Outcome measures matter. They help doctors, therapists, and care teams truly understand how a person is doing after getting a prosthetic hand or arm. They also help you track progress, spot challenges early, and make sure every patient receives the right care at the right time. In India, where access, budgets, and follow-ups can be very different from patient to patient, clear outcome tools become even more important.
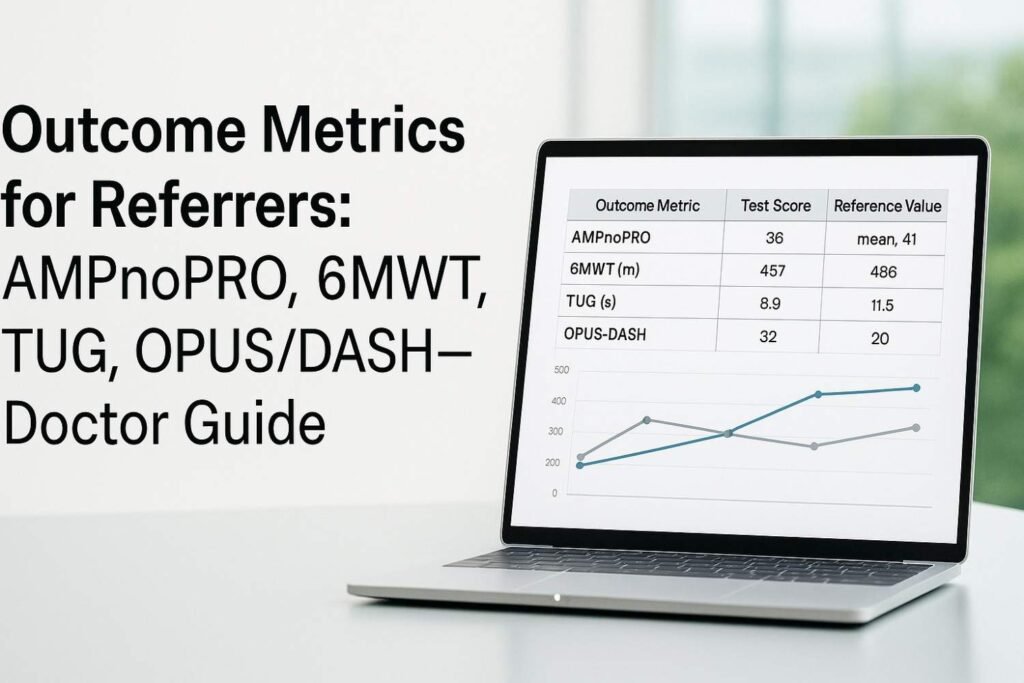
Many referrers we work with tell us the same thing: they want simple ways to measure results without long forms, confusing language, or tests that take too much time. They want tools that are trusted, easy to repeat, and meaningful in real clinical settings. This guide brings clarity to four important outcome measures you can use with upper-limb prosthetic users: AMPnoPRO, 6-Minute Walk Test (6MWT), Timed Up and Go (TUG), and OPUS/DASH. We explain them in plain words, show when each test helps, and share how they guide better decisions for your patients.
AMPnoPRO
What AMPnoPRO Really Measures
AMPnoPRO is a simple test that helps you understand how well a person moves without wearing a prosthesis. It is often used before fitting an upper-limb or lower-limb device, but for referrers, it also offers a useful view of a patient’s starting point.
The test looks at balance, basic movements, sitting tasks, standing tasks, and small actions that show how confidently the person can control their body. Even though the name looks long, the idea behind it is very simple: it shows how ready the person is for a prosthetic device.
Many doctors see AMPnoPRO as a clean way to understand strength and stability before the prosthesis is introduced. When this score is used early, you get a baseline that can guide the whole rehab journey ahead.
Why AMPnoPRO Helps Referrers Make Better Choices
AMPnoPRO helps you spot things that may slow down training. Some patients may be strong but lack balance. Some may have good balance but get tired fast. Some may have good control but struggle with posture.
This test shows these gaps in a clear way. When you know the gap, you know how to help. You can plan early physiotherapy, muscle activation training, or simple home routines that prepare the patient for a better prosthetic outcome.
When used well, AMPnoPRO can prevent delays because you can prepare the patient before the fitting process starts. Patients who enter the process with stronger basics often learn faster, adapt faster, and stay motivated.
When AMPnoPRO Is Most Useful in Upper-Limb Cases
While AMPnoPRO is widely used in lower-limb settings, it still gives value to upper-limb referrers. Many upper-limb amputees still struggle with trunk balance, shoulder posture, and core strength, especially after long periods of compensation.
By checking balance and mobility patterns early, you can identify small weaknesses that may affect prosthetic training—like shoulder lift, reach range, or uneven rotation patterns. Early detection leads to targeted rehab, and targeted rehab leads to smoother myoelectric training later.
How to Use AMPnoPRO Results in Your Practice
Once you have the score, break it into sections rather than looking at the total number. Each section hints at a different area of strength or weakness.
The sitting section helps you see trunk stability.
The standing section shows postural control.
The step and balance tasks show how confidently the patient moves.
Use these details to build a simple plan. These plans can be shared with physiotherapists or rehab centers so the patient receives a unified care experience. When everyone works with the same score and plan, the outcome becomes stronger.
If your clinic deals with many new amputees, consider using AMPnoPRO at the very first visit. It creates a clean baseline and sets clear expectations for progress.
6-Minute Walk Test (6MWT)
What the 6MWT Really Tells You

The 6-Minute Walk Test is as simple as it sounds. The patient walks for six minutes, and you measure how far they go. But even though it feels simple, it tells you a lot about endurance, gait quality, confidence, and overall function.
In prosthetic care, walking distance often gives clues about strength, cardiorespiratory fitness, pace control, and fatigue levels. Even for upper-limb users, the test can show how posture and arm swing affect balance.
Because the test is based on natural walking, it is easy to repeat during follow-ups, and it produces meaningful data without special tools.
Why Doctors Prefer the 6MWT for Tracking Progress
One reason referrers like the 6MWT is that it reflects real life. Patients need to walk in their daily routine—at home, at work, outdoors, or during travel. A six-minute walk shows how well they manage everyday movement.
If the distance improves over time, it usually means strength and confidence are growing. If the distance drops, it may mean there is pain, discomfort, weakness, or an issue with the prosthesis.
The test also gives you a simple way to compare recovery at different stages. A patient might start small, then grow steadily after fitting, after training, and after daily use of the prosthesis. Seeing the curve go up keeps the patient motivated and helps you plan the next steps.
When the 6MWT Is Most Useful for Upper-Limb Amputees
Upper-limb amputees often change their walking patterns. Loss of arm swing on one side can shift balance, change posture, or increase fatigue. Some people also lean or rotate the body more while walking.
The 6MWT captures these small changes because fatigue shows up early. If the patient becomes tired fast, you know there is a strength or posture issue. If the pace keeps dropping, you know a muscle group is overloaded or underused.
These details can help you recommend simple exercises, gait training, or posture correction before the prosthesis training begins. This approach leads to fewer complications later.
How to Use the Data for Better Prosthetic Outcomes
Write down not only the distance but also how the patient moves. Observe their posture, pace, step length, and any visible discomfort. These small things matter because prosthetic success depends on full-body coordination.
Record the score neatly and compare at future visits. A steady improvement is always a good sign. A sudden drop is your signal to check for pain, socket fit issues, or fatigue. When you act early, the patient stays comfortable and engaged.
If your clinic works with many rural patients, use the 6MWT because it needs no machines, only clear walking space. This keeps the process simple, affordable, and accessible to everyone.
Timed Up and Go (TUG)
What the TUG Test Measures in Real-Life Movement
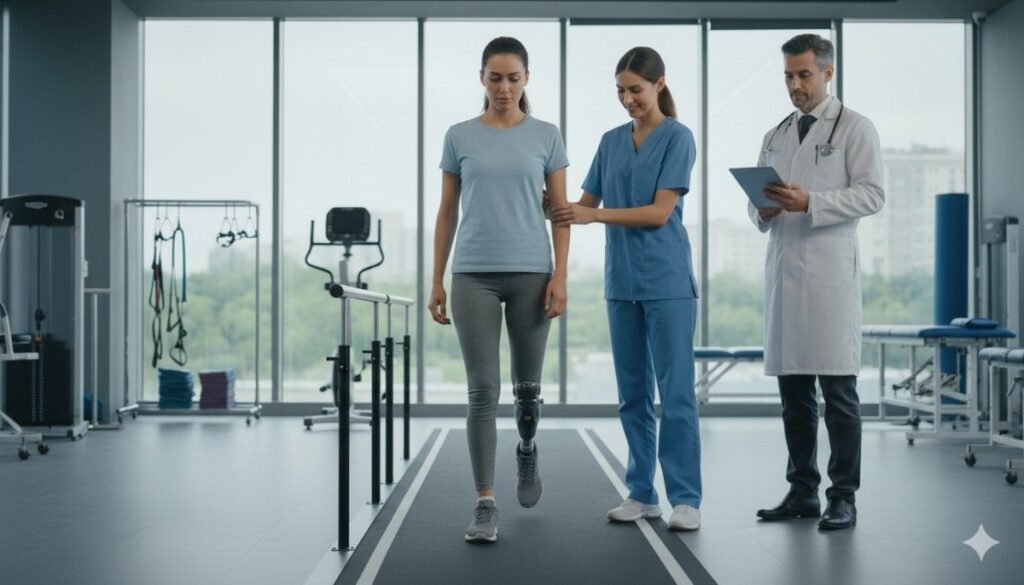
The TUG test checks how fast a person can stand up, walk a short distance, turn around, walk back, and sit down. This entire action shows balance, confidence, and how smoothly the body handles quick shifts between tasks.
Even though upper-limb users do not depend on leg function, the test still tells you a lot about how their body works as one unit. Many arm amputees adjust their posture or lean while doing daily tasks, and the TUG test brings these changes to light.
Why the TUG Test Matters for Prosthesis Readiness
The TUG score acts like a window into how safely someone can move in everyday life. A slow score often means the person is cautious, tired, or experiencing discomfort somewhere in the body. A fast score means good control and confidence.
For referrers, this score helps in planning when the patient is ready for prosthetic training. Someone who can move smoothly will pick up myoelectric control faster. Someone who struggles may require basic rehab first.
The TUG test also helps you predict fall risk. Even for upper-limb cases, imbalance or sudden fatigue can lead to unsafe movement. When you spot these risks early, you can guide the patient to safe exercise routines.
How the TUG Measures Adaptation After Fitting
Once the prosthesis is fitted, the TUG score usually improves. This is because balance becomes more natural when the body feels complete on both sides. The shoulder, spine, and pelvis begin to align better with regular use.
If the score does not improve, or if it becomes slower, it may show discomfort from the prosthesis, poor fitting, muscle weakness, or compensatory patterns in the upper body.
Tracking the TUG at regular intervals helps you maintain clear visibility on the patient’s progress. It also gives you a simple language to discuss goals with the patient.
Using the TUG Test in Rural and Busy Clinics
The TUG test takes less than two minutes and requires only a chair and a few meters of walkway. Because of this simplicity, many referrers use it during packed clinic hours or in rural screening camps.
The score is easy to explain to patients. You can say, “Your time today was this, and we want it to reach this.” These simple benchmarks help patients stay committed to their exercise routines.
If your clinic handles many referrals, using the TUG test as a routine screen can help you quickly identify which patients need more attention.
OPUS and DASH
What OPUS and DASH Really Measure
Both OPUS and DASH are questionnaire-based tools. They capture how a person feels about their upper-limb function in daily life. These tests focus on simple things—reaching, holding, lifting, pulling, writing, grooming, and other tasks that make life easier.
Unlike movement tests, these tools measure satisfaction, comfort, and confidence. They show how well the prosthesis fits into the patient’s lifestyle, not just how well the patient performs in a clinic setting.
Doctors who use these tools get a clearer picture of the patient’s real-life challenges and emotional experience.
Why Patient-Reported Outcomes Are Important
Many referrers forget that function is not only physical. A prosthesis may look perfect in clinic tests but may feel heavy, tiring, or inconvenient at home. Sometimes the issues are small but annoying—like difficulty tying threads, holding small objects, or lifting certain items.
OPUS and DASH reveal these concerns. When the patient fills these forms honestly, you can understand what needs improvement. You may need to adjust training, correct fitting, or teach better grip patterns.
These tools also help track emotional comfort. Some patients may be shy using their prosthesis in public. Some may not feel confident yet. These emotional elements matter deeply in long-term use.
How to Use OPUS and DASH in Follow-Up Care
The best way to use these tools is to do them at three stages. First, before fitting. Second, after initial training. Third, during long-term review. This gives you a clear curve showing how the patient’s life improves over time.
If the score jumps quickly after training, you know they are adapting well. If the improvement is slow, you can step in with extra guidance, stronger rehab support, or new strategies for daily tasks.
These tools also help you support family members who want to understand how the patient is doing. When you share the progress curve, it builds trust and improves family participation in care.
Why OPUS and DASH Work Well With Grippy Bionic Hand Users
Many upper-limb users in India choose Grippy because it is light, responsive, and gives better control through myoelectric signals. The Sense of Touch system in our bionic hand also helps users feel objects in a natural way.
OPUS and DASH capture how these features help the user. You can see how tasks become easier and how confidence grows. When the patient reports better grip control or ease in everyday tasks, you know the technology is doing its job.
These questionnaires become a powerful tool to show real-world outcomes for advanced prosthetics.
How These Tests Work Together
Seeing the Full Picture of a Patient’s Function
When referrers use AMPnoPRO, 6MWT, TUG, and OPUS/DASH together, something powerful happens. You start seeing the patient from many angles instead of just one. Each tool shows a different part of their journey, and together they form a clear picture of readiness, progress, and comfort.
One tool may show balance. Another shows endurance. A third shows confidence. A fourth shows daily life struggles. When all these details come together, decision-making becomes smoother and more accurate.
This also helps you guide the patient in a way that feels personal and thoughtful. Instead of general advice, you give targeted steps that create real change.
Why One Test Alone Is Not Enough
Many doctors rely only on walking tests or only on patient feedback. But when only one part of the story is visible, you may miss something important. A patient may walk well but feel unhappy with their prosthesis. They may feel confident but struggle with fatigue after a few minutes of walking. They may have great balance but poor trunk stability.
Each test fills a gap left by another test. That is why using all four gives you a balanced view. This balanced view leads to better fittings, better rehab plans, and better safety for the patient.
How Combining Tests Improves Prosthetic Training
Prosthetic training becomes easier when you know exactly what the patient needs. If AMPnoPRO shows weak core strength, you can work on posture before training. If 6MWT shows poor endurance, you can adjust early exercise. If TUG shows slow turns, you can improve balance. If OPUS/DASH shows low confidence, you can introduce smaller daily tasks first.
By adjusting care based on real data, you reduce frustration for the patient. They feel seen, understood, and supported. This emotional comfort makes learning any advanced prosthetic—like Grippy—faster and smoother.
How These Tests Help in Long-Term Care
These tests also help you during long-term follow-ups. Over months and years, the patient’s needs change. Their lifestyle changes. Their strength changes. Their prosthetic goals also change.
When you retest regularly, you see patterns clearly. You can catch early signs of discomfort, muscle fatigue, posture shifts, or drop in strength. These early signs help you adjust the plan before the problem becomes bigger. This keeps the prosthesis comfortable and useful for many years.
Role of These Metrics in Indian Clinical Settings
Making Outcome Measures Practical for Busy Clinics
Many Indian referrers face shortage of time, staff, and space. Some clinics are crowded. Some are in rural areas. Some doctors travel for camps. Because of these realities, outcome tests must be simple, quick, and meaningful.
AMPnoPRO, 6MWT, TUG, and OPUS/DASH all meet this need. They do not need machines. They do not need special training. They do not need expensive tools. Only space to walk, a chair, a stopwatch, a pen, and a simple form.
This makes these tests perfect for Indian settings where practicality always matters.
Making Outcome Tracking Affordable for Patients
Most patients in India live on limited budgets. Many travel long distances for appointments. Many cannot afford long rehab programs. This makes it even more important to know exactly what they need and when.
Using these tests helps you avoid unnecessary visits and unnecessary delays. You can focus on what gives the highest impact first. Patients appreciate this approach because it saves time, money, and stress.
When families see progress recorded through simple numbers or short forms, they also feel more confident about the journey.
Why Standardized Testing Builds Trust
Referrers who use outcome measures appear more reliable to patients and families. When you show them scores, improvements, and clear patterns, they feel reassured. They trust your plan because they see proof, not guesses.
In India, where many families worry about the cost of prosthetics, transparency becomes a powerful tool. These tests help you explain why a prosthesis is needed, when training should start, and how the patient is improving over time.
Trust grows faster when the family sees data that is simple and easy to understand.
Using Outcome Scores for Insurance and Government Programs
Many states and support schemes now ask for proof of medical need before funding a prosthesis. Outcome scores act like a strong foundation for these requests. They show the patient’s condition before and after fitting. They show improvement. They show need for ongoing rehab.
Having documented scores makes your case stronger. This helps families secure support from programs such as government disability benefits or workplace insurance claims.
Outcome measures also help hospitals and NGOs maintain clean records that match newer guidelines for medical documentation.
How Referrers Can Implement These Tests Easily
Creating a Simple Testing Workflow
The easiest way to start is to set a small workflow that fits your clinic. You can keep a simple sequence like this:
Start with AMPnoPRO to check early stability.
Then do the 6MWT to measure endurance.
Next, do the TUG to observe quick movement.
End with OPUS or DASH to understand daily life and emotions.
This neat flow takes little time but gives rich information about the patient. Once you set this routine, your staff can follow it smoothly.
Training Staff to Conduct These Tests
Most tests need no special training, but it helps to teach your assistants how to watch posture, pace, and body movements. They should learn how to time the TUG, measure walking distance, and help the patient fill OPUS or DASH.
You can also keep small printed sheets for each test. This helps the whole team stay consistent. Over time, your clinic will build a strong database of outcomes for all patients.
When more than one staff member uses the same method, the reliability of your tests becomes much stronger.
Keeping Records Clean and Clear
Every test should be recorded on the same day. Write the date, score, and short notes. Store everything in the patient file in a simple sequence. You may use a digital sheet or paper file—both work well.
Clear records make follow-ups easier. You can flip through old scores and compare them in seconds. This quick comparison helps in decision making, especially when patients come after long gaps.
It also lets you notice slow improvements or sudden drops early.
Making the Testing Experience Friendly for Patients
Many patients feel nervous during tests. Some worry about being judged. Some worry they will fail. Some feel embarrassed if they move slowly.
A friendly approach helps them relax. Speak gently. Explain why each test matters. Tell them that the goal is not to judge but to understand. When patients feel comfortable, their performance becomes more natural. Natural performance gives more accurate scores.
A calm, kind environment also builds trust and improves long-term engagement.
How These Tests Support Prosthetic Selection
Matching Test Results to Prosthetic Needs
No two patients are the same. Some need a simple mechanical hand. Some need a myoelectric device. Some want high fine-motor control. Some focus on daily chores. Some need strong grip for work.
When you read all test scores together, you understand what type of device fits their needs. For example:
If AMPnoPRO shows poor trunk stability, lightweight devices help.
If 6MWT shows quick fatigue, energy-efficient designs help.
If TUG shows balance issues, symmetrical weight distribution helps.
If OPUS/DASH shows desire for fine-task control, advanced bionics help.
This matching of data to device makes your recommendation stronger and more accurate.
Why This Matters for Grippy Bionic Hand Users
Grippy is light, responsive, and built for natural movement. It uses myoelectric signals and provides tactile feedback through Sense of Touch technology. This design reduces effort and increases comfort.
When you match test scores to these features, you know exactly which patients will benefit the most. Many users who score low in confidence but high in motivation respond well to Grippy because it makes daily tasks easier.
Patients with shorter residual limbs also benefit because Grippy needs very little force to operate. Outcome tests help you spot these ideal candidates early.
How Tests Influence Fitting and Alignment
Outcome scores also help with socket design, suspension type, and alignment. For example:
If the 6MWT shows fatigue on one side, check if weight distribution is even.
If TUG shows slow turning, assess shoulder alignment.
If OPUS/DASH shows discomfort during overhead tasks, adjust cable routing or electrode placement.
These adjustments improve comfort and long-term satisfaction.
Outcome measures turn fitting from guesswork into a guided, informed process.
Using Outcome Measures to Strengthen Follow-Up Plans
Creating Clear Milestones for the Patient
Patients feel motivated when they know what to expect. When you set small targets—like improving 6MWT distance or improving TUG time—they get something concrete to work toward.
These small wins create steady motivation. Patients start feeling proud when they see numbers improving. This emotional lift plays a big role in prosthetic success.
With clear milestones, they also take rehab more seriously because they know the purpose behind every exercise.
Helping Patients Understand Their Own Progress
Many patients underestimate their progress. They may feel nothing is changing even when they are improving. Showing them the scores helps break this doubt.
You can show them how their AMPnoPRO score improved after early exercises. You can show how their walking distance increased. You can show how their TUG time reduced. You can show how their OPUS/DASH answers shifted from difficulty to ease.
When they see this growth, they gain confidence and continue using their prosthesis with joy.
Supporting Long-Term Engagement
Follow-ups often drop after the first few months. Patients may get busy. Some may lose motivation. Some may think everything is fine and skip visits.
Using outcome measures gives you a structured reason to call them back. You can say, “It’s time to check your progress again.” Patients understand this better than vague follow-ups.
Regular scores help you maintain long-term care, ensuring the prosthesis remains useful and comfortable for years.
Practical Tips for Each Outcome Measure
Making AMPnoPRO Easy to Use in Daily Practice

AMPnoPRO becomes very simple once you get used to the flow. One helpful way to begin is by giving the patient a short explanation before starting. Tell them the test helps you understand their body control before prosthetic training. This helps them relax and perform naturally.
During the test, watch how smoothly the patient shifts weight, how steady their trunk looks, and how comfortable they feel with each small movement. These small observations often tell you more than the score itself.
Encourage the patient gently through each step. Many lose confidence when they struggle with a movement. A calm voice helps them stay focused. After the test, explain in simple words what the score means and how early exercises can help improve their readiness for a prosthesis.
Making the 6MWT More Meaningful for Your Patients
The 6MWT should feel natural, not rushed. Before starting, make sure the walkway is clear. Ask the patient to walk at a pace they feel comfortable with. Do not pressure them to walk faster than normal.
As they walk, observe their shoulder posture, trunk rotation, and arm swinging pattern. Upper-limb amputees often change their walking style to compensate for the missing limb. These changes show up clearly during this test.
Write down not only the final distance but also any visible fatigue, wobbling, or slowing near the end. These details help you guide the patient later. When you compare distances over time, you can show them how their endurance improves with consistent training.
Tips for Getting Reliable TUG Scores
For the TUG test, place the chair against a wall so it stays steady. Ask the patient to move at a comfortable speed. Tell them they do not need to rush. The goal is smooth movement, not a race.
Watch their balance when they stand. Watch how they turn. Watch if their steps become uneven as they get tired. These details show how confident and stable they feel.
If the patient moves slowly or hesitates, reassure them. Make the environment warm and supportive. A stressed patient may move unnaturally, giving you inaccurate results. A relaxed patient gives the truest score.
Helping Patients Answer OPUS or DASH Honestly
OPUS and DASH work only when the patient answers honestly. Take a moment to explain that these forms help you understand their comfort and daily challenges. Tell them there are no right or wrong answers.
Some patients feel shy to admit difficulty. Some feel proud and say everything is fine even when it is not. Encourage them to speak openly. Remind them that honest answers help you improve their training and prosthetic experience.
If needed, read the questions aloud. Many patients, especially in rural areas, do not feel comfortable reading long forms. Reading aloud helps them understand better and respond clearly.
Case Scenarios to Guide Your Clinical Decisions
Case 1: A New Upper-Limb Amputee With Weak Core Control
A young patient arrives after recent amputation. Their AMPnoPRO score shows weak trunk stability and poor balance during sitting tasks. The 6MWT distance is short, and the TUG time is slow. OPUS shows they feel anxious about using a future prosthesis.
This combination tells you they need early core strengthening before prosthetic training. Even a simple program of guided breathing, trunk activation, and shoulder mobility can help. When strength improves, prosthetic training becomes much smoother.
This case also shows you that emotional reassurance is important. Early counselling and simple guidance help build trust.
Case 2: A Patient With Good Movement but Low Confidence
Another patient moves well. AMPnoPRO looks balanced. 6MWT distance is strong. TUG is quick. But OPUS and DASH show low confidence and fear of using a device in public.
This case requires emotional support more than physical rehab. Introduce small daily tasks. Give them simple goals like holding a cup or lifting small objects. Celebrate small wins with them. Show them how each task matters.
With support, their confidence grows, and their OPUS/DASH score improves even without major physical changes.
Case 3: A Patient Who Shows Good Progress Then Suddenly Declines
Some patients start strong. Their scores improve for weeks. Then one follow-up shows a sudden drop in 6MWT or a slower TUG. OPUS shows discomfort in a few tasks that were easy earlier.
This drop is a signal. Maybe there is socket discomfort. Maybe a new posture issue. Maybe stress or fatigue. Maybe they stopped home exercises.
This is your chance to step in early. Make small fitting adjustments or refresh their rehab plan. These small corrections prevent long-term problems and help them return to their earlier progress.
Case 4: A Patient Who Needs to Return to Heavy Physical Work
Many Indian amputees work in jobs that demand strength, lifting, or long hours of movement. These patients may score well on early tests but show fatigue during 6MWT or hesitation in OPUS/DASH when it comes to tough tasks.
This combination helps you design special training for work tasks. Heavy users need strong shoulders, stable trunk muscles, and good endurance. You can plan their rehab accordingly. Their progress becomes smoother, and their return to work becomes safer.
How Outcome Metrics Improve Communication Between Teams
Helping Doctors, Therapists, and Prosthetists Work Together
Outcome measures become a shared language among care teams. Doctors, physiotherapists, prosthetists, and counselors can all read the same scores and understand the patient in the same way.
This avoids confusion. It prevents repeated tests. It makes decision-making faster. Everyone works with the same data, which keeps the care plan clear and organized.
For example, if AMPnoPRO shows weak core strength, the therapist knows what to focus on. If OPUS shows difficulty in handling small objects, the prosthetist knows what grip patterns to train. If TUG shows slow turning, the doctor knows balance needs attention.
Helping Families Understand the Journey
Most families want to help but do not know what to expect. Showing them test scores makes everything clearer. They see what the patient is working on. They see what improvements look like. They understand why some tasks take time.
This understanding helps them support the patient with patience and hope. It also prevents misunderstandings or unrealistic expectations.
When the family feels included, the patient receives stronger emotional support at home, which improves long-term results.
Helping Patients Feel Involved in Their Care
Patients feel more in control when they understand their scores. When you explain what each test means, they feel like active partners in their own care. They start taking rehab seriously. They start asking questions. They start noticing changes in their own body.
This sense of involvement improves commitment. They begin to see the prosthesis not as a device but as a part of their growth. When emotional engagement grows, physical progress follows.
The Role of These Metrics in Long-Term Prosthetic Success
Preventing Harmful Compensation Patterns

Many amputees unknowingly use harmful compensation patterns. They may shift weight to one side, rotate the body, or lift their shoulder too high. Over time, this leads to pain, stiffness, and poor alignment.
Outcome measures like TUG and 6MWT reveal these patterns early. When you catch them early, you can correct them with simple exercises. This prevents long-term issues that often appear months or years after fitting.
Correcting patterns early protects the patient from chronic discomfort.
Maintaining Proper Fit Over Time
The human body changes. Muscle mass changes. Weight changes. Skin condition changes. When these changes happen, the prosthesis may start feeling loose, tight, or uncomfortable.
Regular outcome checks help you spot these changes quickly. A drop in 6MWT, slower TUG, or new complaints in OPUS/DASH may all signal fit issues. When these signals appear, you can adjust the socket or alignment before the discomfort becomes severe.
This keeps the prosthesis comfortable and usable for a long time.
Supporting Large-Scale Data Tracking in Clinics
If your clinic sees many patients, tracking their scores over time builds a large database. This helps you predict patterns, plan services, and improve your care model.
You can see which rehab steps work best. You can see which devices perform best. You can see what challenges are common in your region. This helps in training new staff and planning future improvements.
Outcome data becomes a tool for both individual care and overall clinic growth.
Why Outcome Measures Matter for High-Quality Prosthetic Care
Bringing Clarity to Complex Decisions
Prosthetic care involves many choices—device type, socket design, training steps, rehab plans, follow-up timelines. Outcome measures make these decisions clear because they show real needs, not assumptions.
When you rely on scores, you reduce guesswork. Each step becomes guided, structured, and logical. This increases the likelihood of success.
A clear process means smoother fitting, faster learning, better comfort, and improved daily life for the patient.
Building a Culture of Quality and Accountability
When clinics use outcome measures regularly, they build a culture of quality. Every patient gets measured. Every decision gets documented. Every improvement gets tracked.
This culture improves trust among patients, families, and partners. It also helps your clinic stand out as a center that values transparency and measurable success.
In India, where prosthetic access varies widely, being a data-driven clinic becomes a strong advantage.
Strengthening the Patient–Provider Relationship
Most patients seek more than a prosthesis. They want reassurance. They want guidance. They want someone who understands their struggles and helps them grow.
Outcome measures strengthen this relationship because they show you are paying close attention. When you discuss scores with kindness and clarity, patients feel respected and valued. They trust your words because they see the proof behind them.
Trust is the base of long-term success in prosthetic care.
Bringing It All Together for Better Patient Outcomes
How These Four Measures Create a Strong Clinical Foundation
When AMPnoPRO, 6MWT, TUG, and OPUS/DASH are used together, they give you a complete view of the patient’s physical and emotional well-being. Each test adds a small but important piece to the story. You see how the patient moves, how stable they are, how long they can stay active, and how they feel during daily life tasks.
This mix of physical performance and personal feedback creates a rich, balanced picture. It helps you set clear goals and provide care that feels thoughtful and specific to each patient. In the long run, this leads to stronger outcomes, greater comfort, and a smoother rehab journey.
Why Simplicity Matters in Outcome Tracking
Many clinicians worry that outcome measures will take too much time or feel too complex. But these four tests stay simple by design. They use natural human movement. They rely on honest patient feedback. They require very few tools.
The simplicity of these tests is what makes them powerful. Patients understand them. Families understand them. Your team understands them. Because of this clarity, they become easy to repeat during every visit. Over months and years, these repeated scores form a clean line of progress that tells the true story of the patient’s journey.
How These Measures Help You Push for Better Standards
When you use structured outcome measures, you automatically raise the standard of care in your clinic. Each test shows your commitment to evidence-based practice. It also shows that you care about long-term success, not just short-term fitting.
This approach sets your clinic apart. It shows patients and partners that you value accuracy and transparency. It also helps you document your outcomes for future quality checks, audits, or research. With time, your clinic becomes known not just for services, but for reliable and proven results.
Using Outcome Measures for Better Patient Motivation
Turning Scores Into Small, Achievable Goals
Patients often feel overwhelmed in the early phases of prosthetic care. New movements, new sensations, and new habits can feel challenging. But when you show them simple scores with small improvement targets, the journey becomes easier.
You can say, “Our next goal is to improve your walking distance,” or “Let’s try to reduce your TUG time by a few seconds.” These small goals feel manageable. They reduce anxiety and keep the patient focused. Every small success builds confidence. This confidence spreads into training, daily tasks, and social interactions.
Celebrating Improvements Openly
When a patient improves even a little, it is worth celebrating. Show them how their AMPnoPRO score moved upward. Show them how the 6MWT distance grew. Show them how they now take fewer seconds for the TUG. Show them how their OPUS/DASH answers shifted toward comfort.
These improvements make the patient feel proud. When they feel proud, they try harder. When they try harder, they progress faster. A positive cycle forms naturally.
Sometimes, even small changes can make a big emotional difference. A patient who sees their score improve feels stronger, more hopeful, and more connected to their future.
Keeping the Patient Engaged During Long Gaps
Many Indian patients travel from villages, towns, or far-off districts. Long gaps between visits are common. Outcome measures help bridge this gap. They act like checkpoints in the journey.
When you call a patient for a review, you can say, “It’s time to check your scores again.” This gives a clear purpose for the visit. Patients understand why they must come back. It reduces no-shows and improves long-term engagement.
Some clinics even ask patients to track simple activities at home. This adds another layer of involvement and keeps motivation alive.
Practical Use of Outcome Scores in Grippy Bionic Hand Care
Building Personalized Training Plans

Grippy is designed to adapt to the user’s natural muscle signals. But the learning curve becomes smoother when you match the training plan to the patient’s outcome scores.
If AMPnoPRO shows weak shoulder stability, early training can focus on simple shoulder control before myoelectric activation. If the 6MWT shows fatigue, training sessions can be shorter at first. If TUG shows slow turning, you can add small balance exercises. If OPUS/DASH shows difficulty in fine tasks, you can introduce assignment-based training like picking up coins or tying threads.
These small adjustments tailor the training to the patient’s exact needs. This helps them learn faster and feel more confident with their Grippy hand.
Reducing Early Frustration Through Clear Benchmarks
Many prosthetic users feel frustrated during the first few weeks of training. They may feel clumsy or slow. But when you show them outcome numbers, expectations become clearer.
You can tell them, “Your early goal is to improve grip control by focusing on these specific movements,” or “We want your OPUS score to shift in these two tasks.” Clear benchmarks reduce confusion and bring calmness to the process.
When the patient knows what they are aiming for, they feel more stable emotionally. This emotional stability supports better learning.
Using Outcome Measures to Adjust the Hand or Socket
Outcome measures also guide technical adjustments. If OPUS reports pressure during certain tasks, you can check the socket fit. If 6MWT shows sudden drop in endurance, you can check weight distribution. If TUG shows hesitation during standing, you can check alignment or trimming requirements.
This helps the prosthetic team work smarter. Instead of guessing what might be wrong, they use the data to identify the cause. Adjustments become faster and more accurate.
Over time, this improves patient comfort and device usability.
Making Outcome Measures Part of Every Referral
Standardizing Assessments Across Partner Clinics
If your clinic refers patients to prosthetic centers often, having a standard outcome set helps create a common language between both sides. You can share AMPnoPRO, 6MWT, TUG, and OPUS/DASH scores with the prosthetic team.
This makes the transition smooth. The prosthetic team understands the patient from day one. They know what exercises were done. They know what challenges were faced. They know the emotional readiness of the patient.
Standardized assessments also improve collaboration because everyone follows a clear method.
Improving Referral Quality Through Clear Documentation
Clear outcome scores strengthen your referral notes. Prosthetic centers appreciate detailed information because it helps them design a better plan. It saves time. It reduces repeated tests. It shows the seriousness of your clinical approach.
Your documentation also becomes useful if the patient applies for financial help, government support, or insurance claims. Clean records and clear numbers make the process smoother.
Over time, you build a reputation as a referrer who sends well-prepared patients. This improves your network and patient trust.
Helping Patients Travel With Confidence
In India, many prosthetic users travel across states to reach advanced centers. A set of outcome scores gives them confidence because they feel prepared. They know what their challenges are. They know what they need to ask. They know what progress to expect.
This reduces stress and builds trust between the patient and all care teams involved.
The Future of Outcome Measures in Indian Prosthetic Care
Moving Toward Data-Driven Healthcare
India is slowly moving toward data-driven healthcare models. Outcome measures are the first step in this direction for prosthetic care. They make healthcare more organized, more reliable, and more focused on long-term results.
As more clinics adopt these measures, the quality of prosthetic care will rise across the country. Patients will benefit from more structured, predictable, and research-backed programs.
This also helps the prosthetic industry grow stronger because data shows what works and what needs improvement.
Building Stronger Community Awareness
Outcome-based practice also helps you educate your community. You can create awareness programs that explain the value of structured testing. Families and patients appreciate knowing that their care is guided by real numbers, not guesswork.
When more people understand the role of testing, they participate more actively. They follow exercises better. They attend follow-ups more regularly. They ask better questions. This shift changes the entire environment of care.
Increasing Access to Affordable Advanced Prosthetics
As outcomes improve, the demand for better prosthetics grows. More people become aware of devices like the Grippy Bionic Hand. They realize that advanced technology is not just for a few, but accessible and affordable.
This awareness leads to more referrals, more partnerships, and more positive results for patients. It creates a healthier ecosystem where quality care becomes achievable for everyone.
Conclusion
Why These Measures Should Be Part of Every Clinic
AMPnoPRO, 6MWT, TUG, and OPUS/DASH are more than tests. They are powerful tools that help you understand your patient deeply. They guide your decisions. They support your training plan. They create a clear path for the patient’s progress.
When you use them together, you build a strong foundation for long-term prosthetic success. You help your patients move with confidence, adapt with comfort, and live with dignity.
Outcome measures are not just forms and numbers. They are steps toward better care, stronger trust, and brighter futures for people with limb differences.