
Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
For many clinicians, the surgery is only the first step. What happens after the operation

For most surgeons, the focus after an amputation ends when the wound closes. But for the patient, the real journey begins only then — the journey to walk, move, and live again.
In recent years, medicine has reimagined how recovery can work. The Enhanced Recovery After Surgery (ERAS) approach has changed everything from how we handle anesthesia to how fast patients sit up, eat, and return home. It’s a philosophy built around early mobility, multidisciplinary care, and patient empowerment — and it’s proving that recovery doesn’t have to be slow.
Now, this same principle is being applied to amputee care.
An ERAS-style pathway for amputees focuses on speeding up recovery from the operating room to the first prosthetic fit. It blends surgical precision, pain control, nutrition, and psychological care with early rehabilitation and pre-prosthetic training.
For doctors, it’s a new way to think about old challenges — cutting time to independence, reducing complications, and improving long-term outcomes.
In this article, we’ll explore how ERAS-style programs can transform amputation recovery, what physicians should include in their templates, and how early prosthetic integration changes the entire rehabilitation landscape.
Because when recovery begins the same day as surgery, the road back to living doesn’t have to wait.

Enhanced Recovery After Surgery, or ERAS, began as a surgical philosophy designed to help patients recover faster and safer. It combines evidence-based medical practices with patient education and early mobility to reduce stress on the body after surgery.
Instead of a traditional “rest until healed” approach, ERAS encourages controlled activity, proactive pain management, and multidisciplinary coordination from day one.
When adapted to amputee care, these principles can dramatically change how long it takes a patient to stand, move, and use their first prosthesis.
For decades, amputation recovery followed a linear model — surgery first, rest second, rehabilitation third. It was reactive, not proactive.
ERAS-style pathways flip this order. They integrate rehabilitation right into the surgical plan, preparing patients before and after amputation for mobility.
The result is less deconditioning, fewer complications, and faster prosthetic fitting.
When patients stay inactive after surgery, muscle mass declines rapidly. Circulation slows, lungs lose capacity, and healing becomes sluggish.
Early mobilization — even sitting upright or performing deep-breathing exercises — keeps these systems active. It reduces inflammation, boosts oxygen delivery, and keeps the body primed for recovery.
For amputees, this means better wound healing, stronger residual limbs, and a quicker path to prosthetic tolerance.
ERAS also emphasizes the mind. Patients who are educated, supported, and involved in their recovery tend to heal faster.
In amputation care, early engagement helps manage fear, depression, and phantom pain. It restores a sense of control, turning recovery from something done to the patient into something done with them.
Doctors who adopt this approach often find their patients more cooperative, confident, and resilient through every stage of rehabilitation.
ERAS begins before the first incision. Surgeons and physiatrists work together to educate the patient about the entire journey — not just the surgery.
Preoperative counseling focuses on what to expect, pain management options, and the importance of early motion afterward.
This preparation removes fear and builds trust. Patients enter the operating room informed and mentally prepared, which reduces postoperative anxiety and improves compliance later.
Nutrition, hydration, and metabolic stability are cornerstones of ERAS.
Doctors ensure that patients have adequate protein levels and controlled blood sugar to promote wound healing. Smoking cessation and physiotherapy may also be started preoperatively to improve lung and heart function.
These steps, though simple, drastically reduce post-surgical complications like infection, delayed healing, and respiratory distress.
During amputation, the ERAS mindset continues. Surgeons aim to preserve as much healthy tissue, muscle, and bone as possible while ensuring proper shaping of the residual limb.
They use nerve-handling techniques like targeted muscle reinnervation or regenerative peripheral nerve interfaces to minimize phantom pain later.
Soft-tissue management focuses on creating a smooth, well-padded limb that can tolerate early compression and eventual prosthetic fitting.
Every surgical decision — from incision design to closure — is made with future mobility in mind.
Effective pain management is a central ERAS principle. Instead of relying only on opioids, multimodal pain control is used — a combination of local anesthesia, nerve blocks, and non-opioid medications.
For amputees, this reduces both acute pain and the risk of chronic phantom pain. It also helps patients stay alert and mobile sooner, enabling faster participation in physiotherapy.
Good pain control sets the tone for recovery. A comfortable patient moves more, heals faster, and regains confidence earlier.
Traditionally, post-surgical patients were kept fasting for long periods. ERAS changes that.
As soon as medically safe, patients are allowed to resume fluids and soft diets. Early feeding supports gut health, boosts immunity, and maintains energy.
In amputee recovery, this nutritional balance fuels muscle repair and tissue regeneration — essential for pre-prosthetic preparation.
This period sets the rhythm for everything that follows. Under ERAS principles, doctors aim to mobilize patients — even in small ways — within hours of surgery.
That doesn’t mean walking right away. It may simply mean sitting up, flexing residual muscles, or doing deep-breathing and arm movements.
The goal is activation, not exertion. These early actions prevent lung complications, blood clots, and stiffness.
The residual limb is protected but not immobilized completely. Gentle positioning, compression, and limb elevation help reduce swelling while keeping tissues flexible.
Doctors and nurses check circulation and wound condition frequently. Proper bandaging and light compression help shape the limb for future prosthetic fitting.
These small interventions make socket design easier later and reduce healing delays.
Early pain management continues with a structured plan. Doctors use nerve blocks, local patches, or oral medication combinations to maintain consistent comfort levels.
Phantom limb sensations are addressed with reassurance, mirror therapy, and light massage when appropriate.
Addressing pain early prevents it from becoming chronic and makes patients more willing to move and engage in therapy.
Within the first two days, the psychological impact of limb loss starts to surface.
Physicians and counselors visit patients early to talk openly about what to expect and to normalize their emotions.
This proactive empathy helps patients begin acceptance and sets the stage for active participation in their own recovery.
In ERAS-style care, mental recovery begins right alongside physical healing.
Doctors, physiotherapists, nurses, and prosthetists conduct daily team rounds. They share updates, modify plans, and ensure every discipline supports the same recovery goal.
This coordination prevents overlap, reduces confusion, and reassures patients that everyone is aligned in helping them reach their first fit as soon as possible.
By the third or fourth day, most patients are ready for gentle mobilization.
Physicians and therapists assist them with sitting, transferring, and standing with aids. Even partial weight-bearing improves blood flow, mood, and confidence.
These early sessions are supervised carefully to avoid strain, but their psychological benefit is enormous. The patient starts to feel capable again.
Even while the residual limb heals, other muscle groups must stay active.
Therapists guide patients through gentle contractions of thigh, hip, or shoulder muscles depending on the amputation site.
These exercises prevent atrophy and help maintain strength in the sound limb — critical for future balance and prosthetic control.
Doctors introduce compression therapy early to manage swelling and prepare the residual limb for a snug prosthetic socket.
Elastic bandages or shrinker socks are applied in progressive stages, teaching the limb to adapt gradually to pressure.
A well-shaped, firm limb speeds up prosthetic casting and improves socket comfort later.
Even before fitting, doctors often introduce the patient to prosthetic models or training tools.
This visual exposure demystifies the process and helps patients imagine themselves using one.
When the time for fitting comes, it feels familiar rather than foreign — a psychological advantage that boosts compliance and optimism.

In ERAS-style amputee care, rehabilitation doesn’t start after discharge — it begins the moment the patient leaves the operating table.
The focus shifts from passive healing to active engagement. The body learns, adapts, and strengthens under medical supervision. The mind, too, starts to reconnect movement with purpose.
Every session, from breathing exercises to early limb mobilization, reinforces one message: you are already in recovery.
Physiatrists are the bridge between surgery and prosthetic readiness. They evaluate strength, endurance, and emotional stability before tailoring exercise intensity to each stage of healing.
Their collaboration with physiotherapists ensures the patient progresses safely — from seated motion to supported standing to walking trials once fitted.
By following ERAS principles, they don’t wait for perfection; they build momentum.
Therapists complement this by making every session meaningful. Each movement — even lifting the sound leg or flexing a hip muscle — serves a purpose in restoring normal biomechanics.
One of the strongest benefits of ERAS protocols is reduced hospital stay. Patients who follow structured pathways often go home days or weeks earlier than traditional timelines.
However, going home doesn’t mean recovery stops.
Physicians provide detailed home exercise routines, nutrition advice, and follow-up schedules. For those ready, pre-prosthetic exercises continue through tele-rehabilitation — a growing tool in India’s expanding digital health network.
Early discharge paired with continued monitoring ensures progress remains steady without unnecessary inpatient costs.
One common challenge in traditional amputee recovery is deconditioning — the rapid decline in strength and endurance caused by inactivity.
ERAS solves this by keeping patients active throughout the recovery cycle. Even simple tasks like sitting upright, repositioning in bed, or engaging in daily hygiene contribute to maintaining cardiovascular health.
The philosophy is simple: every small effort prevents big setbacks.
Posture is often overlooked in early recovery. Yet, for amputees, correct alignment is critical to preventing back pain and uneven gait later.
Physicians and therapists use mirror feedback, core stabilization drills, and light balance exercises to train posture early.
This not only improves symmetry but also builds awareness — helping the patient adapt naturally to their new body mechanics before prosthetic fitting begins.
For lower-limb amputees, ERAS programs introduce gait simulation even before the prosthesis arrives.
Therapists use partial weight-bearing systems, parallel bars, or virtual motion simulations to mimic walking. This helps the brain establish the rhythm and confidence needed for real prosthetic use.
By the time the device is fitted, the neuromuscular pathways are already active, and the patient feels prepared rather than overwhelmed.
Nutrition remains a constant theme throughout the ERAS pathway.
Protein intake supports muscle repair, vitamins promote skin integrity, and hydration maintains tissue elasticity. Physicians emphasize high-quality calories rather than high volume — food that nourishes healing.
Dietitians often collaborate closely with surgeons and physiatrists to personalize plans for each patient’s needs and metabolic rate.
Food, in this sense, becomes part of the therapy.
ERAS-style programs rely on structured, time-bound milestones that guide both doctors and patients.
A typical pathway may define readiness checkpoints — day three for mobilization, week two for residual limb conditioning, week six for socket evaluation.
These timelines act as flexible templates that can be adjusted depending on wound healing, emotional state, and overall fitness.
The clarity of these timelines keeps both doctors and patients motivated and focused on measurable progress.
Before the first prosthetic fit, physicians ensure that the patient is medically stable.
They check cardiovascular endurance, skin healing, and absence of infection. They also evaluate medication impact, ensuring no drugs interfere with muscle control or alertness.
ERAS emphasizes proactive monitoring. By identifying issues early, doctors avoid delays and setbacks that can derail rehabilitation momentum.
Pain control remains a daily focus. Physicians track both physical and phantom pain, adjusting medication and therapy accordingly.
They use mirror therapy, graded imagery, and desensitization techniques to retrain the nervous system to interpret sensation correctly.
When pain is controlled early and consistently, patients engage more fully with movement and regain trust in their own bodies.
Physiatrists perform periodic evaluations of muscle tone and joint flexibility.
They look for tightness, contractures, or imbalances that could affect prosthetic alignment.
By maintaining a proactive schedule of assessments, they can intervene before stiffness becomes a barrier.
Strong, mobile joints translate directly into smoother prosthetic control and longer device comfort.
Physical recovery is incomplete without emotional readiness.
Physicians assess mood, confidence, and motivation before prosthetic introduction. Counseling sessions and peer support networks often become part of this stage.
When patients believe they are ready, they are more likely to succeed in early adaptation.
A calm, confident mind makes learning complex physical skills easier — an insight ERAS practitioners understand deeply.
Before the fitting, doctors often arrange sessions with prosthetists to explain the device — how it works, how it’s worn, and what to expect during training.
This education builds curiosity instead of fear. It also helps set realistic goals for the first days of use.
The ERAS approach turns anticipation into preparation. When the prosthesis arrives, it feels like the next logical step, not an intimidating unknown.
Many Indian hospitals still operate within traditional postoperative frameworks, where rehabilitation begins weeks after discharge.
ERAS challenges this by proving that early, structured recovery is not only safe but superior.
The shift begins with education — for both medical teams and patients. Surgeons, physiatrists, and nurses learn to coordinate closely, communicate frequently, and document progress collectively.
Once this culture takes root, patients experience shorter hospital stays, fewer complications, and better long-term satisfaction.
Implementing ERAS requires training. Hospitals that partner with prosthetic manufacturers like RoboBionics receive hands-on support to develop care templates suited to their infrastructure.
Workshops and modules teach clinicians how to integrate pain control, wound management, and early mobilization protocols in a synchronized manner.
Through real-world data, these centers learn how small adjustments — like early limb wrapping or bedside EMG training — can shorten rehabilitation timelines by weeks.
In a country as vast as India, accessibility is often the biggest challenge. ERAS models leverage digital tools to bridge this gap.
Tele-rehabilitation platforms allow physicians to track recovery remotely, guide exercises, and adjust protocols without requiring frequent hospital visits.
For rural or semi-urban patients, this approach makes early rehabilitation feasible, consistent, and affordable.
It’s a blend of modern medicine and practical innovation — one that fits India’s evolving healthcare landscape perfectly.
Hospitals working with integrated prosthetic centers — such as those affiliated with RoboBionics — see the fastest results.
By involving prosthetists from the early postoperative phase, measurements, assessments, and limb shaping can start weeks before final fitting.
This early collaboration ensures that the transition from surgery to prosthetic training is seamless. Patients no longer face long waiting periods between healing and movement.
Instead, recovery feels like a continuous, empowering journey.
Education sits at the core of ERAS success.
Hospitals implementing these pathways provide informational booklets, videos, and counseling sessions that explain every phase — from wound care to nutrition to prosthetic expectations.
When patients understand why each step matters, compliance soars.
They begin to take ownership of their recovery, reducing dependence on external motivation and creating long-term engagement with therapy.
RoboBionics’ products, including the Grippy™ Bionic Hand and our upcoming lower-limb prosthetic systems, are built for early training.
Their lightweight, intuitive design allows physicians to introduce functional training sooner without overwhelming the patient.
Our devices respond naturally to muscle signals, mirroring the principles of ERAS — efficiency, comfort, and patient empowerment through movement.
We collaborate directly with hospitals and clinics across India to help design ERAS-inspired recovery templates.
Our medical liaisons assist physicians in building time-based care models, from surgery to first fit, using real clinical data from ongoing partnerships.
This hands-on collaboration ensures our technology and the physician’s expertise work together in perfect sync.
Our ongoing data collection from partner institutions has revealed clear patterns: early prosthetic preparation under ERAS principles leads to measurable gains.
Patients participating in structured early recovery programs reach functional independence faster, show fewer wound complications, and report higher satisfaction scores.
Every case reinforces what we’ve always known — timing and teamwork define success.
By manufacturing 60 of 64 prosthetic components in India, RoboBionics makes advanced rehabilitation pathways feasible for hospitals of all sizes.
Affordability removes barriers to early intervention. When doctors don’t have to worry about costs, they can prescribe what’s best for the patient — not what’s cheapest.
That freedom changes lives.

The ERAS mindset begins before the patient ever enters the operating room. Physicians start by creating a roadmap — a clear, step-by-step outline of what will happen before, during, and after surgery.
This plan includes nutritional optimization, patient counseling, and preoperative exercise or “pre-hab” routines.
By the time surgery arrives, the patient is informed, emotionally grounded, and physically prepared.
Doctors who follow this model often find that early clarity eliminates uncertainty and reduces post-surgical anxiety — both major factors in recovery speed.
An ERAS-style amputation is not simply about removing a limb; it’s about preparing a foundation for movement.
Surgeons adopt tissue-sparing techniques, create muscle stabilization flaps, and use nerve management methods like targeted muscle reinnervation.
Every incision is planned with a future prosthesis in mind — how it will fit, how it will bear pressure, and how it will move.
This alignment of surgical technique with future function embodies the ERAS principle of thinking beyond the moment. It’s surgery in service of independence.
Immediately after surgery, the ERAS pathway emphasizes controlled, early mobilization.
Doctors and physiatrists coordinate to ensure patients begin light motion within 24 to 48 hours, focusing on breathing exercises, limb elevation, and gentle isometric contractions.
Each movement restores circulation and signals to the body that healing is active, not passive.
By integrating these activities into daily rounds, physicians turn recovery into a rhythm — predictable, progressive, and empowering.
Pain, both real and phantom, can disrupt progress if not addressed early. ERAS-style care uses a blend of nerve blocks, non-opioid medications, and cognitive behavioral support to manage discomfort.
Mirror therapy and virtual visualization techniques are introduced early to help the brain adjust to new sensory input.
Doctors regularly evaluate pain levels to fine-tune medication and therapy.
This proactive management not only improves comfort but also prevents the development of chronic phantom pain — one of the greatest barriers to prosthetic success.
ERAS reminds doctors that healing is biochemical before it’s mechanical.
Nutritional support — rich in protein, vitamins, and hydration — becomes part of the prescription.
Dietitians and physicians work together to ensure patients maintain metabolic balance and tissue repair potential.
For diabetic amputees especially, blood sugar control during this stage is critical to avoid infection and delayed healing.
The difference between a slow recovery and a strong one often begins on the plate.
In the traditional model, psychological care was optional. In ERAS, it is mandatory.
Physicians coordinate counseling sessions and group support early in recovery. Patients are encouraged to share fears, celebrate milestones, and visualize the life they are working toward.
Doctors lead this tone of empathy — reminding patients that losing a limb doesn’t mean losing identity.
When hope is nurtured alongside healing, resilience becomes a clinical outcome.
The first step in bringing ERAS-style amputee care to hospitals is forming a multidisciplinary team.
This team includes surgeons, physiatrists, prosthetists, physical therapists, anesthesiologists, dietitians, and psychologists.
Regular meetings and clearly defined communication channels ensure everyone stays aligned with the recovery timeline.
When every specialist shares the same mission — early mobility and faster prosthetic readiness — patients experience consistent, coordinated care.
Implementing ERAS doesn’t require expensive infrastructure; it requires thoughtful workflow design.
Hospitals can start by adjusting ward routines — earlier physiotherapy sessions, proactive nutritional monitoring, and pain assessments during morning rounds.
Simple changes, like allowing patients to sit up within hours after surgery or providing bedside exercise tools, can make measurable differences.
These small interventions create a culture of movement and participation, turning recovery from passive observation into active collaboration.
Many Indian hospitals are beginning to add pre-habilitation to their ERAS pathways.
Before amputation, patients are enrolled in short conditioning programs that build upper-body strength, improve circulation, and teach breathing control.
This not only prepares the body but also helps the patient mentally accept and plan for rehabilitation.
When pre-hab and ERAS combine, recovery time can shrink dramatically — sometimes by weeks.
For hospitals, data is key to sustaining change. Physicians can track recovery using functional metrics such as the Timed Up and Go test (TUG), the Six-Minute Walk Test (6MWT), and the Amputee Mobility Predictor (AMPnoPRO).
Comparing pre- and post-ERAS outcomes helps institutions validate improvements and refine protocols further.
When results show shorter hospital stays, fewer complications, and faster prosthetic readiness, administrators gain powerful evidence to expand the program system-wide.
RoboBionics actively collaborates with hospitals to train doctors, nurses, and therapists in ERAS-aligned amputee care.
Workshops and case studies are conducted to demonstrate how each phase — from anesthesia to early prosthetic training — connects to the larger goal of enhanced recovery.
Through continuous learning, medical teams gain confidence in integrating advanced technology and early rehabilitation methods safely.
This shared knowledge culture ensures consistency, no matter where the patient begins their journey.

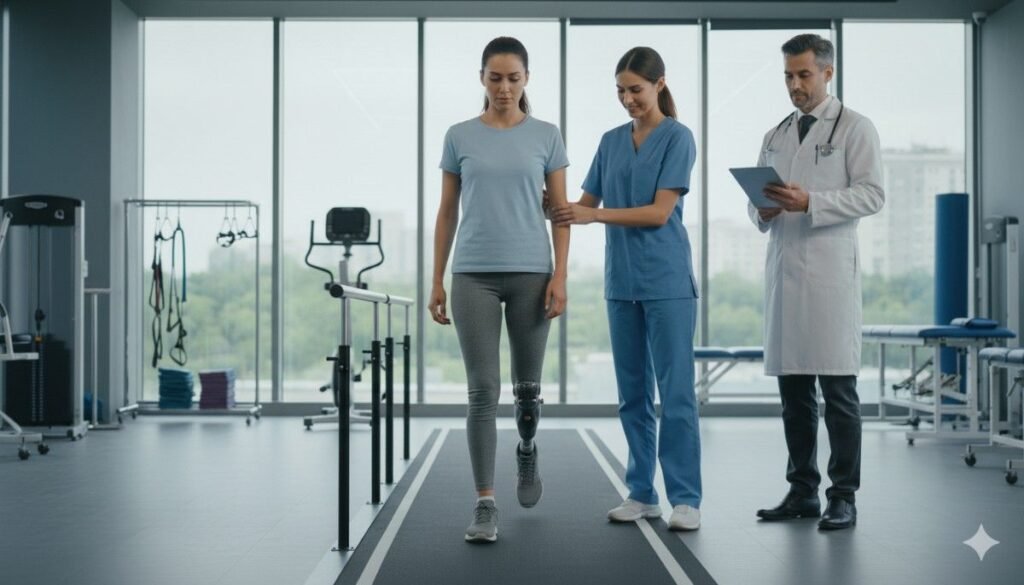
A 32-year-old construction worker lost his leg in a workplace accident. In the past, his recovery might have taken six months before he could walk again.
But with ERAS principles, his doctor initiated movement within 48 hours of surgery. Gentle hip and core exercises were followed by early compression therapy.
By week three, he was practicing partial weight-bearing with a walker. By week six, his first prosthetic was fitted.
When asked what helped most, he said simply, “My doctors never let me feel like I was waiting. I was always moving.”
A 45-year-old music teacher underwent a below-elbow amputation after a severe infection.
Her ERAS pathway included early myoelectric training and counseling sessions during her hospital stay.
By the time her Grippy™ Bionic Hand was fitted, she already had full muscle control. Within months, she was teaching piano again — the same students who once came to visit her in the ward were now learning from her return.
Her story became a hospital case study in the power of preparation.
At 70, most people would expect a long recovery. But for one diabetic amputee treated under an ERAS framework in Pune, independence returned faster than anyone imagined.
His surgeon introduced bedside exercises immediately after surgery. The team emphasized nutrition, emotional counseling, and compression shaping.
With consistent guidance, he took his first steps with his prosthesis at the two-month mark.
Today, he walks his terrace every morning, greeting neighbors with a smile that says, “I got here early — and that made all the difference.”
What started as an experimental adaptation is now becoming a movement.
As more hospitals see the results — shorter recovery times, lower costs, and happier patients — ERAS-style pathways are being written into clinical guidelines for amputation care.
In time, this model may become the national standard, where every amputation automatically includes early rehabilitation planning and prosthetic integration.
It’s a transformation not just in medicine but in mindset.
Public hospitals, rehabilitation centers, and private prosthetic manufacturers like RoboBionics are beginning to collaborate in powerful new ways.
By sharing knowledge, resources, and technology, they are bridging the gap between surgery and social reintegration.
This partnership-driven model ensures that even patients in smaller towns can benefit from world-class recovery protocols once reserved for elite institutions.
Advances in prosthetic design are perfectly aligned with ERAS principles.
Devices like the Grippy™ Bionic Hand allow for early interaction, real-time feedback, and gradual training without strain.
Lower-limb systems under development at RoboBionics focus on reducing energy expenditure and enhancing balance — ideal for early mobility training.
As devices become smarter and lighter, doctors can safely integrate them into rehabilitation earlier than ever before.
The next step in scaling ERAS for amputees is education.
Medical schools and residency programs can begin incorporating ERAS principles into their surgical and rehabilitation curriculums.
RoboBionics supports this initiative through academic collaborations and data sharing, helping students learn from real outcomes.
When young doctors enter practice already trained in enhanced recovery methods, early mobility becomes the default, not the exception.

RoboBionics isn’t just building prosthetics; we’re building systems of recovery that help doctors deliver faster results.
By offering physician tools, pre-hab templates, and ERAS-compatible prosthetic solutions, we make it easier to translate theory into practice.
When surgeons, physiatrists, and therapists work with us, they gain access to the complete ecosystem — devices, training, and ongoing support — to bring early recovery to life.
For patients, early fitting isn’t just about walking or grasping again; it’s about rediscovering confidence.
Each milestone, from lifting a cup to taking a first step, becomes a declaration of possibility.
That emotional transformation is what drives everything we do — creating technology that listens to the human body and responds with care.
India is uniquely positioned to lead the world in affordable, accessible, high-quality prosthetic care.
With locally manufactured components, skilled medical professionals, and growing ERAS adoption, our country has everything it needs to redefine recovery for millions.
RoboBionics is proud to be part of this movement — combining compassion, innovation, and Indian ingenuity to make early independence a national standard.
The ERAS pathway is more than a clinical protocol. It’s a philosophy — one that believes in starting early, moving often, and healing completely.
For doctors, it’s a framework that turns waiting into progress. For patients, it’s proof that recovery doesn’t have to be slow or uncertain.
When physicians lead with coordination, preparation, and compassion, the line between surgery and rehabilitation disappears. Recovery becomes one continuous journey — from operating room to early prosthetic, from loss to renewal.
At RoboBionics, we stand with every doctor who dares to move early. Because every day saved is a day returned to life.
If you’re a surgeon, physiatrist, or rehabilitation specialist ready to build ERAS-style pathways in your hospital, let’s do it together.
Schedule a demo or connect with our clinical team at robobionics.in/bookdemo.
The future of prosthetic recovery in India is not just fast — it’s thoughtful, dignified, and already within reach.

For many clinicians, the surgery is only the first step. What happens after the operation
For trauma amputees, the journey does not begin at the prosthetic clinic. It begins much
Amputation after cancer is not just a surgical event. It is the end of one

When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.