The road to recovery after an amputation isn’t just about healing wounds. It’s about rebuilding strength, relearning movement, and preparing both the body and mind for something entirely new. That journey doesn’t start the day you get your prosthetic. It starts much earlier—with pre-prosthetic therapy.
One of the biggest questions people face after amputation is when to begin this therapy. Start too early, and you might risk slowing down healing. Start too late, and you may face stiffness, weakness, or socket fit problems down the line. So timing is everything.

The Critical Healing Phase Right After Surgery
What Happens in the First Few Days
In the first few days after an amputation surgery, the main goal is simple: allow the body to rest and begin healing. This stage is delicate. The residual limb is still fresh from surgery.
There may be pain, swelling, and a bandage or dressing that needs to stay clean and dry. Your body is also adjusting to the sudden change—physically and emotionally.
During this phase, you’ll spend time in bed or a hospital chair. Movement is limited, but that doesn’t mean it’s completely off-limits. Nurses and therapists might help you change positions, encourage gentle breathing exercises, or even move your other limbs to keep blood flowing.
But for the surgical site, the main focus is protection. The limb needs time to close and form a solid base before therapy can begin.
This phase usually lasts about one to two weeks, depending on your health, how the surgery went, and whether there were any complications. It’s important not to rush.
If you push too soon, it can cause the wound to reopen or slow healing. But that doesn’t mean you’re just waiting around either.
Why Rest Doesn’t Mean Inactivity
Even while your residual limb is healing, there are small things that can be done to prepare for therapy later. Simple actions like sitting up in bed, doing light leg lifts with your non-affected side, or gently moving your arms can keep other parts of your body active.
These small movements matter. They help you avoid stiffness, maintain circulation, and reduce the risk of complications like blood clots or lung infections.
You might also begin learning how to care for your residual limb. Nurses will show you how to keep it clean, how to avoid pressure injuries, and how to monitor for signs of infection.
This kind of care is part of therapy, too. It builds awareness and confidence, so you’re not caught off guard when more active therapy begins.
When Pain and Swelling Start to Fade
Once the swelling begins to go down and the surgical pain is more under control, the door to pre-prosthetic therapy begins to open.
This window usually comes around week two or three, but it can vary widely. Some people heal faster, while others may need more time due to diabetes, poor circulation, or infections.
This is where your care team starts watching more closely. Is the wound closed and free of drainage? Is the pain manageable without heavy medication? Is the limb forming a consistent shape, or is it still changing a lot? These questions help decide when to safely begin therapy.
At this stage, you might start to notice your residual limb feeling more like a part of your body and less like a wound. That’s a good sign. It means your body is beginning to accept the change and is almost ready to start building strength.
The Therapist’s First Visit
Your first visit with a physical or occupational therapist may happen while you’re still in the hospital. It won’t be intense. It’s more of a conversation, combined with a gentle check of how you’re moving.
The therapist might ask about your pain, your daily routine, and how you’re feeling emotionally.
They may guide you through basic breathing and posture exercises. These help set the stage for better movement later on. They’ll also teach you how to position your body correctly—how to rest your limb without causing contractures (permanent stiffness), and how to avoid letting muscles weaken just because they’re not being used.
This early guidance is a part of therapy, even if it doesn’t feel like traditional exercise yet. It’s the first real step toward getting your body and mind ready for the prosthetic journey ahead.
Healing Is Not Just Physical
It’s important to recognize that during this healing phase, a lot is happening emotionally too. You may be dealing with fear, grief, or anxiety. You may be wondering what comes next or how life will change. These feelings are completely normal.
Many pre-prosthetic therapy programs include emotional support as part of the process. You might speak to a counselor or be introduced to a peer support group.
These resources help you cope, and that emotional strength plays a big role in how ready you’ll be for more active therapy later.
When you feel emotionally supported, you’re more likely to follow your rehab plan, stay motivated, and trust the process. This trust makes everything smoother, especially when it’s time to start working harder with your limb.

Starting Gentle Pre-Prosthetic Therapy: The Early Movement Phase
When Movement Becomes Safe and Productive
Once your surgical wound has closed and pain is under better control, your body is finally ready for more structured movement.
This is when the real foundation of pre-prosthetic therapy begins. The goal here is not just to move for the sake of movement, but to prepare your limb and your body for life with a prosthesis.
This stage usually begins two to three weeks after surgery. Some people may start sooner, some later, depending on their unique situation. What matters is not the date, but the signs. If your wound is healing well, if there’s no infection, and if your doctor or therapist feels you’re ready, then it’s time to begin.
At this point, your therapy will include basic exercises to keep your joints flexible and your muscles active. These aren’t high-impact or strenuous moves. Instead, they’re gentle, repeated actions that help prevent your body from becoming stiff or weak.
You might start with small leg raises, slow hip bridges, or stretching your arms and shoulders to avoid tightness.
Even these simple moves make a big difference. They protect you from muscle loss and help your body maintain balance.
Later, when you’re fitted for your prosthesis, this balance is what will help you walk smoother, move confidently, and feel less strain on the socket.
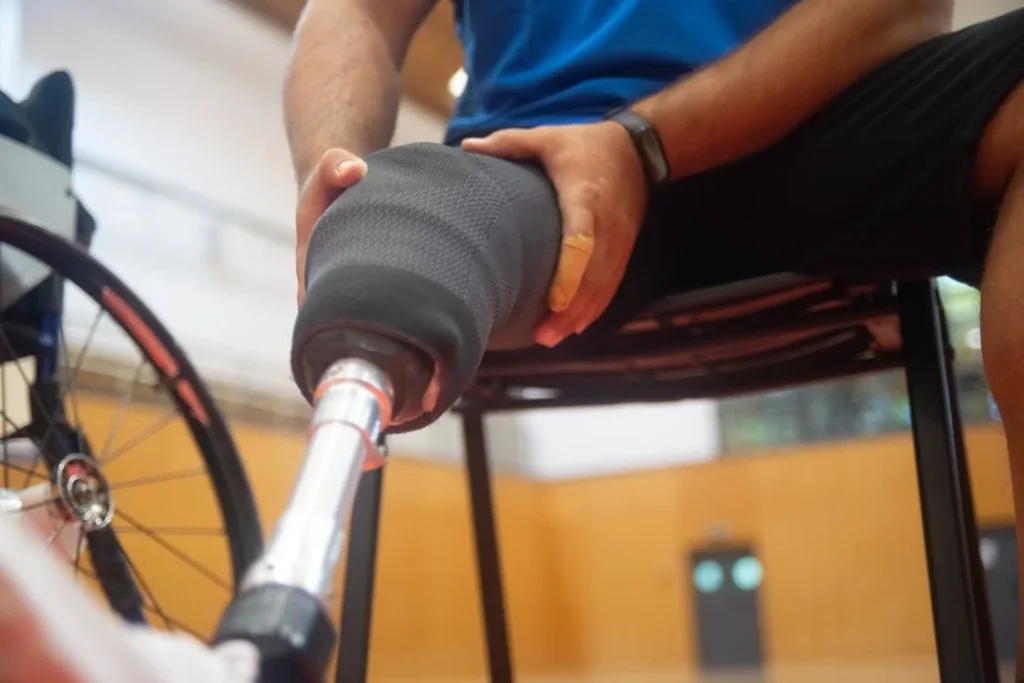
Shaping the Residual Limb for a Better Fit
One of the most important goals during this phase is helping your residual limb form the right shape. After surgery, the limb is often swollen, soft, or uneven.
To get the best socket fit later, it needs to become more tapered and firm. That means gently guiding the limb into the right form through a combination of compression and controlled movement.
Your therapist may introduce shrinkers—elastic garments that gently squeeze the limb to reduce swelling and help it form a smooth, cone-like shape.
These shrinkers are worn for most of the day and removed for cleaning and skin checks. They help reduce fluid buildup and promote healthy tissue shaping.
You might also start using limb elevation, mild massage, or even early weight-bearing exercises on soft surfaces. All of this is aimed at preparing the limb to sit comfortably inside a future socket.
The better this shaping is done now, the fewer problems you’ll face with socket fit later.
A well-shaped limb reduces pressure points, keeps the prosthetic stable, and helps avoid painful rubbing or blisters. It also improves how the prosthesis moves with your body, giving you more freedom and less frustration.
Strengthening the Muscles That Will Carry You Forward
When you lose a limb, the muscles near the site lose their normal job. Without regular use, they shrink and weaken quickly.
But these muscles are still important. They help stabilize your body and guide your movement once a prosthesis is in place.
Pre-prosthetic therapy focuses on keeping these muscles active. You’ll be guided through simple strength-building exercises that don’t stress the healing area.
These could include squeezing a towel with your thighs, pressing your residual limb gently into a pillow, or raising your hips slightly off the bed to activate your core.
You may not feel like you’re doing much at first, but these exercises are incredibly important. They train the muscles that will help you stand, walk, and move with less effort.
They also help with posture, balance, and endurance—all things that will affect how your socket fits and feels.
Even five or ten minutes of targeted exercises each day can make a noticeable difference. And as your strength improves, your therapist will slowly increase the intensity or duration to match your progress.
Learning to Use the Rest of Your Body in New Ways
When one limb is lost, the rest of your body has to adjust. You may need to shift your balance differently, use your arms more, or build stronger hips and core muscles to make up for the change.
This doesn’t just help with walking—it helps with everyday things like getting out of bed, transferring from a chair, or using crutches or walkers.
Your therapist will teach you how to use your body efficiently and safely. These movement patterns are designed to prevent injury, avoid bad habits, and prepare you for future prosthetic use.
For instance, you’ll learn how to keep your hips level, how to avoid leaning too far forward or backward, and how to take pressure off your healing limb while staying active.
This stage is also where you begin to build endurance. At first, even a few minutes of movement can leave you feeling tired. That’s normal.
But with consistency, your energy levels will improve, and your body will start feeling stronger each week.
This energy and strength are key to managing your prosthetic successfully later on. A tired, untrained body will always struggle with socket comfort.
But a body that’s been gradually prepared will adapt faster and perform better.
Building Toward Prosthetic Readiness: The Strength and Coordination Phase
Transitioning from Gentle Movement to Focused Training
After a few weeks of light exercises and limb shaping, most people reach a point where their body can handle more structured therapy. The wound is healed, swelling is mostly gone, and muscles have regained some strength.
This is where pre-prosthetic therapy becomes more focused. You’re no longer just moving to stay active—you’re training your body to support a prosthetic limb.
This stage often starts around four to six weeks post-surgery, though it can begin earlier or later depending on how recovery is going.
The key sign that it’s time to move forward is when you can complete daily activities with less effort, your pain is manageable, and your residual limb is taking shape.
Your therapy now becomes more dynamic. Movements become a bit faster, more coordinated, and more goal-driven. You’ll practice posture, balance, and endurance, all with the aim of preparing your body for weight-bearing and motion with a prosthetic limb.
This part of therapy often feels like training—not just healing—and it marks a major milestone in your journey.
Training Your Body to Work in Harmony
Using a prosthetic successfully depends on how well the rest of your body cooperates.
Every movement you make with a prosthesis requires muscle coordination from other areas: your hips, core, shoulders, and even your neck. If one part is off-balance, the socket won’t sit right. It may twist, rub, or even slip.
In this stage of therapy, your exercises will begin focusing on synchronization. That means learning how to control multiple muscle groups at the same time.
For lower limb amputees, this could include standing on one leg while keeping your hips level and back straight.
For upper limb users, it might mean lifting your shoulder while stabilizing your core and rotating the torso together.
You may not notice how much coordination this takes at first. But your therapist will spot it—and help correct it. These subtle changes are what make a prosthesis feel natural instead of forced.
By training these patterns now, you’ll avoid bad habits that cause poor alignment and socket pressure later. A body that moves in balance allows the socket to work with you, not against you.
Core Strength Makes All the Difference
Many new amputees underestimate how important the core muscles are. These muscles—located around your stomach, back, and pelvis—are what hold your body stable as you move. Without strong core support, every step, lift, or turn becomes harder.
Core training becomes a top priority in this phase. You’ll work on exercises like seated balance, modified planks, or standing with support while activating your abdominal muscles.
These activities improve your posture, reduce strain on the socket, and help you avoid common issues like leaning or limping.
Even better, strong core muscles make prosthetic training safer. They protect your back, improve endurance, and make movements more efficient.
This reduces fatigue, which is one of the biggest causes of socket discomfort. The less energy you waste on staying upright, the more you can use to move confidently.
Core strength also helps with pain control. A balanced body distributes weight more evenly, which reduces pressure points inside the socket.
That means less skin irritation, fewer adjustments, and a longer, more comfortable day on your feet—or with a prosthetic arm in motion.
Preparing Mentally for Prosthetic Use
As the body strengthens, the mind must prepare as well. Many people feel excited about getting their prosthesis, but they also carry fear, doubt, or unrealistic expectations.
That’s completely normal. The idea of using an artificial limb can feel overwhelming at first. There are questions about comfort, control, and how it will affect daily life.
This stage of therapy is where mental readiness becomes just as important as physical. Therapists might guide you through visualizing movements with your future prosthesis.
They’ll talk to you about what to expect—how the prosthetic will feel, how to take care of it, and how to handle common challenges like pressure or skin soreness.
Some programs also introduce mock prosthetics or simulation tools. These allow you to practice using your muscles and balancing weight as if you already had the limb in place.
The goal isn’t perfection—it’s preparation. The more familiar you are with how things will work, the easier it becomes to adapt.
You may also meet with other prosthetic users, attend a support group, or watch educational videos that show real people using their devices.
These moments help build emotional resilience. They remind you that you’re not alone, and that success comes with time and effort—not instant results.
Laying the Groundwork for Socket Comfort
This phase is where all your earlier effort begins to show. A well-shaped limb, strong muscles, good posture, and mental clarity all combine to support a smoother prosthetic fitting.
When your body and mind are aligned, the socket fits better and feels better.
You’ll also start learning how to check your skin, report pressure areas, and understand how socket adjustments work. Knowing when something is wrong—and speaking up about it—is a skill that often begins here.
By the time you’re ready for your first fitting, your body won’t be surprised. It will be ready. And that readiness is the best protection against long-term socket fit issues.

Recognizing Readiness: The Transition to Prosthetic Fitting
Signs You’re Ready for the Next Step
Reaching the point where you’re ready for a prosthetic fitting is a major milestone. But how do you know you’re truly ready? It’s not just about how the residual limb looks—it’s about how your entire body has prepared to support a new way of living.
One of the clearest signs is that your residual limb has settled into a consistent shape. It’s no longer changing size from one week to the next. The swelling has gone down, and the tissue feels firm, not soft or spongy.
This kind of stability makes it much easier to get an accurate socket measurement. If you attempt fitting too early, while the limb is still changing, you may end up with a socket that becomes too loose or tight in just a few weeks.
Strength is another key factor. You should be able to move around with relative ease using your walker, crutches, or wheelchair. If your balance is better, your posture more upright, and you can complete basic movements without strain, it’s a good sign you’re physically prepared for the prosthesis.
Emotionally, you’ll know you’re ready when you feel more curious than afraid. You might still have questions or concerns, but they don’t stop you from moving forward.
You trust your body more. You trust your team more. And you’re willing to take the next step.
The Therapist’s Role in Determining Readiness
Even if you feel eager to begin using your prosthesis, your therapist will make the final call on when to start the fitting process.
This decision is based on more than just healing. It includes physical readiness, safety, muscle control, and mental preparedness.
Your therapist will assess how well you can control your core, how stable your gait is (even with aids), and how strong your residual limb is against gentle pressure.
They’ll also check your range of motion. If joints are too stiff, it could affect how the socket aligns, leading to long-term comfort problems.
Your skin will also be closely inspected. Any open areas, signs of infection, or pressure injuries need to be fully healed before socket fitting begins.
Even a small sore can become a big issue once you’re wearing a prosthetic all day.
You’ll likely go through a final round of tailored exercises, positioning techniques, and skin conditioning. These final steps in therapy are designed to get you over that last hill—turning preparation into performance.
What Happens Right Before Your First Fitting
In the days or weeks before your fitting, your therapist will start to shift the focus of therapy. Instead of just working on movement, you’ll now be guided through specific positioning techniques that align your body for the prosthesis.
For lower limb amputees, this means practicing how to evenly distribute your weight through your hips and spine. You may start standing exercises with the help of bars or rails, slowly building confidence in your balance.
You’ll learn how to step properly, how to shift weight, and how to stay relaxed in your stance. These details are vital. If your body is stiff or tense, the socket won’t align properly.
For upper limb users, the focus shifts toward limb control, shoulder flexibility, and small, deliberate movements that mimic tasks you’ll eventually do with your prosthetic hand or arm.
The aim is to develop smooth, intentional motion—not jerky, rushed actions that can throw off socket positioning.
You may also be shown videos or photos of how sockets are fitted, what to expect in the clinic, and how to prepare your limb for the fitting day.
You’ll be told to keep your shrinker on, continue skin checks, and avoid anything that might cause new irritation.
This period feels like a countdown. It’s a mix of excitement, nerves, and anticipation. But by now, you’ve done the hard work. Your body has been shaped, your muscles have been strengthened, and your confidence has grown.
You’re not just getting a prosthetic—you’re about to make it a part of your life.
Why This Stage Sets the Tone for Long-Term Success
The weeks leading up to prosthetic fitting are some of the most important in your rehab journey. It’s the bridge between preparation and performance.
If everything has been done right—if therapy has been consistent, if the body is balanced, if the mind is steady—then the socket fit will be smoother, the prosthetic will feel more natural, and adjustments will be easier.
That doesn’t mean everything will be perfect. Most people still go through a short period of trial and error with their new device.
But they recover faster, they adapt more easily, and they stay engaged. And that makes all the difference.
In contrast, when therapy is skipped or rushed, socket fitting becomes a struggle. The limb may be too swollen, the skin too fragile, or the person too weak to wear the device for more than a few minutes at a time.
This leads to discomfort, discouragement, and sometimes abandonment of the prosthesis altogether.
That’s why every day of pre-prosthetic therapy matters. It’s not just about getting ready for a fitting. It’s about making that fitting count. It’s about giving the prosthetic the best chance to succeed—because it’s joining a body that’s truly ready for it.

How Lifestyle and Home Environment Influence Therapy Readiness
Recovery Starts at Home, Not Just in Clinics
It’s easy to focus only on hospital rooms and rehab centers when thinking about recovery, but the truth is that most of your healing happens at home. That space—your living room, bedroom, bathroom—is where your body rebuilds and your habits take shape.
The way your home is set up, how accessible it is, and how your day-to-day life is structured can directly impact how early and how successfully you begin pre-prosthetic therapy.
If your home is cluttered, has stairs, or lacks grab bars and support furniture, basic movement becomes harder. You might avoid getting up or doing exercises because it feels unsafe or exhausting.
That leads to delays in strengthening your body, and with every delay, socket fitting becomes a little more complicated.
In contrast, a home that supports safe movement—clear pathways, a chair with arms, a firm bed, a bathroom setup for easy access—can speed up your therapy progress. It makes it easier to follow your therapist’s instructions and practice your daily exercises.
When you can move more freely and confidently at home, you’re more likely to start and maintain therapy without setbacks.
Support Systems Affect Motivation and Consistency
Another key factor is who’s around you. Are there family members or friends who can help you move, prepare meals, or encourage you to keep going on tough days? Or are you mostly alone, trying to figure things out as they come?
People with strong support systems often start pre-prosthetic therapy earlier and stick with it longer. That’s because they feel safer, more motivated, and less overwhelmed.
They have someone to hold them accountable, celebrate progress, or simply be there when pain or frustration shows up.
Even having one reliable person who checks in, helps manage medication, or reminds you to wear your shrinker can make a huge difference in how ready you are for therapy.
On the other hand, if support is limited, therapists may delay certain activities until they’re sure it’s safe to proceed without supervision.
This doesn’t mean progress is impossible without help. It just means planning is even more important. Your therapy team might suggest setting alarms, keeping journals, or doing teletherapy check-ins more often to stay on track.
Your Daily Routine Tells a Bigger Story
Before starting pre-prosthetic therapy, therapists often ask questions that go beyond the medical chart. They want to know what a normal day looks like.
Do you wake up early or late? Do you spend most of the day in bed, or are you moving around your home? Do you cook, clean, or care for someone else?
These questions help therapists understand your current routine—and whether it supports or delays healing. For example, if your day is very inactive, it might mean your muscles are weakening faster than expected.
If you’re trying to do too much too soon—like standing for long periods without balance training—it might put strain on your healing limb or back.
Therapists use this information to build a more realistic plan for pre-prosthetic therapy. Instead of a generic exercise schedule, they align therapy goals with your lifestyle.
If your goal is to walk to the kitchen on your own, that becomes part of your daily rehab. If your goal is to carry your child or use a keyboard again, those actions are broken down into small therapy tasks.
This connection between real life and therapy builds purpose. And when your therapy has purpose, you’re more likely to stick with it, and more likely to enter your prosthetic fitting phase with strength and confidence.
Cultural and Emotional Comfort Matter More Than You Think
Another unique factor is your emotional environment. That includes your beliefs, values, and even the cultural messages you’ve grown up with around disability, independence, and body image.
These invisible forces can influence how open or hesitant you feel about starting therapy.
In some homes, there might be pressure to “tough it out” without much support. In others, there might be fear of becoming too dependent on medical devices or hesitation about asking for help.
These attitudes can delay therapy, even if the body is ready. People may skip appointments, avoid exercises, or dismiss early discomfort, thinking it’s normal or shameful to complain.
Pre-prosthetic therapy works best when these emotional blocks are addressed early. That’s why therapists sometimes bring in counselors or peer mentors who’ve been through the same journey.
When you see others who’ve overcome similar obstacles, it becomes easier to believe that healing and strength are possible—and worth the effort.
It also helps when therapy conversations are honest and sensitive. Not every day is positive, and not every movement feels like progress.
When your therapy team acknowledges that and supports you without judgment, you’re more likely to speak up, stay involved, and ask for what you need.

The Hidden Power of Nutrition and Hydration in Pre-Prosthetic Therapy
Your Body Can’t Rebuild on an Empty Tank
After amputation surgery, your body works overtime to heal wounds, rebuild tissue, and manage pain. This process demands energy, and that energy comes from what you eat and drink.
If your body isn’t getting enough nutrients, even the best therapy plan will fall short. Muscles won’t strengthen properly. Skin won’t repair itself as fast. Fatigue will set in quicker, and inflammation may linger longer.
This is why what you put on your plate matters just as much as the exercises you do. If you’re not eating enough protein, your muscles won’t grow. If you’re low on vitamins, your immune system may weaken, slowing down healing.
And if you’re not drinking enough water, your joints will stiffen, your skin will dry out, and your energy will plummet.
Many new amputees don’t realize this link. They focus on bandages, exercise routines, and medical appointments—but forget that every cell in the body needs fuel to function.
Without the right fuel, even simple movements during pre-prosthetic therapy can feel harder than they should.
Protein: The Muscle Builder You Can’t Skip
Protein is the number one nutrient your body needs to rebuild after surgery. It helps repair skin, grow muscle, and fight off infections.
During pre-prosthetic therapy, protein becomes even more important because your body is working to regain lost muscle tone and prepare for the load a prosthesis will add.
If your protein intake is low, your therapy may hit a wall. You might do all the right exercises but see slow progress.
Your therapist might notice that your strength plateaus or that you tire easily after basic tasks. In these cases, a simple change in diet—adding eggs, beans, fish, nuts, or dairy—can make a big difference.
Some people, especially older adults or those with chronic health conditions, may also benefit from protein shakes or supplements.
These help bridge the gap when appetite is low or meals aren’t balanced. Your medical team can guide you on safe and effective options tailored to your body’s needs.
Staying Hydrated Helps More Than You Think
Water doesn’t just quench thirst—it keeps your body moving smoothly. Proper hydration helps your muscles contract and relax, allows joints to stay flexible, and improves circulation. It also supports digestion, mental focus, and even mood.
Dehydration, on the other hand, can cause muscle cramps, dizziness, and sluggishness—all of which make therapy harder.
It can also make your skin more fragile, which is a serious issue when you’re preparing for socket use. Dry, thin, or irritated skin is more likely to break down under pressure, making socket fit painful or even unsafe.
Staying hydrated is simple, but easy to overlook. Some people drink less water after surgery because they move less, sleep more, or want to avoid frequent trips to the bathroom.
But skipping fluids can slow down healing and weaken performance during therapy.
A good rule is to drink small amounts of water often throughout the day. Avoid sugary or heavily caffeinated drinks that dehydrate the body.
And if you’re sweating during rehab or taking medication that affects fluid balance, drink even more.
Vitamins and Minerals That Support Healing
Beyond protein and water, certain vitamins and minerals also play a role in how ready your body is for therapy. Vitamin C helps with wound healing. Vitamin D supports bone health and muscle strength. Zinc helps fight infection. Iron supports energy and oxygen flow to your muscles.
If your body is low on any of these nutrients, it may take longer to see results from therapy. You might feel weaker, heal slower, or get sick more easily.
Many people recovering from surgery already have low levels of these nutrients—especially if they were in the hospital for long periods or had limited diets before surgery.
That’s why your rehab team may suggest a blood test or a consultation with a nutritionist. It’s not just about treating illness—it’s about speeding up your return to strength.
A small change in your diet today could mean getting your prosthesis sooner and using it more successfully later.
Eating Habits and Energy Levels in Daily Therapy
One of the subtle but important things nutrition affects is how much energy you bring into your therapy sessions.
If you skip meals, eat mostly processed foods, or rely on quick snacks, your energy levels will rise and fall in sharp waves. That makes it hard to stay focused, consistent, or motivated during therapy.
On the other hand, steady meals with whole grains, lean protein, and vegetables keep your body fueled in a more stable way.
You’ll have better stamina, sharper focus, and more patience for the physical and emotional challenges of therapy. And over time, that consistency becomes a major advantage.
Your therapist may not always talk about food, but they can usually tell when nutrition is helping—or holding you back. If you feel like you’re stuck, plateauing, or burning out, it might be worth looking at what’s on your plate.
Conclusion
Knowing when to begin pre-prosthetic therapy after amputation surgery isn’t just about timelines—it’s about readiness. Your body, mind, home environment, and even what you eat all play a role in how smoothly therapy begins and how well your prosthetic journey unfolds.
Starting therapy too early can slow healing. Waiting too long can delay progress. But with the right guidance, personalized care, and small daily habits, you can prepare your body for success. From wound healing and limb shaping to core strength and emotional resilience, each step builds toward a more comfortable and functional prosthetic fit.
There’s no perfect schedule. But with awareness, support, and consistent effort, you can find the right moment to begin—and move forward with confidence, strength, and purpose.