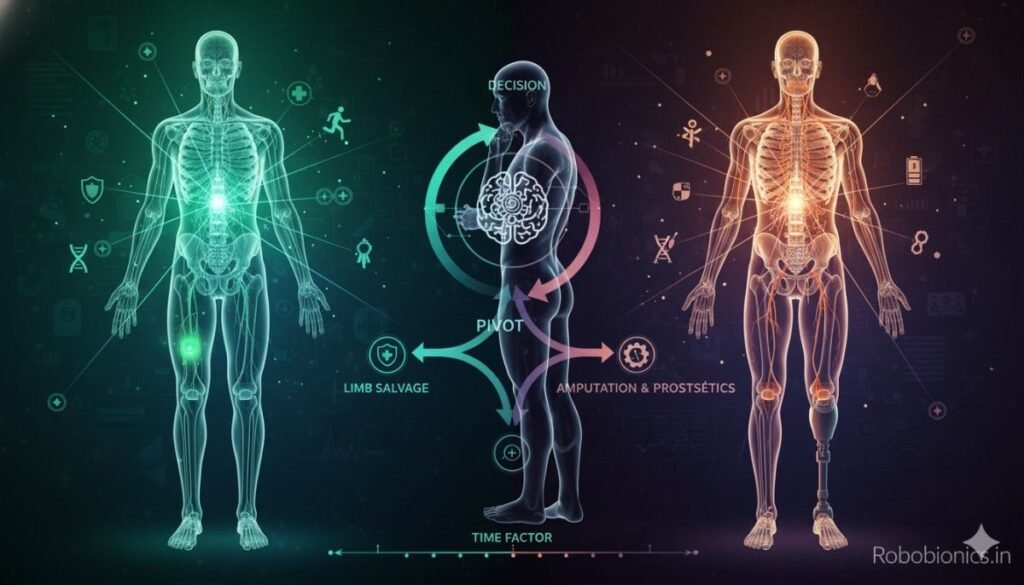
One key question every doctor must ask is: what kind of life will the patient have afterward?
A limb that looks preserved but can’t move, lift, or bear weight may not serve its purpose. The goal is not just to keep the limb, but to ensure independence. If an amputation followed by prosthetic fitting can provide better function, then it often becomes the logical — though emotionally harder — decision.
Medical readiness alone isn’t enough. Emotional readiness plays a major role. Some patients cope better when they feel informed, supported, and part of the decision-making process. Others need time and counseling to process the fear and loss.
Doctors who communicate openly and show examples of people living full lives with prosthetics help patients regain hope. The human mind is powerful — when patients believe they can recover, they almost always do better physically.
Sometimes, saving the limb at all costs leads to years of pain, repeated surgeries, and emotional exhaustion. Patients may lose faith in their recovery or live with constant discomfort.
At this point, doctors must ask — are we helping, or prolonging suffering?
When the functional outcome is low and the emotional cost is high, pivoting to prosthetics can give the patient a better chance at living freely again. Modern prosthetic limbs are designed for comfort, control, and confidence. They allow people to walk, lift, and even return to sports.
Infection, poor blood flow, or necrosis after limb salvage are warning signs. If these complications threaten overall health or risk spreading cancer, amputation becomes a life-saving measure.
Doctors who pivot early — rather than waiting for conditions to worsen — often help patients recover faster and with fewer long-term issues. The earlier the stump heals, the sooner prosthetic training can begin.
Thanks to technology, prosthetics today can often outperform reconstructed limbs in terms of functionality. A person fitted with a well-made prosthetic can regain up to 90% of normal activity, depending on the level of amputation.
Bionic hands, for example, can perform delicate tasks like picking up a coin, typing, or holding a glass. Powered legs can help users climb stairs, walk on uneven terrain, and even run.
If limb salvage limits a person to crutches or braces, but prosthetics can restore independence, the choice becomes clear.
A patient’s mindset can guide timing too. When someone expresses readiness to embrace prosthetics and rebuild their life, doctors can pivot confidently. The best outcomes come when decisions are made together — with empathy, not just clinical logic.
Prosthetic rehabilitation is a journey. The sooner it begins, the faster confidence and function return. Doctors who introduce prosthetic specialists early in treatment create smoother transitions and better emotional recovery.

The journey of prosthetics has been remarkable. What started as simple wooden pegs centuries ago has evolved into lightweight, sensor-driven limbs that move like natural extensions of the body.
In oncology, this progress means that losing a limb no longer equals losing independence. With innovations like myoelectric control — where muscles send natural signals to the prosthesis — users can perform everyday tasks almost intuitively.
Some prosthetic hands today even offer sensory feedback. This means users can feel pressure or texture, allowing more precise control when gripping objects.
Such technology transforms recovery. Instead of learning to “use a tool,” patients learn to “feel again.” The emotional benefit is huge — restoring a sense of wholeness that surgery alone can’t provide.
In India, imported bionic limbs often cost over ₹10 lakh, making them out of reach for most patients. This financial barrier has kept many from choosing prosthetics after amputation.
Companies like RoboBionics are changing that story. By manufacturing locally and focusing on affordability, they’ve made advanced bionic hands and arms available for as low as ₹2.15–3 lakh.
This accessibility means doctors can confidently recommend prosthetics without worrying about financial stress for patients.
Timing matters. The sooner a patient is fitted with a prosthetic after amputation, the faster they recover physically and emotionally. Early fitting helps prevent muscle atrophy, keeps balance intact, and reduces phantom limb pain.
When oncology teams coordinate with prosthetic specialists from the start, rehabilitation becomes part of the treatment plan, not an afterthought.
The first few weeks after amputation can feel like a blur. The patient is coping with physical pain, emotional loss, and uncertainty about the future. It’s natural to grieve — after all, it’s a major change.
But soon, a shift begins. With the right care and support, patients realize that life doesn’t end after losing a limb. In fact, it can restart in new and unexpected ways.
Doctors, physiotherapists, and prosthetic experts all play a vital role here. The moment they start treating the patient as capable — not broken — recovery becomes faster. Confidence builds when patients see what they can still do, not what they’ve lost.
Each small victory matters: sitting up unassisted, balancing, walking a few steps. These moments add up and fuel a sense of possibility.
No one recovers alone. Behind every successful comeback story is a team that believes in the patient’s strength.
Oncologists handle cancer treatment. Surgeons manage healing. Physiotherapists rebuild strength. Prosthetists fit and train patients to use their new limb. Psychologists help navigate the mental adjustment.
When all of them work together, outcomes are not just medically sound but emotionally empowering. The patient feels cared for as a whole person — not just as a medical case.
Hospitals that build such integrated teams see faster rehabilitation and better long-term satisfaction. Patients are more likely to return to school, work, and social life sooner.
Losing a limb is not only physical — it’s deeply emotional. Many patients describe a period of shock, denial, anger, and sadness before acceptance begins. This process mirrors grief in many ways.
Doctors who acknowledge this emotional journey create space for healing. Instead of rushing patients to “move on,” they guide them gently, reassuring them that feeling low is normal.
Support groups, therapy, and meeting other amputees who have adapted well can be life-changing. When patients see someone walking confidently with a prosthetic, hope returns almost instantly.
One of the most puzzling experiences after amputation is the feeling that the missing limb is still there. This is called “phantom limb sensation.”
It can range from mild tingling to painful cramps. Though unsettling, it’s not imaginary — the brain is simply adjusting to the new reality. Physical therapy, mirror therapy, and early prosthetic fitting often help ease these sensations.
When the brain begins to associate movement with the prosthetic instead of the lost limb, the confusion settles. Technology and training help the brain “rewire” itself to the new normal.
Rehabilitation is not just about learning to walk or move again — it’s about reclaiming life. It’s the bridge between surgery and independence.
Each patient’s journey is unique. Some learn quickly, while others need months of guided therapy. The focus is on improving balance, coordination, and muscle strength. More importantly, it’s about building confidence in using the prosthetic in daily life.
This process is deeply human. It’s filled with small milestones — learning to wear the prosthesis for longer hours, standing without fear, or performing daily tasks like eating, writing, or dressing.
Before a patient can use a prosthetic, the residual limb must heal properly. Once healed, therapists begin gentle exercises to strengthen the surrounding muscles.
These exercises prevent stiffness and prepare the body for prosthetic fitting. For myoelectric prosthetics, training also includes learning to control muscle signals.
In time, patients learn how different muscle movements correspond to different prosthetic actions — like opening or closing a bionic hand. It’s a process that takes patience but becomes second nature with practice.
Every stump is unique. A prosthetic that fits perfectly makes all the difference between frustration and freedom.
A poor fit can cause discomfort, bruising, or even infection. That’s why precision is everything. Modern prosthetic makers use 3D scanning and digital modeling to ensure each limb fits naturally, evenly distributing pressure and providing comfort.
The right socket design, padding, and alignment give users stability and confidence to move without hesitation. A well-fitted prosthesis doesn’t just feel comfortable — it becomes part of the body.
Once patients gain control and comfort, rehabilitation shifts toward everyday tasks.
For someone with a lower-limb prosthesis, it means walking indoors, climbing stairs, or walking on uneven ground. For upper-limb users, it means learning to cook, type, or hold a pen again.
The joy of being able to do simple tasks independently is often indescribable. It restores dignity, confidence, and the sense of “I can do it” — something no medicine can replace.
Beyond physical training, there are emotional turning points too. The first day walking outdoors, returning to work, shaking hands confidently — each one marks a victory.
Therapists celebrate these wins because they know they’re not small. They’re proof that life after amputation is not limited, only different.
Some patients even go on to become mentors, helping others who are newly amputated. This creates a powerful cycle of hope and healing.

Earlier, prosthetics were seen as simple aids — static devices that helped a person “manage.”
But today, thanks to bionic engineering, prosthetics have become intelligent extensions of the body. They respond to natural muscle signals, adjust grip strength, and even mimic natural motion.
For cancer survivors, this means they no longer have to settle for limited movement. They can return to driving, writing, cooking, or even sports.
Myoelectric technology has revolutionized how prosthetics function. It works by detecting tiny electrical signals generated by the muscles in the residual limb.
These signals are translated into movement — opening or closing a hand, bending a joint, or rotating a wrist. This allows the user to control their prosthesis intuitively, without buttons or external controls.
The result feels natural and fluid, restoring not just mobility but confidence. Patients report feeling more “whole” when they can use their prosthetic like a real limb.
One of the most exciting innovations in prosthetics is sensory feedback — a system that lets users feel pressure or vibration when touching objects.
This technology helps prevent accidental dropping or crushing of items. It also enhances precision during delicate tasks.
For patients who have undergone amputation due to cancer, this touch feedback often has deep emotional meaning. It reconnects them to the physical world in ways they thought were lost forever.
In India, prosthetic innovation is catching up rapidly. Startups like RoboBionics are making world-class prosthetics locally, reducing dependency on expensive imports.
Grippy™, their flagship bionic hand, is an example of how affordable doesn’t have to mean inferior. It’s powered, lightweight, and uses myoelectric signals for control.
Even more remarkable is its Sense of Touch™ technology — something once available only in high-end foreign devices. And yet, it’s priced between ₹2.15–3 lakh, putting it within reach for thousands of Indians.
This local manufacturing revolution means oncologists now have practical solutions to recommend. Instead of worrying about cost or availability, they can confidently discuss prosthetics as a natural next step in cancer care.
No two patients are the same — and no two prosthetics should be either.
Prosthetic specialists today customize everything: socket shape, weight balance, grip strength, even skin tone. For many users, seeing a prosthetic that matches their natural skin color or feels “like them” has deep emotional value.
It’s not vanity — it’s identity. Feeling complete again helps people reintegrate into society without stigma. The psychological boost this brings often speeds up physical recovery too.
Delaying prosthetic fitting can cause physical issues like muscle shrinking, poor posture, and imbalance. Emotionally, it can also reinforce dependency and reduce motivation.
Early intervention prevents these setbacks. When doctors and prosthetic experts collaborate soon after amputation, they ensure the patient stays active and positive.
Even a temporary training prosthesis can make a big difference in maintaining symmetry and coordination.
The human body adjusts quickly. If a patient goes months without a prosthetic, their body starts compensating — leaning to one side, overusing certain muscles, and developing strain.
An early prosthesis restores natural posture, making walking or movement easier. This balance translates into confidence, which feeds into every aspect of recovery.
Studies show that early prosthetic use can reduce phantom limb pain. When the brain starts linking motor signals to a new limb instead of the missing one, confusion decreases.
This neuroplastic adjustment makes recovery smoother and more comfortable. It’s not just about replacing what’s lost, but retraining the brain to accept what’s new.
Seeing a prosthetic limb — especially one that looks functional and lifelike — can completely change how a patient views their recovery.
Hope replaces fear. Motivation replaces despair. Early fitting helps patients focus on what’s ahead instead of what’s missing.
For doctors, this means fewer post-surgery mental health challenges and better long-term patient engagement.

In oncology, every decision carries emotional and ethical weight. Saving a life is always the priority — but how that life will be lived afterward matters just as much.
Doctors often find themselves walking a thin line between extending life and preserving its quality. A limb-sparing surgery might sound ideal, but if it leaves the patient in pain, dependent, or facing multiple revisions, the victory may feel hollow.
It takes honesty and courage to pivot from preservation to amputation. But the decision, when made at the right time, can transform the patient’s future rather than limit it.
Limb salvage surgery can sometimes become a goal in itself. The pressure to “save” a limb — from patients, families, or even medical peers — can overshadow broader considerations like function and emotional recovery.
A wise oncologist steps back and sees the entire picture:
Will this limb truly work after surgery?
Will it allow the patient to walk, hold, and live normally?
Will it let them return to their dreams?
If the answer to these questions is uncertain, introducing the idea of prosthetics early can prepare everyone for a smoother transition, both medically and mentally.
Tough decisions require gentle words. When doctors communicate clearly, compassionately, and without jargon, patients feel empowered rather than defeated.
The best conversations happen when doctors sit with patients, listen to their fears, and explain all possible outcomes — not in numbers, but in human terms.
Instead of saying “You may lose function,” say “You may not be able to lift your arm like before.”
Instead of saying “You’ll need rehabilitation,” say “You’ll learn to use your new arm step by step, and we’ll be with you all the way.”
Words can soften even the hardest realities. They can replace panic with understanding and help patients feel part of the decision, not victims of it.
Families carry their own emotional burden. They want to protect their loved one, often clinging to hope that the limb can still be saved. But sometimes, their hope delays acceptance.
Doctors who include families early in conversations make the process smoother. Showing them examples of prosthetic success stories can help them visualize a life beyond the surgery.
When everyone understands the bigger goal — a healthy, independent life — the focus naturally shifts from loss to recovery.
Doctors are trained to heal, to preserve, to fight for every inch of recovery. But there comes a moment when continuing to save a limb may cross into prolonging pain.
Recognizing that line is an act of wisdom, not defeat. It’s a shift from doing “everything possible” to doing “what’s best.”
An ethical approach balances the medical facts with compassion. It acknowledges that dignity and independence are part of healing too.
Shared decision-making puts patients at the center. It means giving them all the information they need — risks, benefits, alternatives — and letting them take part in the choice.
When doctors act as guides rather than directors, patients feel respected. They recover faster because they feel ownership of their treatment path.
This collaborative approach also builds trust. A patient who feels heard is far more likely to follow through with rehabilitation and embrace prosthetics with optimism.
False hope can be more damaging than bad news. When patients are led to believe that limb salvage guarantees a “normal” limb, they’re unprepared for the limitations that follow.
Real hope, on the other hand, is grounded in truth. It says, “You will walk again, but it might be with a prosthetic leg.”
It says, “You will hold your child again, even if it’s with a bionic hand.”
This kind of hope empowers rather than deceives. It builds resilience and helps patients see possibilities beyond the operation table.
Oncologists are not only surgeons or clinicians — they’re also emotional anchors. A patient often mirrors their doctor’s tone and energy. When a doctor speaks calmly, with confidence and warmth, it creates stability in moments of fear.
Small gestures — a reassuring hand, a smile, eye contact — go a long way. They humanize medicine.
Empathy doesn’t mean avoiding difficult truths; it means delivering them with compassion. When patients feel cared for, they trust the journey — even when it’s hard.
Not long ago, prosthetics were introduced only after all else failed. They were seen as a “backup plan.”
Today, that mindset is changing. Doctors are beginning to see prosthetics as part of the treatment pathway, not the end of it.
By involving prosthetic specialists early — even before amputation — oncologists can prepare patients better. They can plan surgical techniques that preserve optimal stump length and muscle control, improving later prosthetic use.
This integrated approach ensures that patients don’t just survive cancer — they thrive afterward.
Prosthetic specialists bring unique insights that surgeons may not always consider. They can advise on the best amputation levels for maximum functionality, recommend training timelines, and design personalized rehabilitation programs.
When oncologists and prosthetists collaborate, the outcome is smoother and faster recovery. It’s a partnership that merges medical science with human engineering.
Moreover, having a prosthetic expert in the discussion helps patients visualize life after surgery — reducing fear and creating excitement about recovery.
One of the hardest parts of amputation is the feeling of dependency. Patients worry about needing help for basic tasks. Prosthetics break that barrier.
Modern bionic limbs restore not just movement, but self-respect. When patients can hold a cup, write their name, or walk to the gate on their own, they rediscover confidence.
For many cancer survivors, the prosthetic becomes more than a device — it becomes a symbol of strength and rebirth.
In India, accessibility matters as much as technology. That’s why the emergence of affordable, high-quality prosthetics is so significant.
RoboBionics, for instance, manufactures 60 of 64 parts of its Grippy™ bionic hand locally. This focus on local innovation cuts costs without compromising quality.
It also ensures easy maintenance, faster support, and greater customization — all vital for patients rebuilding their lives after cancer.
The Grippy™ hand’s Sense of Touch™ technology and intuitive control bring global-level functionality to Indian users, at a fraction of the price.
This balance of affordability and excellence is helping oncologists confidently recommend prosthetic solutions to a broader range of patients.

It’s easy to talk about prosthetics in terms of sensors, motors, and materials. But behind every bionic limb is a story — of resilience, courage, and renewal.
For cancer survivors, that story often starts in fear and ends in freedom.
When they first see their prosthetic, they may hesitate. But once they wear it, move it, and feel it respond, something powerful happens — they reconnect with themselves.
This emotional transformation is what drives prosthetic innovation forward. It’s not about building machines; it’s about rebuilding lives.
Psychological rehabilitation is as important as physical recovery. Many survivors battle self-consciousness — wondering how others will perceive them.
Counseling, peer support, and exposure to positive stories can turn that anxiety into pride.
Some even begin to see their prosthetic as a badge of survival — proof that they fought and won. This mindset shift not only accelerates healing but inspires others around them.
Across India, survivors fitted with prosthetics are redefining what’s possible.
A young engineer in Pune returned to his job using a myoelectric hand after losing his arm to osteosarcoma.
A teenager in Kolkata resumed cycling with a below-knee prosthesis.
A teacher in Delhi now writes on the blackboard again, proudly demonstrating her Grippy™ hand to her students.
Each story sends a message: cancer may take a limb, but it can never take determination.
Sharing real success stories during consultations can change patient mindsets instantly. Seeing proof of recovery breaks fear and sparks belief.
Hospitals and oncology centers can partner with prosthetic makers like RoboBionics to organize awareness sessions and demos.
When patients see the prosthetic in action — feel its lightness, watch its precision — it becomes less of a medical device and more of a symbol of hope.
In India, the conversation around cancer is shifting. It’s no longer just about living — it’s about living well.
Survivorship means helping people return to the rhythm of life — work, relationships, hobbies, and dreams. Prosthetics play a major role in that return.
By integrating prosthetic care into oncology treatment plans, doctors are giving survivors tools to rebuild both body and spirit.
Government initiatives like Startup India and Make in India are supporting companies like RoboBionics in making advanced prosthetics accessible nationwide.
Partnerships with hospitals, rehabilitation centers, and NGOs are ensuring that even rural patients have access to cutting-edge prosthetic care.
This growing ecosystem marks the dawn of a new era — one where cancer survivorship in India includes not just remission, but restoration.
Many doctors still hesitate to recommend prosthetics early simply because they’re unfamiliar with the technology.
Workshops, CME programs, and hospital collaborations can bridge this gap. When oncologists see firsthand how modern prosthetics work, their approach to amputation decisions naturally evolves.
Education creates confidence — and confident doctors inspire confident patients.
The future of oncology will blend surgery, rehabilitation, and prosthetic integration seamlessly. The question will no longer be “Should we amputate?” but “How soon can we restore full function?”
Prosthetics are not the end of treatment — they’re the continuation of healing. They represent modern medicine’s promise not just to save lives, but to make those lives worth living.
Cancer changes lives in ways no one prepares for. But every choice — even the hardest ones — can lead to renewal.
When doctors pivot from limb salvage to prosthetics with clarity and compassion, they give patients something more than mobility. They give them freedom, self-respect, and the chance to dream again.
Modern prosthetics are not symbols of loss. They’re symbols of strength, science, and second chances.
As medicine and technology move forward, the message becomes clear — losing a limb does not mean losing life’s possibilities.
At RoboBionics, we see this truth every day. With every Grippy™ hand fitted, we see courage reborn, confidence restored, and lives rebuilt.
If you’re a doctor looking to understand how prosthetics can become part of your oncology care plan, or if you’re a patient wanting to explore what recovery could look like beyond surgery, we’re here to help.
Book a demo today at robobionics.in/bookdemo — and discover how technology and compassion together can give life a stronger, more hopeful touch.

For many clinicians, the surgery is only the first step. What happens after the operation

For trauma amputees, the journey does not begin at the prosthetic clinic. It begins much

Amputation after cancer is not just a surgical event. It is the end of one

When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.