
Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
For many clinicians, the surgery is only the first step. What happens after the operation
The journey from amputation to prosthetic fitting is rarely straight. For every patient, healing follows its own rhythm. Yet, one truth stands firm: faster, safer recovery depends not just on wound care, but on how well the body’s inner systems are managed.
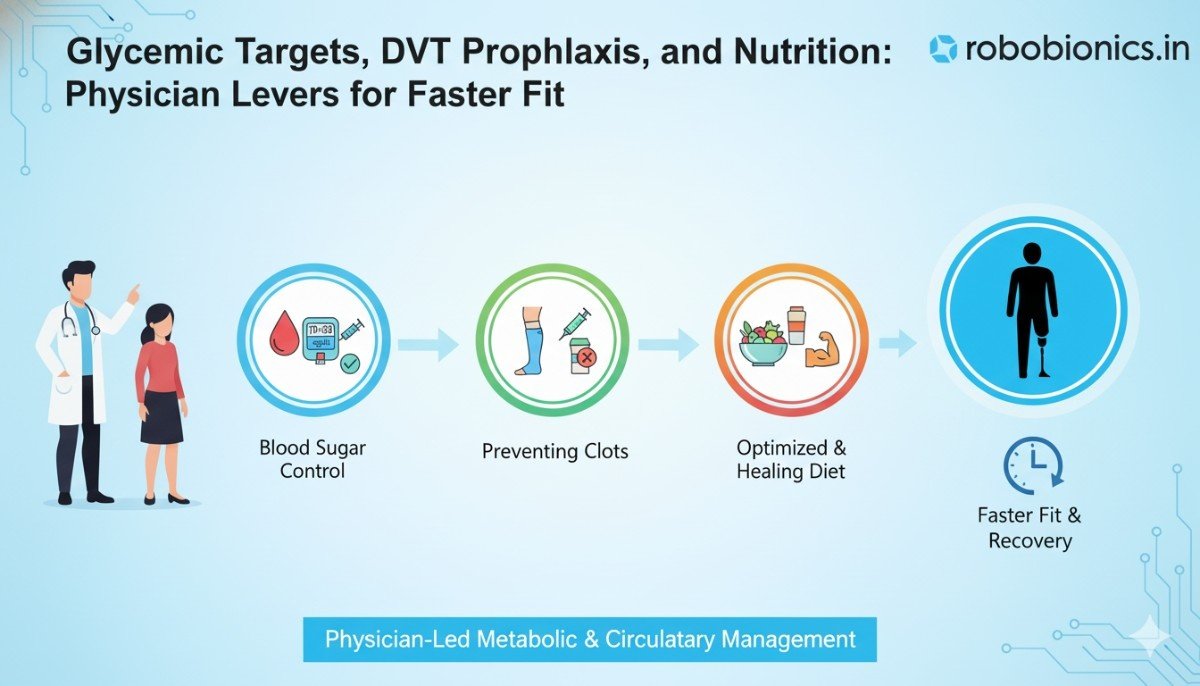
Behind every smooth recovery story is a doctor making quiet, calculated moves—keeping blood sugar stable, preventing dangerous clots, and feeding the body just what it needs to rebuild. These are the invisible levers of progress. They don’t just heal wounds; they prepare the limb and the person for the prosthetic that’s waiting ahead.
This article explores those levers—glycemic control, DVT prophylaxis, and nutrition—and how they speed up readiness for socket fitting. It’s a practical guide for physicians, physiatrists, and rehab teams who want every patient to reach mobility faster, stronger, and with fewer setbacks.
When a limb is lost, the body is under immense stress. That stress itself can spike blood sugar. Add in limited mobility, pain, and altered metabolism, and glucose levels often rise even in patients who were not previously diabetic.
High blood sugar quietly slows down every stage of wound healing. It thickens the blood, clogs small vessels, and starves tissues of oxygen. It feeds bacteria. It dulls the immune system’s response.
In other words, uncontrolled sugar doesn’t just slow healing—it keeps the wound open longer, delays prosthetic fitting, and increases the risk of infection under the socket later.
Doctors often debate how tight blood sugar control should be in post-amputation patients. Too high, and infection risk rises. Too low, and the patient risks hypoglycemia, which can also delay recovery.
For most patients, a fasting blood glucose between 90–130 mg/dL and a postprandial level under 180 mg/dL is safe. The exact target depends on the patient’s age, comorbidities, and energy needs.
The goal is steady, predictable control—not aggressive correction. Consistency allows tissues to heal in a calm environment where blood flow and nutrient delivery remain optimal.
Small, repeatable routines make the biggest difference. A steady meal schedule, moderate activity (as allowed), and regular hydration keep glucose fluctuations gentle.
For inpatients, blood sugar checks before meals and at bedtime provide the rhythm for insulin or medication adjustment. For outpatients, home glucose monitoring at least twice a day during early rehab helps spot patterns quickly.
The doctor’s role is to teach—not just prescribe. When patients understand what each reading means, they take ownership of healing.
Even short bursts of high sugar slow tissue repair. Elevated glucose stiffens white blood cells, dulling their ability to fight infection. It thickens blood, reducing oxygen delivery to the wound edge. It also changes collagen formation, making new tissue weak and fragile.
If the patient wears a prosthetic too soon under those conditions, the fragile tissue can break open again. That means more dressing changes, more rest, and more frustration.
Physicians should reassess diabetic medication needs immediately after amputation. Reduced physical activity often means lower calorie use, so insulin or oral drug doses may need modification.
Sliding scale insulin can cover temporary spikes. But longer-term, stable basal-bolus therapy or a controlled oral regimen gives smoother results. The trick is to stay proactive—never waiting for hyperglycemia to appear before acting.
Stress, grief, and anxiety after limb loss also affect blood sugar. Cortisol and adrenaline push glucose up. Patients who feel heard and supported often show better metabolic stability.
This is why early counseling, family involvement, and positive communication matter. The body listens to the mind. Calm, informed patients heal faster.
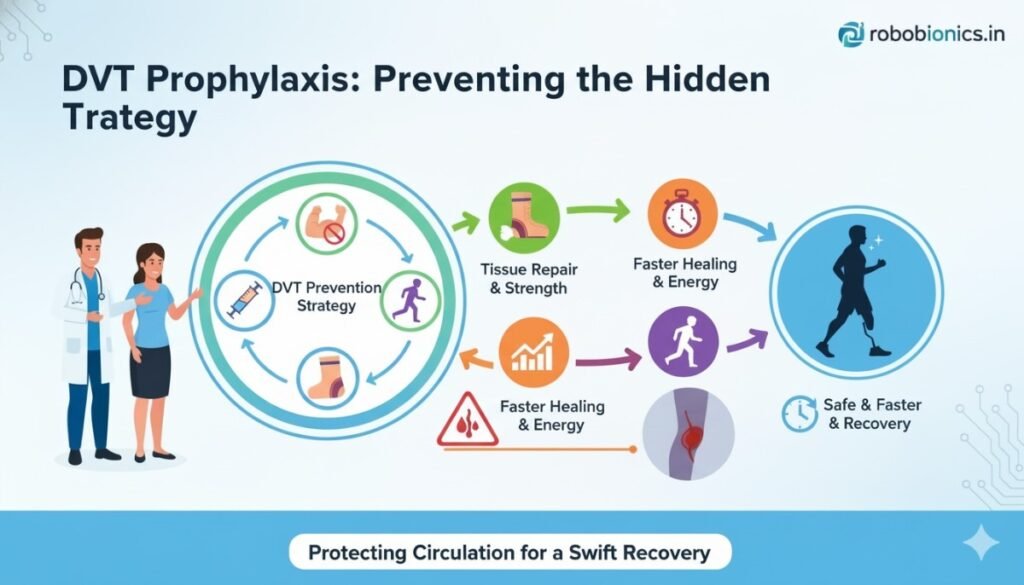
After amputation, the body slows down. The limb is immobilized. Blood moves sluggishly through veins that are already healing from surgical trauma. Add dehydration, pain medication, and bed rest, and the perfect setup for deep vein thrombosis (DVT) appears.
A clot in a deep vein doesn’t just cause swelling or pain. It can break off and travel to the lungs—a pulmonary embolism, often fatal. Many times, there are no early symptoms. That’s why prevention isn’t optional.
The risk for DVT peaks during the first 2–3 weeks after surgery but doesn’t vanish after discharge. Even mild swelling or reduced movement can keep the danger alive.
Physicians need to balance early mobility with safety. Compression, anticoagulants, and hydration form the core strategy.
A sudden increase in swelling, warmth, or dull ache in the thigh or calf deserves immediate attention. Physicians should educate patients and caregivers to report these symptoms quickly.
If DVT is suspected, a Doppler ultrasound confirms it. Quick detection can be life-saving.
Why discuss DVT in an article about faster socket fitting? Because clot formation delays everything. A swollen limb cannot be measured, compressed, or shaped properly. Blood pooling in tissues slows healing and may even reopen closed wounds.
Preventing DVT keeps circulation smooth. Smooth circulation means faster wound contraction, stronger scar tissue, and earlier limb stabilization—the key for an accurate prosthetic fit.
Doctors should view DVT prophylaxis as both medical and rehabilitative care. Preventing clots means protecting healing momentum. It keeps the patient’s recovery timeline intact.
Close communication between surgeons, nurses, and physiotherapists ensures no one forgets prophylaxis once the wound “looks fine.” It remains crucial until the patient is moving confidently with their prosthesis.
Wound healing and tissue regeneration are not magic—they are biology. And biology needs raw materials. Protein, vitamins, minerals, and fluids are the bricks and mortar of recovery.
Unfortunately, many patients eat poorly after surgery. Loss of appetite, depression, or hospital food preferences reduce calorie intake right when the body needs more.
Doctors and rehab teams who make nutrition a daily conversation help patients recover weeks faster.
A healing body needs fuel. Most adults require 25–30 calories per kilogram of body weight daily during recovery, sometimes more. Protein needs rise sharply—about 1.2 to 1.5 grams per kilogram per day—to rebuild tissues and immune cells.
When protein intake is too low, wounds take longer to close, scars form weakly, and muscles waste away. That muscle loss directly affects prosthetic control later.
Vitamin C supports collagen formation. Zinc aids tissue repair. Iron helps oxygen delivery. B vitamins maintain nerve and muscle health.
Deficiencies in any of these can quietly slow progress, even if the wound looks clean on the surface. Physicians should watch for pale skin, fatigue, or slow scar formation—small clues that nutrition is falling short.
Painkillers and stress can dull appetite or alter taste. Instead of forcing large meals, smaller, nutrient-rich portions work better. Smoothies with protein powder, milk, or lentils provide easy calories without burdening digestion.
For diabetic patients, balanced meals with low-glycemic carbs prevent sugar spikes while still fueling healing.
Water keeps blood thin, skin elastic, and nutrients moving. Yet dehydration is common after surgery. Encourage regular sips throughout the day rather than large drinks at once.
Signs like dry lips, concentrated urine, or dizziness often point to dehydration—an easy fix with big benefits.
If eating enough solid food is difficult, protein shakes or fortified drinks help. For patients with specific deficiencies, short-term supplementation of vitamin C, zinc, or iron may speed recovery—but always under physician supervision.
The key is moderation. No single pill replaces real food. The goal is a diet built from simple, local, nourishing ingredients that the patient enjoys and can sustain.
The body is an ecosystem. Blood sugar, circulation, and nutrition aren’t separate—they support each other.
Controlled glucose improves blood flow and helps nutrients reach tissues. Good nutrition stabilizes sugar levels and strengthens veins. DVT prevention keeps oxygenated blood moving freely to where it’s needed.
When physicians align these three levers, patients move from healing to fitting faster, safer, and with far fewer complications.
Take the case of a 55-year-old diabetic man who underwent below-knee amputation after a severe infection. His early weeks were rough—blood sugar often touched 250 mg/dL, and swelling made it hard to apply compression.
His physician stepped in with three small changes: tighter glucose monitoring with slow insulin adjustments, daily LMWH for two weeks, and a protein-rich meal plan designed with his family.
For patients healing from amputation, unpredictability is the enemy. A good physician builds structure into each day: consistent meal times, medication schedules, and gentle physical activity. Predictability stabilizes metabolism and keeps the body from swinging between extremes.
Doctors should start by reviewing each patient’s pre-surgery sugar trends. If the person was previously non-diabetic but is now showing high readings, stress hyperglycemia is likely. The answer isn’t aggressive insulin right away—it’s a steady approach with gradual titration and close monitoring.
Checking fasting, post-meal, and bedtime readings for the first few weeks gives a rhythm to treatment. Patients who feel included in this routine, rather than controlled by it, often maintain discipline far better.
A “one-size-fits-all” plan doesn’t work here. Each patient’s body, diet, and healing rate demand personalization.
For stable type 2 diabetics, oral medication with adjusted doses may suffice. But when tissue repair is the top priority, insulin therapy often gives tighter control. It lets doctors respond fast to changing needs—an advantage during wound healing, when the body’s fuel demands rise and fall.
The target isn’t textbook perfection; it’s stability without hypoglycemia. Every low sugar episode delays healing as much as a high one does.
Nurses and physiotherapists play a critical role here. They see the patient daily, notice appetite shifts, fatigue, or mood swings that could signal unstable glucose levels. When physicians build open communication with their team, adjustments happen early, before a small issue turns into a big one.
Blood sugar often climbs at night due to stress hormones and inactivity. Night-time insulin adjustments or slow-digesting snacks like milk with protein can help prevent this. Stable night sugars mean the body wakes ready to heal, not recover from another glucose spike.
A controlled carbohydrate plan supports medical management. Meals that pair complex carbs with protein and fiber keep sugar curves smooth.
In India, where rice and bread dominate, small substitutions—like mixing brown rice with white, adding lentils or sprouts, or including a handful of nuts—can make a measurable difference.
Doctors should guide families on portion control rather than restriction. The goal is not to deny food but to redesign it.
After amputation, the patient’s body slows down—not just physically, but metabolically. The heart rate drops, calf muscles stay still, and venous return weakens. Blood pools in the lower body, setting up the perfect storm for DVT.
The physician’s job is to break this loop early.
Even the smallest movement counts. Once the wound is stable, gentle leg lifts, ankle pumps, and rolling from side to side in bed improve venous flow. For above-knee amputees, assisted sitting and transfers from bed to chair provide similar benefits.
Doctors should authorize physiotherapy early, not wait for complete closure. Controlled movement under supervision is safer than complete stillness.
Compression is both science and art. Applied too loosely, it’s useless; too tight, it cuts off circulation. The ideal wrap starts from the end of the residual limb and spirals upward, maintaining gentle, even pressure.
Doctors should ensure the team knows how to check for color, warmth, and capillary refill after applying compression. A well-trained nursing staff prevents 90% of DVT complications this way.
Shrinkers—specialized compression sleeves—can replace bandages once swelling stabilizes. They not only prevent clots but also shape the limb for socket casting.
While heparin or oral anticoagulants are vital, they must be tailored carefully. Overuse can cause bleeding in healing tissues, which sets the process back.
Physicians can adopt a time-limited prophylaxis plan: for example, LMWH for 10–14 days post-op, then reassess based on mobility and wound stability. For longer-term immobile cases, low-dose aspirin or continued compression therapy can be considered.
Clot prevention isn’t only about medication. Many patients, especially the elderly, drink less after surgery to avoid frequent urination. This thickens the blood, making clots easier to form.
A simple prescription—one glass of water every hour during waking time—often makes a measurable difference. It’s one of the cheapest and most effective DVT prevention tools available.
Sometimes, the only early symptom of DVT is restlessness or mild discomfort in the thigh. A good physician looks beyond visible swelling.
Regularly checking limb circumference, temperature, and pain levels builds an early warning system. Educating families to recognize these clues extends that vigilance beyond hospital walls.
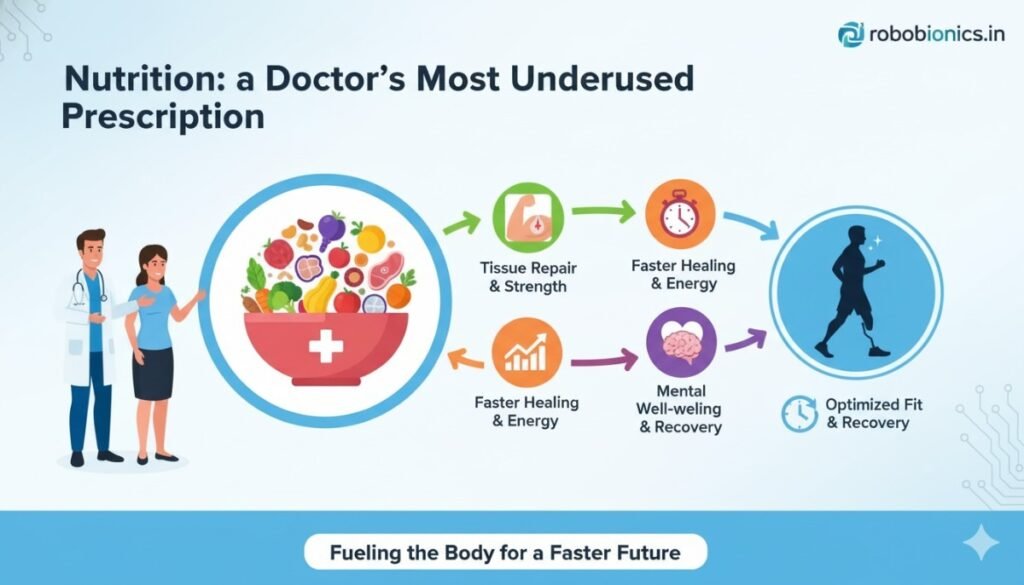
Food can be medicine when prescribed with purpose. For post-amputation patients, nutrition isn’t just about calories—it’s about creating the biochemical environment for regeneration.
Doctors who take five minutes to discuss food during each visit transform recovery outcomes. A patient who understands why every bite matters is far more likely to heal on time.
Healing follows a rhythm. Protein intake spread evenly across meals works better than loading it all at dinner. The body can only absorb and use so much at a time.
Encouraging patients to have protein in breakfast and lunch ensures nutrients are available when the body’s repair machinery is most active.
For diabetics, pairing carbohydrates with fat or protein slows glucose absorption. So a bowl of rice with dal, curd, or paneer works better than plain rice. These simple cultural adaptations are easy to follow and sustain.
A light bedtime snack—like milk with turmeric or a boiled egg—also prevents night-time sugar dips and supports stable healing overnight.
Immobility shrinks muscle fast. Protein-rich meals alone can’t stop it; the body needs stimulus. That’s why doctors should pair dietary advice with light resistance therapy as soon as it’s safe.
Even seated arm exercises or isometric holds keep metabolism active and reduce insulin resistance. The goal is not just to feed muscles but to remind them they still have work to do.
Zinc, iron, vitamin D, and vitamin C are the hidden catalysts of recovery. Zinc deficiency alone can double wound-healing time.
In India, where vegetarian diets are common, iron and zinc levels often run low. A short course of supplements—or foods like jaggery, pulses, and seeds—fills this gap naturally.
Doctors should also monitor vitamin D levels. Exposure to sunlight for 20 minutes a day can do wonders for both bone strength and mood.
Proper hydration helps nutrients circulate and toxins flush out. But plain water isn’t the only way—soups, buttermilk, and tender coconut water also count.
Encourage patients to drink before they feel thirsty, since thirst perception often declines with age or medication use.
A skilled physician looks at each patient as a system, not a sum of problems. During rounds, a quick glance at three numbers can predict recovery trajectory: fasting blood sugar, hemoglobin, and limb circumference.
If sugar is stable, hemoglobin is improving, and swelling is down, the patient is on track for early prosthetic readiness. If even one slips, small interventions can bring them back fast.
Every team member—from nurses to dietitians—should know the current glycemic goal, mobility plan, and meal schedule.
A short note on the chart—like “Target FBS <130, encourage 1L extra fluids, rewrap limb after physiotherapy”—turns good intentions into action.
This level of coordination ensures that care remains continuous even during shift changes or discharge transitions.
Doctors often ask, “When is my patient ready for socket fitting?” The answer lies in a combination of objective and intuitive markers.
The wound must be closed, yes—but also dry, calm, and stable in size for at least one week. Blood sugar should have remained consistent for 10–14 days. The patient should be off prophylactic anticoagulants and moving without new swelling.
When these align, it’s the perfect moment to introduce the prosthetist.
Not every patient will heal on schedule. The key is to spot what’s holding them back—uncontrolled sugar, poor nutrition, or lingering edema—and address it directly.
A single dietary tweak or medication change can restart progress. Physicians should remind patients that temporary delays are not failures; they’re recalibrations.
Numbers can only go so far. Encouragement turns compliance into habit. When doctors celebrate small victories—a day of stable sugar, a wound size reduction, a successful physiotherapy session—the patient feels seen.
This emotional boost often reflects in better appetite, steadier glucose, and more consistent participation in care routines.
Patients remember what they understand. Explaining complex medical advice in simple, local language helps them act on it.
Telling a patient, “Your wound heals better when your sugar stays under 130,” lands more effectively than a lecture on HbA1c and insulin resistance.
When people grasp cause and effect, they take ownership of results.
The first few weeks after surgery are about survival—closing the wound, preventing infection, and keeping blood sugar from soaring. But once the crisis phase ends, the physician’s role shifts toward long-term stabilization.
This phase is less dramatic but more critical. Healing may look complete on the surface, yet tissue strength and scar maturity depend on stable glucose over months. The goal is to maintain a healthy internal environment that keeps the skin strong under daily prosthetic pressure.
Physicians should gradually transition patients from hospital-based monitoring to self-managed routines. Education, not medication, becomes the foundation.
When patients understand how meals, mood, and movement affect their sugar, control becomes natural. Doctors can use simple visual tools like “traffic light charts” to help them interpret readings:
By empowering patients to spot trends early, doctors reduce emergency calls and prevent setbacks.
For long-term control, longer-acting insulin analogues or combination oral drugs often work better. They provide steady background control, avoiding daily peaks and valleys.
The ideal plan is one that fits the patient’s life—not the other way around. A rigid regimen that doesn’t match local diet, sleep, or work habits will fail. Adjusting the plan around real-life patterns keeps compliance high and stress low.
Once the patient starts walking with a prosthesis, metabolism changes again. Muscle movement improves insulin sensitivity, and calorie demands rise. Doctors should anticipate this and adjust doses before hypoglycemia appears.
A good practice is to recheck fasting and post-meal glucose during the first two weeks of prosthetic training. Stable readings mean the plan is working; sudden dips signal the need for dose or diet revision.
Relapses happen—especially around festivals, social gatherings, or emotional stress. Instead of punishment, physicians should use setbacks as teaching moments.
Explaining why one high reading doesn’t erase weeks of progress helps patients stay motivated. The best care feels supportive, not strict. Over time, this relationship builds lasting discipline.

Even months after discharge, a patient can develop deep vein thrombosis, especially if mobility remains limited. Long car rides, dehydration, or a sedentary routine are common triggers.
Physicians should counsel every amputee on lifelong DVT awareness. Prevention doesn’t stop when the wound closes—it evolves.
Walking with a prosthesis is excellent natural protection. Each step squeezes the calf muscles, pumping blood upward and preventing clot formation.
For patients not yet full-time ambulators, daily exercises like ankle rotations (for the intact leg), arm pumping, or deep breathing help keep circulation active.
Doctors can prescribe structured physiotherapy schedules, emphasizing both sides of the body. Balanced movement prevents overuse on the intact leg while maintaining systemic flow.
If the patient has a history of DVT, prolonged low-dose anticoagulation may be needed. The challenge lies in balancing clot prevention with bleeding risk, especially under the prosthetic socket where microabrasions are possible.
Routine follow-ups, clotting time checks, and medication reviews every three months ensure safety. Physicians should also teach patients to avoid over-the-counter painkillers like NSAIDs that can increase bleeding risk.
Post-amputation patients often face their first major travel during prosthetic training or after fitting. Long flights or bus rides are a classic DVT trigger.
Doctors can advise a simple protocol:
A few minutes of motion every hour can prevent weeks of complications later.
Omega-3 fatty acids, found in flaxseed, walnuts, and certain fish, keep blood slightly thinner and more flexible. Including them regularly in the diet adds natural protection.
Balanced hydration—neither dehydration nor excessive water intake—also keeps blood flow optimal. A pale-yellow urine color is the simplest marker for good hydration.
Early wound-healing diets are high in calories and protein, but once healing is complete, balance returns to the forefront. The physician’s role here is to ensure that patients don’t overcorrect by cutting calories too sharply.
The new focus becomes muscle strength, stable weight, and heart health—all essential for comfortable prosthetic use.
Even after recovery, daily protein needs remain higher than pre-surgery levels. Ongoing tissue renewal under the prosthetic demands amino acids.
Encourage patients to keep one high-quality protein source in every main meal—whether it’s eggs, paneer, pulses, fish, or soy. Doctors can tailor recommendations to regional diets, so patients stay consistent without feeling restricted.
Healthy digestion ensures nutrients reach the skin efficiently. Chronic constipation, acidity, or bloating can indicate an imbalance that slows absorption.
Advising patients to include fermented foods like curd or buttermilk, along with fiber from vegetables and fruits, keeps the gut in sync. A happy gut means smoother skin and fewer prosthetic irritations.
Every six months, physicians should recheck vitamin D, hemoglobin, and serum protein levels. Subtle deficiencies can reappear over time, especially if diet habits slip.
Reinforcing supplements briefly during winter months or after illness keeps the body resilient.
The act of eating well also carries psychological power. Many amputees experience guilt, frustration, or low self-worth post-surgery. Teaching them to view food as a tool for strength—not a comfort or punishment—restores control and dignity.
A warm conversation about simple home-cooked food can often do more healing than a prescription.
The fastest healers share one trait: they don’t just follow instructions—they co-create their care plan. Physicians who involve patients in setting targets see higher engagement and fewer setbacks.
Instead of saying, “Keep your sugar under 130,” a doctor can ask, “What times of day does your sugar rise the most?” This invites ownership and insight.
When the patient feels responsible, every choice—meal, walk, water intake—becomes intentional.
Families often control meal timing, medication reminders, and emotional support. Involving them early in discussions about diet, compression, and exercise ensures consistency at home.
For older patients, family participation prevents forgetfulness or neglect. For younger ones, it reduces resistance and keeps morale high.
Doctors should encourage one designated family member to attend follow-ups, ask questions, and record key advice.
True recovery is multidisciplinary. The surgeon, prosthetist, physiotherapist, dietitian, and physician form a single circle around the patient.
Weekly coordination—either through shared notes or brief calls—prevents overlap and confusion. For example, if physiotherapy intensifies, the physician can preemptively adjust calorie and insulin needs.
This seamless handoff ensures the patient’s progress remains smooth and predictable.
Instead of focusing only on numbers like blood sugar or hemoglobin, physicians should track milestones: wound closure date, swelling reduction, compression tolerance, and first full prosthesis wear.
Milestone tracking shows real-world progress and motivates both patient and team. It also helps predict when to introduce advanced rehabilitation tools like myoelectric prosthetics.
Sometimes the most strategic move is to slow down. If the patient shows rising sugar, new swelling, or poor appetite, forcing progress risks setbacks.
Doctors who recognize when to pause therapy and focus on stabilization ultimately save weeks of rework. A two-day rest today can prevent a two-month delay tomorrow.

Every amputation leaves emotional echoes—fear, grief, and self-doubt. These emotions often manifest physically: poor appetite, sugar spikes, skipped medication, or insomnia.
Physicians who make time to ask, “How are you coping?” invite honesty. When patients feel heard, compliance naturally improves.
Humans crave stability after chaos. Doctors can turn daily care routines—checking sugar, cleaning the limb, eating on time—into predictable rituals that bring peace.
Rituals reduce anxiety, which in turn lowers stress hormones and stabilizes glucose naturally. It’s a subtle yet powerful connection.
Simple visual tools like comparing wound photos, tracking glucose charts, or measuring limb circumference give patients tangible proof of improvement.
When progress is visible, motivation blooms. A motivated patient eats better, moves more, and heals faster.
Before giving the final clearance for prosthetic fitting, doctors must ensure three physiological pillars are firm:
These parameters ensure the limb can handle pressure, friction, and weight distribution safely.
A direct handover meeting between physician and prosthetist prevents communication gaps. Sharing recent sugar trends, medications, and physical restrictions helps the prosthetist plan the socket design and initial wear schedule correctly.
This teamwork turns the transition from medical to mechanical care into a smooth handoff rather than a risky leap.
The physician’s words often shape expectations. Remind the patient that the first socket is not the final one—it’s part of the learning curve.
Setting this mindset reduces disappointment and keeps enthusiasm alive through adjustments.
The period immediately after the prosthesis is fitted is just as critical as the weeks before. Skin that looks healed must now adapt to new pressure, friction, and heat. The physician’s job isn’t done—it simply evolves.
Regular follow-ups every two weeks during the first month help ensure that sugar remains stable, circulation strong, and nutrition adequate. Any small wound or redness under the socket must be treated with the same seriousness as the initial incision.
A stable body chemistry supports stable skin. A patient with erratic sugar or dehydration will always find the prosthesis harder to tolerate.
Even a mild rash or blister can signal friction or high local pressure. If not addressed quickly, it can lead to infection, forcing a break in prosthesis use.
Doctors should encourage patients to report every sign—no matter how small. What looks trivial to them may be the body’s first whisper of distress.
Consistent blood sugar checks and periodic hemoglobin monitoring keep the invisible factors of healing under control. If energy levels dip or swelling returns, a nutritional or circulatory reassessment may be required.
As patients regain mobility, the body’s energy needs rise again. This can cause fluctuations in blood sugar or minor weight changes. Physicians must preemptively guide dietary and medication adjustments to match this new rhythm.
Encouraging gentle physical activity beyond rehabilitation—such as walking short distances, light stretches, or home chores—helps keep metabolism and morale balanced.
A moving body heals continuously; a sedentary one risks regression.

Many patients begin strong but slowly relax discipline as comfort increases. Missed glucose checks, skipped medications, or reduced hydration start to creep in. The skin, deprived of internal balance, begins to show minor irritation or inflammation.
This is the relapse cycle physicians must guard against. Prevention doesn’t require new treatments—only vigilance.
A quick monthly teleconsultation or message check-in often keeps patients accountable. It reminds them that care doesn’t end with fitting; it simply becomes maintenance.
A simple model works well:
At each visit, doctors should reassess wound condition, blood sugar trend, hydration status, and overall nutrition. Small corrections at these intervals prevent large problems later.
Even after full recovery, circulation can remain compromised if activity levels fall or weight increases. Reassessing cardiovascular health once a year keeps the body ready for any future socket modifications or replacements.
If new swelling or numbness appears, doctors should consider Doppler testing to rule out hidden venous issues. Early detection saves months of regression.
Many patients abandon compression once the prosthesis fits comfortably. But mild compression worn for a few hours daily helps maintain limb shape, reduce edema, and improve socket comfort.
Physicians can reintroduce compression therapy intermittently, especially during hot seasons when swelling is common.
Every successful rehabilitation ends with the patient taking full ownership of their health. Doctors who teach self-monitoring, basic limb inspection, and daily care rituals empower patients to manage themselves long after discharge.
Patients should know how to clean the limb, recognize infection, track sugar, and keep a balanced meal plan—all without waiting for reminders.
Knowledge creates security, and security builds confidence.
Instead of dictating routines, physicians can ask reflective questions:
Questions like these spark awareness. The patient becomes a participant, not a passive receiver of advice.
Each milestone—whether it’s a week of stable sugar, a new walking distance, or a healthy scar—should be celebrated. Recognition reinforces discipline.
Physicians who praise progress plant hope. Hope fuels compliance better than any medication ever could.
At its core, faster socket readiness depends on three tightly linked systems:
When one weakens, the others strain to compensate. When all three align, progress feels almost effortless.
Each lever influences the others. Stable sugar supports healthy blood flow; good circulation improves nutrient delivery; proper nutrition stabilizes glucose and enhances vascular function.
This loop isn’t just biological—it’s behavioral. Patients who internalize this connection rarely regress.
Initially, doctors lead the process. But as healing matures, control should shift gradually to the patient. The best outcomes happen when medical management turns into personal habit.
The physician remains a guide, stepping in only when the system drifts.
Some teams push for early socket fitting to show quick results. But premature fitting over an unstable wound, swelling, or fluctuating sugar almost always backfires.
The result is a poor fit, pain, and discouragement. Physicians should insist on meeting all readiness criteria before approval, even if it adds a few weeks. The long-term gain outweighs the short delay.
Recovery isn’t just physical—it’s mentally draining. Patients may appear compliant but feel quietly overwhelmed. Skipped meals or inconsistent monitoring often reflect burnout, not neglect.
Regular, empathetic conversations can uncover hidden fatigue before it turns into medical regression. A few minutes of listening often save weeks of healing time.
The intact limb bears double the work during recovery. Neglecting its care leads to strain, swelling, or even ulceration. Physicians should include both limbs in every checkup.
Balanced muscle health ensures long-term mobility and prosthetic success.

If the wound reopens, sugar spikes, or swelling returns, it’s not failure—it’s feedback. The body is signaling imbalance.
Doctors should calmly return to the basics:
Once the problem stabilizes, a new healing cycle begins—shorter and smoother than the first.
When the doctor stays calm during setbacks, the patient learns resilience. Each recovered setback builds mental strength.
In prosthetic care, confidence is as healing as any antibiotic. It helps patients endure the process and keep moving forward.
After the prosthesis becomes a natural extension of the body, health routines must evolve from treatment into lifestyle.
Simple, local foods. Regular movement. Stable sleep. Periodic check-ins. These are the quiet pillars that sustain long-term success.
Physicians who frame these routines as empowerment, not obligation, help patients carry them with pride.
Peer groups or rehabilitation communities play a powerful role in sustaining habits. Patients learn from one another, share struggles, and celebrate progress.
Doctors can recommend trusted support groups or local mobility clubs. Seeing others thrive renews motivation more than any lecture ever can.
Even years after recovery, annual or biannual checkups with the physician help reset goals. Sugar patterns can drift, weight can change, and lifestyle factors evolve.
These refreshers act like tune-ups—keeping the engine of health running smoothly.
In the race to fit a prosthesis, physicians often focus on surgical precision and device technology. Yet, the quiet forces—glucose control, clot prevention, and nutrition—decide the true pace of recovery.
Every well-timed insulin adjustment, every hydration reminder, every protein-rich meal speeds up readiness more than any high-end device alone.
Physicians hold the science; patients hold the will. When both meet halfway—with clarity, consistency, and care—the body follows naturally.
The socket fitting becomes not an end point, but a symbol of teamwork between biology and belief.
At Robobionics, we see prosthetic fitting not as a mechanical milestone but as a human transformation. Our mission is to make that transformation smoother, faster, and safer for every individual.
Through close collaboration with physicians, physiotherapists, and patients, we aim to help every person regain independence with dignity.
Whether it’s glycemic stability, circulatory safety, or nutrition support—we believe every detail matters. Because every small improvement adds up to one big outcome: a life back in motion.

For many clinicians, the surgery is only the first step. What happens after the operation

For trauma amputees, the journey does not begin at the prosthetic clinic. It begins much

Amputation after cancer is not just a surgical event. It is the end of one

When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.