When someone faces a serious injury or a health condition that affects their leg or arm, one of the biggest and most emotional decisions is whether to try to save the limb or consider amputation. It’s a decision that comes with fear, confusion, and many questions. But one factor that often plays a big role in this choice—and is sometimes overlooked—is the risk of infection.
Infections can delay healing, lead to more surgeries, and even become life-threatening. For some people, trying to save the limb might mean months or even years of fighting infections that keep coming back. In other cases, amputation can actually offer a safer and more stable path forward.

Understanding Infection Risk in Limb Injuries
When a person has a serious injury or a medical condition like diabetes or poor blood circulation, the body’s ability to heal is often weakened.
In such cases, infection risk becomes one of the most important things doctors monitor. An infection isn’t just something that slows healing—it can stop it altogether or even put a person’s life in danger.
Why Infections Matter So Much
In a healthy person with a small wound, the body usually fights off bacteria on its own. But in complex injuries—especially those involving broken bones, open wounds, or damaged blood vessels—the body can’t always protect itself as well.
Bacteria can enter the body through cuts or surgical sites and start to grow. If not treated quickly, the infection can spread deep into the tissue or bone.
This type of infection, called an osteomyelitis when it affects the bone, is extremely hard to treat. It often requires strong antibiotics for weeks or months.
Sometimes, even that isn’t enough, and the infection keeps coming back. In these situations, doctors start to think seriously about whether saving the limb is the right goal—or whether it’s time to consider amputation.
Limb Salvage: What It Involves
Limb salvage is the medical term for trying to keep and repair a severely injured or infected limb.
It often requires many surgeries, including removing damaged tissue, placing metal rods or plates, or even taking healthy tissue from another part of the body to cover a wound. In some cases, doctors use special tools like vacuum devices to help wounds close.
This process can be long and painful. It usually includes long hospital stays, several rounds of antibiotics, and physical therapy to help regain movement.
For people with chronic health problems—like diabetes or vascular disease—this process is even harder because their body doesn’t heal as quickly. That means the risk of infection never fully goes away, even with the best care.
In some cases, the infection might go quiet for a while and then return later. Each return means more treatment, more cost, and more stress on the person.
Over time, some patients begin to feel like they are living in a cycle of surgeries and setbacks, rather than recovery.
When Infections Don’t Go Away
There comes a point in some cases where the infection becomes resistant to treatment. The wound doesn’t heal, or new areas of tissue start breaking down.
The body begins to show signs of exhaustion—fever, pain, and inflammation that doesn’t go down. The limb may begin to lose function. At this stage, continuing to try to save the limb may not be in the person’s best interest.
Doctors and patients must then ask a difficult question: is trying to save the limb actually causing more harm? This is where amputation becomes a valid, and sometimes even life-saving, option.
The Turning Point: When Amputation Becomes the Safer Path
Many people feel scared or defeated when they hear the word “amputation.” It’s understandable. The idea of losing a part of your body is emotional and overwhelming.
But the reality is, for people with constant infections and poor healing, amputation may be the best way to stop the spread of disease and start a real recovery.
Understanding the Shift in Focus
At first, the goal is always to save the limb—especially if the patient is young, active, or hopeful about recovery. But when the infection keeps coming back, or the limb is no longer functional, the conversation shifts.
It becomes about safety, quality of life, and the ability to live independently again.
At this stage, amputation is not a failure—it’s a decision made from strength and clarity. It’s about choosing life over pain, freedom over endless treatments, and movement over being stuck in bed or in a hospital room.
When infection becomes the enemy, removing the infected area can give the rest of the body a chance to heal and stay healthy.
The Role of Timely Decision-Making
One of the biggest risks in these cases is waiting too long. The longer a serious infection stays in the body, the more damage it does.
It can weaken the immune system, spread to other organs, and reduce the success rate of any treatment that comes after. Infections that reach the bloodstream—called sepsis—can be deadly.
That’s why doctors now focus on making timely decisions. They look at how the wound is healing, how the body is responding to antibiotics, and how the patient is feeling overall.
If signs point to long-term infection with no real improvement, they start preparing the patient for the possibility of amputation.
The goal is never to rush. But waiting too long can make things worse—not just physically, but emotionally too. Knowing when to shift the plan is key.

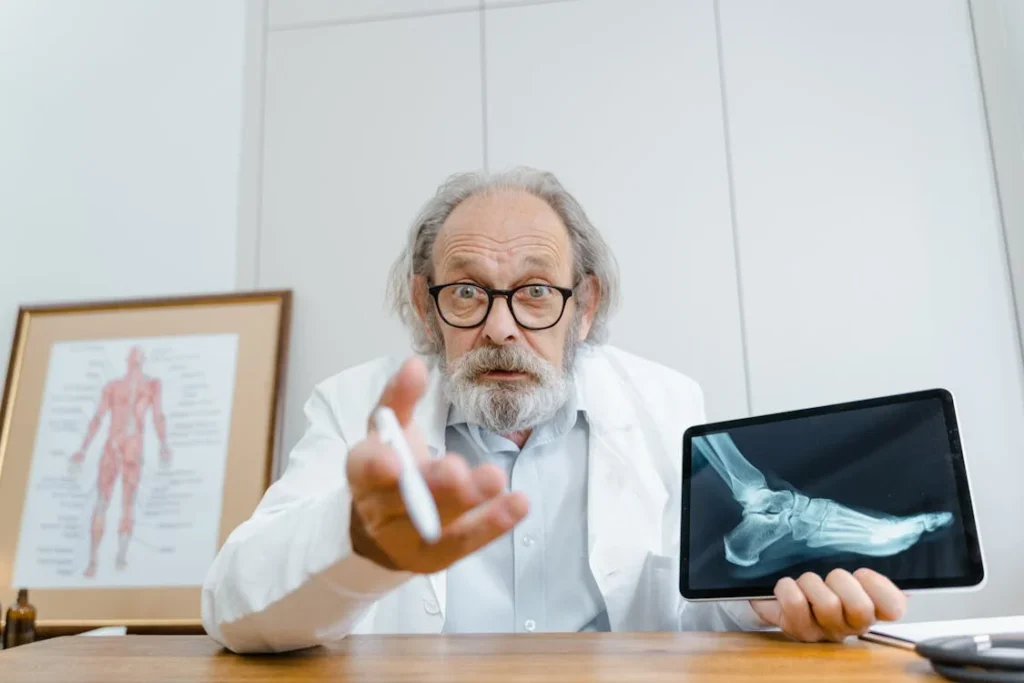
Talking Honestly: Patients, Doctors, and the Infection Risk Conversation
One of the hardest parts of deciding between limb salvage and amputation is the uncertainty. Will the infection clear? Will the limb heal enough to be useful again? Will all this pain and effort actually lead to a normal life? These are not easy questions, and there are no perfect answers. That’s why honest, clear conversations between patients and doctors are so important.
Setting Realistic Expectations
When doctors meet with someone who has a high infection risk—either from an injury, diabetes, or a condition like peripheral artery disease—they have to explain what recovery might look like. Not just the hopeful version, but the real one.
Limb salvage may sound more appealing at first, but it can mean a long path filled with hospital visits, wound care, daily antibiotics, and physical limits that might never fully go away.
For someone who wants to return to work, care for their family, or live without constant medical care, this path may not be ideal.
That’s where discussing the amputation option comes in—not as a last resort, but as a thoughtful plan. It’s a shift from thinking “How do we save this limb?” to “How do we give this person their life back?”
These conversations need trust. Patients have to feel safe enough to ask hard questions. Doctors have to be willing to talk openly—not just about medical facts, but about daily life after either choice.
And if amputation is suggested, it must come with reassurance: that it’s not the end of independence, but a different kind of beginning.
Psychological Weight of the Decision
There’s no ignoring the emotional toll that both choices carry. Trying to salvage a limb and failing can feel deeply frustrating.
Choosing amputation can feel frightening, even when it’s the right decision. People often fear how they’ll look, what others will say, or how they’ll manage everyday tasks.
These feelings are normal. That’s why mental health support is just as important as medical treatment. Talking to a counselor or therapist during the decision-making process can help patients feel more grounded.
Peer support groups, where patients can meet or talk with others who’ve made similar choices, also offer incredible emotional strength.
Seeing real-life stories helps people imagine what’s possible. A conversation with someone living well after an amputation can be more powerful than any brochure or medical diagram.
It helps remove fear and replace it with a more realistic and hopeful view of the future.

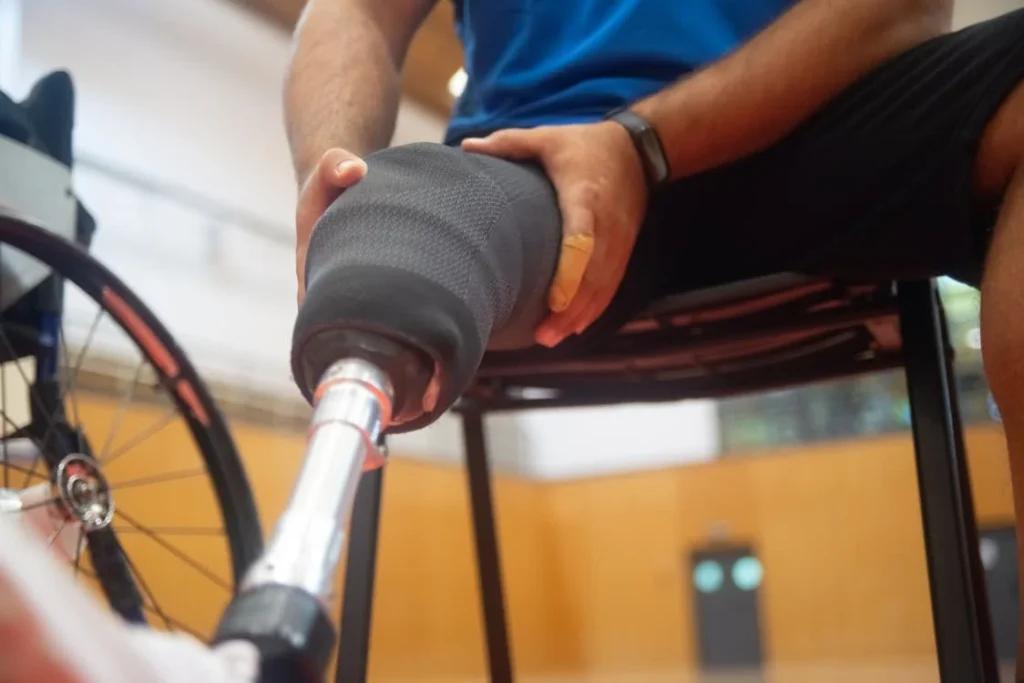
Modern Prosthetics: Changing What Amputation Means
One major reason why more people today are considering amputation as a valid choice—especially in cases of high infection risk—is because prosthetic technology has come a long way.
Amputation doesn’t have to mean the loss of mobility, freedom, or identity. In fact, for many people, it can be a return to those things.
Functionality That Restores Confidence
Modern prosthetics are not just about appearance. They are about movement, stability, and real use in daily life. A well-fitted prosthetic leg can help a person walk, climb stairs, ride a bike, or return to work.
An advanced hand prosthetic can help with tasks like holding a cup, typing on a computer, or using tools.
These are not luxuries. They’re everyday actions that make life feel normal again. When people see that a prosthetic can let them do what they couldn’t do with a painful, infected limb, their mindset begins to shift.
Suddenly, amputation becomes less about loss and more about opportunity.
And for those who feared they’d never be able to move freely again, this realization is incredibly powerful.
Comfort and Customization
Comfort is another major change in today’s prosthetics. In the past, many devices were heavy or caused skin irritation. They weren’t easy to wear for long hours.
Now, with better materials, lighter builds, and custom-fitted sockets, the experience is totally different. A well-designed prosthetic feels more like part of the body than a separate tool.
Customization also means the device can fit a person’s lifestyle. Whether they need more flexibility for movement or a stronger build for work tasks, the prosthetic can be made to suit those needs.
This level of personalization is what helps many patients feel that they’re not just adjusting to a loss—but building something better for their future.

Quality of Life vs. Quantity of Treatment
When someone is facing constant infection and a limb that may never fully recover, the conversation naturally turns toward quality of life. It’s not just about whether a limb can be saved.
It’s about whether life with that limb will be worth living—free of pain, full of function, and mentally peaceful.
When Treatment Becomes the Burden
In limb salvage cases, especially those complicated by infection, the treatment itself can start to feel like the illness. Multiple surgeries, hospital stays, strong antibiotics, and time away from work or loved ones—it all adds up.
The emotional and physical toll is high. For some, this burden becomes heavier than the idea of living without the limb.
There’s also the question of time. How long will the recovery take? How many weeks or months of life will be spent just trying to “fix” something that may never work the way it should?
These are important questions that don’t have easy answers, but they deserve to be asked.
That’s why many people in this situation choose to look at their full picture. They ask themselves: what kind of life do I want in one year? In five years?
If limb salvage can’t promise a good quality of life, then amputation, followed by proper rehabilitation and prosthetic fitting, starts to make more sense.
Reducing Mental Exhaustion
One thing that’s not talked about enough is decision fatigue. When someone is stuck in a cycle of slow healing and recurring infections, they’re constantly making medical choices—more antibiotics, another dressing change, another consultation.
It’s draining. Every minor setback can feel like starting over. That kind of mental exhaustion makes it hard to think clearly, stay positive, or plan ahead.
Amputation, on the other hand, brings closure to that uncertainty. It’s a bold decision, but for many, it ends the medical guessing game.
It replaces “maybe” with a plan. And from there, it becomes about building back—not waiting and hoping that things will change.
Long-Term Outcomes: What the Research Says
Data from hospitals and medical studies over the years has shown that, in certain high-risk cases, patients who undergo amputation after failed limb salvage often report higher satisfaction levels than those who continue with prolonged treatment.
Why? Because once the infection is gone and healing is complete, they can begin to live again—without fear of relapse.
Fewer Hospital Visits, More Mobility
One clear benefit of timely amputation is a lower risk of returning to the hospital.
Once the infected limb is removed and the residual limb is properly healed, the chances of further infection drop dramatically. Compared to ongoing wound care or recurring surgeries, that’s a huge relief.
Patients with well-fitted prosthetics also tend to regain independence faster. They’re able to walk, work, drive, or travel with far fewer limitations. And while there is an adjustment period, many say the freedom they gain outweighs the challenges.
This doesn’t mean amputation is the best option for everyone—but in cases where infection keeps coming back, it often leads to better long-term results, both physically and emotionally.
Personalized Paths, Not One-Size-Fits-All
It’s important to say this clearly: there is no single “right” answer for every case. Each person’s health, goals, and lifestyle are different.
What matters most is that the decision is made with full awareness of what’s possible—and what’s at risk if things continue as they are.
Doctors now aim to personalize every treatment plan. They weigh the chances of full recovery against the burden of repeated treatments.
They bring in prosthetic experts early in the conversation, not at the end. That way, the patient can understand what life could look like after each option—and choose with confidence, not fear.
The Role of Early Detection and Monitoring in Shaping Outcomes
Modern medicine isn’t just about reacting to infections—it’s increasingly about predicting and preventing them. As technology continues to grow, so does the ability to detect infections earlier, monitor healing more closely, and make more informed decisions before the infection reaches a dangerous stage.
This new layer of insight is quietly changing how doctors and patients approach the limb salvage versus amputation decision.
Smart Wound Monitoring Tools
Traditionally, wound care depended on visual checks—redness, swelling, smell, or pus. But by the time these signs show up, the infection may already be well established.
Today, we have more advanced tools. Some hospitals and clinics now use smart bandages, thermal imaging, or sensor-based dressings that can track changes in temperature, moisture, or bacteria levels in real time.
These tools allow doctors to see what’s happening below the surface. They can catch signs of infection even before they’re visible, which means they can act faster.
In many cases, this early detection prevents the need for emergency surgeries or major debridement. And if it becomes clear that the infection isn’t responding to treatment, decisions like amputation can be made before the situation gets worse.
Data-Driven Decision Making
Another powerful shift is the use of data to track recovery over time. Digital health records, wound photography, and AI-powered analysis now allow clinicians to see trends—whether a wound is slowly healing or slowly getting worse. This kind of information isn’t just helpful—it’s critical.
Instead of relying only on gut feeling or general timelines, doctors can now use clear, trackable evidence to decide when to switch strategies.
For example, if a wound has not reduced in size after several weeks of antibiotics, or if tissue oxygen levels stay low, the data helps confirm what the next step should be. This means fewer delays in switching from salvage to amputation when needed—and better timing overall.
Empowering Patients Through Tech
It’s not just doctors who benefit from new tech—patients do too. With tools like mobile apps, home-monitoring kits, and even simple wound-tracking charts, people can now be more involved in their own care.
They can photograph their wound, track their pain levels, or even scan QR-coded dressings that link to healing tips and alerts.
This shared responsibility helps reduce delays. Instead of waiting until a weekly clinic visit to mention a problem, patients can alert their care team as soon as something feels wrong.
Early intervention reduces the risk of deep infection, which can often be the turning point in the salvage vs. amputation conversation.
A New Path to Prevention-First Care
What we’re seeing now is the start of a broader shift. With better monitoring and faster response times, the entire process becomes more proactive.
Doctors can stop infections before they spread. Patients can play a bigger role in healing. And everyone has more time to think clearly, plan ahead, and make balanced decisions.
This doesn’t erase the need for hard choices—but it gives people more control over when and how those choices happen. In many ways, it gives time back. And in the fight against infection, time is everything.
Reframing the Decision: Health, Not Heroics
The idea of saving a limb at all costs is deeply rooted in how we think about strength, survival, and medical progress. But saving a limb should never come at the cost of a person’s peace, health, or future.
In high-risk cases where infection becomes persistent or life-threatening, choosing amputation is not giving up. It’s choosing to stop surviving and start living.
What’s changing now is the language around this choice. More patients and doctors are beginning to understand that “saving” doesn’t always mean keeping a body part.
Sometimes it means saving someone’s time, energy, and dignity. And when the risk of infection turns a limb into a constant source of danger or pain, letting it go can be the strongest, most self-respecting decision a person makes.
With better tools, smarter prosthetics, early infection detection, and more honest conversations, patients now have the power to choose not just how they recover—but why.
They can make decisions that reflect not just their medical status, but their life goals, values, and dreams for the future.
Conclusion
The decision between limb salvage and amputation is never easy, especially when infection risk hangs in the balance. But modern medicine is shifting that decision from a fearful last resort to a well-informed choice. Today, with better monitoring, personalized care, and prosthetic technologies that return mobility and independence, amputation is no longer the end—it’s often a new beginning.
What matters most is making that decision with clarity. Not driven by fear. Not pressured by outdated thinking. But supported by facts, by trusted voices, and by a clear understanding of what kind of life lies on the other side.
Infection may try to take control, but with the right care, the right timing, and the right tools, people can take that control back—and step into the future they deserve.



