In prosthetic rehabilitation, every step counts — quite literally. For doctors, tracking those steps isn’t just about watching a patient walk; it’s about measuring how well they’re regaining their independence, confidence, and quality of life.
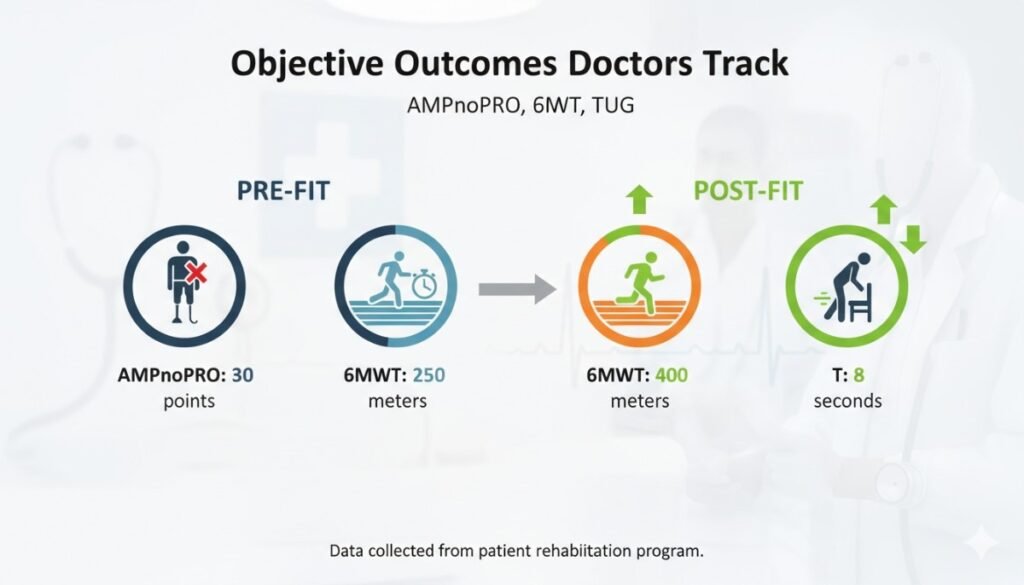
Objective outcome measures like the AMPnoPRO, the Six-Minute Walk Test (6MWT), and the Timed Up and Go (TUG) test help physicians do exactly that. They turn recovery into data, allowing doctors to understand how far a patient has come and what more can be done.
For amputees, especially those using advanced prosthetic limbs, these tests are more than numbers — they’re milestones of progress. From the first step in rehab to walking confidently with a new prosthetic, these evaluations show the transformation that happens when technology and medical science work hand in hand.
In this article, we’ll explore how these outcome measures guide prosthetic care before and after fitting, how doctors use them to personalize treatment, and why they’re essential in building stronger, more confident users of prosthetic technology.
Because when it comes to mobility, progress isn’t just seen — it’s measured.
Why Outcome Measures Matter in Prosthetic Rehabilitation
The Shift from Subjective to Objective Progress

For years, rehabilitation success was often described in vague terms — words like “improving,” “stable,” or “doing better.” While these phrases sound encouraging, they don’t tell the full story.
Objective outcome measures, however, give doctors and therapists a clear, measurable picture of how a patient is truly progressing. These tools turn physical ability into data — showing improvements in balance, endurance, and coordination in a way that can be tracked over time.
They remove guesswork. Instead of relying on observation alone, doctors can now pinpoint exactly where a patient stands before and after prosthetic fitting.
Measuring What Matters Most
What makes these tests powerful is that they focus on what patients care about most — their ability to move confidently in real life.
Whether it’s walking across a room, standing from a chair, or keeping balance on uneven ground, these tests reflect functional ability rather than medical theory.
By using structured assessments, doctors ensure that progress isn’t just happening inside a clinic, but also translating into daily activities. That’s where the true value of prosthetic rehabilitation lies — independence beyond therapy walls.
From Numbers to Narratives
While the data collected is numerical, the meaning behind it is deeply human.
When an amputee who once struggled to take two steps without support completes a six-minute walk test, that number represents months of effort, courage, and adaptation.
These tests become motivational tools too — tangible proof for patients that their hard work is paying off. It’s progress they can see, feel, and be proud of.
Consistency Across Care Teams
Objective measures also bring consistency across healthcare providers. Different therapists, doctors, or prosthetists can interpret results the same way, ensuring coordinated care.
This shared language helps avoid confusion, especially in multidisciplinary teams where surgeons, physiotherapists, and prosthetists work together. Everyone can align around clear data, not assumptions.
For hospitals and clinics, this consistency builds credibility — showing outcomes that can be tracked, compared, and improved upon.
Pre-Fit Evaluation: Laying the Foundation
Why Pre-Fit Testing Is Crucial
Before a prosthesis is even fitted, doctors need to understand the patient’s baseline physical capacity. Pre-fit evaluations reveal the person’s current strength, balance, endurance, and motivation.
Without this data, it’s impossible to design a prosthetic or rehabilitation plan that truly fits the patient’s body and lifestyle. Pre-fit testing also helps identify risk factors, such as poor balance or low stamina, which could lead to falls or slow progress.
In short, it’s like building a map before beginning a journey — you can’t reach the destination without knowing where you’re starting.
Preparing the Body and Mind
Before fitting, the body must be ready. Muscles in the residual limb, trunk, and opposite leg need enough strength to handle weight transfer and balance.
Tests like AMPnoPRO and TUG help identify whether the patient is physically prepared. If not, the focus shifts to targeted exercises — strengthening weak muscles, improving flexibility, and boosting endurance.
But it’s not just about the body. These pre-fit tests also prepare the mind. When patients see measurable goals, they understand that every effort counts, making them more engaged in therapy.
Setting Realistic Expectations
Objective outcomes help doctors and patients have honest, realistic conversations. If the data shows limited stamina or balance, the physician can explain what type of prosthesis or rehabilitation intensity will work best.
This avoids disappointment later. Instead, patients enter the fitting stage with clarity and confidence, knowing exactly what to expect and what’s possible with effort.
Reducing Risks Before Fitting
Pre-fit evaluation is also a safety measure. It identifies issues like joint stiffness, skin problems, or cardiovascular limitations that could make prosthetic use unsafe at first.
Addressing these early — through physical therapy, medical management, or gradual activity — ensures that the fitting process is smoother and safer.
For elderly or diabetic patients, especially, this step can prevent complications and ensure that once the prosthetic is introduced, progress continues steadily.
Understanding AMPnoPRO: Assessing Mobility Potential
What AMPnoPRO Means
AMPnoPRO stands for Amputee Mobility Predictor without Prosthesis. It’s a simple yet powerful test that helps doctors evaluate a lower-limb amputee’s functional ability before fitting a prosthesis.
The “noPRO” part means it’s performed without wearing a prosthesis. This makes it ideal for early rehabilitation stages, right after amputation but before fitting.
It helps answer one of the most important questions in prosthetic care — how mobile can this person be once fitted?
How It Works
The AMPnoPRO consists of 21 tasks that measure balance, coordination, and the ability to move safely with or without support. Patients perform simple activities like standing up from a chair, reaching forward, or maintaining balance.
Each task is scored, and the total gives doctors an objective snapshot of mobility readiness.
The test takes about 10–15 minutes and doesn’t require special equipment — making it practical for hospitals and clinics of all sizes.
What the Scores Indicate
Scores from the AMPnoPRO help classify patients into different functional levels, from limited household ambulation to full community walking.
For example, a low score may indicate the need for strengthening before prosthetic fitting, while a higher score may show readiness for immediate prosthetic training.
This classification guides doctors and prosthetists in choosing the right type of device and therapy intensity. It ensures no one is under-challenged or overburdened.
Why Doctors Value It
Physicians appreciate AMPnoPRO because it connects clinical observation with measurable outcomes. It’s quick, safe, and gives a clear idea of what to expect post-fit.
It’s especially useful for new amputees who may not know what’s achievable yet. The test builds a baseline — a starting point doctors can compare against future progress.
It also provides reassurance. When a patient scores higher over time, it’s evidence that rehabilitation and prosthetic training are working.
The Human Side of Numbers
Behind every AMPnoPRO score is a personal story — a patient learning to stand tall again after surgery, regaining trust in their body, and proving that strength doesn’t depend on having two legs but on courage.
Doctors who take time to explain what the numbers mean help patients see these results as victories, not judgments. It keeps motivation high and spirits steady.
AMPnoPRO and Personalized Rehabilitation
Because every patient is different, AMPnoPRO helps tailor rehabilitation plans precisely.
If a patient struggles with standing balance, exercises focus on posture and trunk control. If coordination is weak, therapists might include stepping or reaching tasks.
This personalization ensures therapy time is effective and relevant — no wasted effort, no guesswork.
The Pre-Fit to Post-Fit Transition
AMPnoPRO is typically used before prosthetic fitting, but it lays the foundation for later comparisons. Once the prosthesis is fitted, the same patient can perform AMP with prosthesis (AMPpro).
Comparing AMPnoPRO and AMPpro results helps doctors see exactly how much the prosthesis has improved mobility. This direct comparison is one of the clearest measures of prosthetic success.
The Six-Minute Walk Test (6MWT)
What the 6MWT Really Measures

The Six-Minute Walk Test, often called the 6MWT, is one of the simplest yet most insightful tools for measuring endurance and functional mobility.
It doesn’t require advanced machines or complex procedures — just a hallway, a timer, and a patient willing to walk. The idea is straightforward: how far can someone walk in six minutes at their own pace, safely and without interruption?
But beneath that simplicity lies powerful information about cardiovascular fitness, muscle strength, and real-world walking ability.
For doctors, this test translates the patient’s effort into measurable progress — showing exactly how well their body handles activity before and after prosthetic fitting.
Why It Matters for Prosthetic Users
Walking with a prosthesis is not just about taking steps; it’s about maintaining rhythm, endurance, and balance over time. The 6MWT helps physicians see how long a patient can sustain movement before fatigue sets in.
It’s an endurance test that reflects everyday life. Walking to the kitchen, the market, or a park bench all require stamina, not just balance. The 6MWT reveals whether the prosthesis supports sustained movement or needs adjustment for comfort and energy efficiency.
How the Test Is Conducted
The process is simple but standardized for accuracy. A flat, straight path — usually 30 meters long — is marked. The patient walks back and forth for six minutes while being monitored for heart rate, oxygen levels, and any discomfort.
They are encouraged to rest if needed but are asked to resume walking when ready. At the end, the total distance covered is recorded.
This single number — the distance walked in six minutes — tells a lot about the patient’s endurance and how well their body is adapting to the prosthetic.
What the Results Indicate
Doctors compare 6MWT results before and after prosthetic fitting. A significant increase in distance post-fit shows improvement in endurance, energy efficiency, and confidence.
For example, a patient who walks 100 meters before fitting and 250 meters afterward has doubled their functional walking ability. That’s a clear, measurable sign that the prosthesis and rehabilitation plan are working.
If progress is slow or stagnant, it’s a sign to reassess — perhaps adjusting the socket fit, changing prosthetic components, or modifying therapy intensity.
The Emotional Impact of the 6MWT
While the numbers provide data, the emotional effect of completing the test is just as valuable.
Many amputees begin rehabilitation unsure of how far they can go. Completing six minutes of steady walking often brings a visible sense of pride and confidence.
It’s no longer just about walking — it’s about endurance, control, and trust in their new limb. The 6MWT gives patients proof of their growing strength, and that encouragement often fuels their determination for the next goal.
Connecting the Test to Real Life
Doctors often use 6MWT results to discuss everyday mobility. If a patient can walk 200 meters in six minutes, it means they can likely manage household distances comfortably. A 400-meter result might indicate readiness for outdoor or community ambulation.
This connection between clinical data and real-world capability helps patients understand what their results mean in daily life. It makes the process relatable and motivating.
The Timed Up and Go (TUG) Test
What the TUG Test Evaluates
The Timed Up and Go (TUG) test is another practical measure of mobility, balance, and coordination. It focuses less on endurance and more on the fluidity and control of motion.
During the test, a patient starts seated in a chair, stands up on command, walks three meters, turns around, walks back, and sits down again. The total time taken to complete this sequence is recorded.
It’s a short, precise way to assess agility, balance, and how safely a person transitions from sitting to walking — all vital skills for prosthetic users.
Why Doctors Use TUG
Doctors use the TUG test to identify risk of falls and to assess how smoothly a patient can manage real-world movements.
Many older amputees or first-time prosthetic users struggle with standing up, turning, or sitting down without losing balance. The TUG test reveals these weaknesses quickly.
A slow or unsteady performance often indicates the need for targeted balance training, core strengthening, or adjustments in prosthetic alignment.
Because it involves common daily movements, the test is an excellent predictor of how safely and independently a patient can function outside the clinic.
How the Test Is Performed
The procedure is simple but must be done consistently for accuracy.
A standard chair with armrests is used, and the walking distance is exactly three meters. The patient is instructed to perform the sequence as naturally and safely as possible, without rushing.
The total time taken — from the command “go” to the moment they sit again — is measured with a stopwatch.
Lower times indicate better mobility and balance. Typically, under ten seconds suggests good functional ability, while longer times indicate areas for improvement.
Tracking Progress Over Time
Doctors use TUG results both before and after prosthetic fitting. A faster completion time after fitting shows improved strength, coordination, and confidence in the prosthesis.
By comparing these results, clinicians can clearly see whether rehabilitation efforts are effective or need modification.
Even a few seconds’ improvement can represent meaningful functional gains — fewer stumbles, faster transitions, and greater independence.
Early Detection of Risk Factors
The TUG test isn’t only for tracking progress — it’s also a diagnostic tool. It helps identify balance deficits and fall risk early.
If a patient takes longer or appears unstable during turns, it signals that further balance and proprioception training is needed. Addressing these issues early prevents injuries and ensures safe adaptation to the prosthesis.
This proactive approach allows doctors to modify therapy before problems escalate.
The Confidence Connection
Confidence and performance go hand in hand. Patients who hesitate or move cautiously during TUG testing often lack trust in their prosthesis or in their own body.
Repetition and encouragement help. As patients see their times improve, their confidence grows naturally. What begins as careful movement transforms into effortless control.
This is where the physician’s role as motivator becomes as important as the data itself.
Linking TUG, 6MWT, and AMPnoPRO Together
Each of these three tests — AMPnoPRO, 6MWT, and TUG — provides unique insight into different aspects of mobility.
AMPnoPRO measures potential before fitting.
6MWT measures endurance and stamina.
TUG measures agility and safety in movement.
When doctors use them together, they get a complete picture — from readiness to real-world performance.
These results also guide prosthetists and therapists in fine-tuning devices and training programs. For instance, if AMPnoPRO scores are high but 6MWT endurance is low, the issue may be cardiovascular fitness rather than prosthetic design.
Objective outcomes like these allow rehabilitation to become data-driven, personalized, and precise.
Comparing Pre-Fit and Post-Fit Results
Seeing the Difference Data Can Make
When doctors compare pre-fit and post-fit test results, they can literally see transformation in motion.
An increase in 6MWT distance, a reduction in TUG time, or a higher AMP score confirms that the prosthetic and therapy plan are working. This evidence-based approach builds trust not only between doctor and patient but also within the medical team.
It’s one of the reasons modern prosthetic care is moving strongly toward objective testing — because it makes progress visible.
The Motivation Behind Measurement
Numbers can inspire as much as they can inform. For many amputees, seeing their test results improve over time is like watching their determination come to life.
When doctors share results with genuine encouragement — “You’ve improved by 30 meters!” or “You completed that in half the time now!” — it transforms the rehabilitation journey into a shared celebration.
Motivated patients try harder, stay engaged, and recover faster.
Refining the Prosthesis and Rehabilitation Plan
Objective tests also help fine-tune the prosthetic design.
If a patient’s 6MWT distance doesn’t increase as expected, it may indicate that the prosthetic socket needs adjustment, or the alignment isn’t ideal. If the TUG test shows balance issues, therapists can modify the rehabilitation plan to include targeted exercises.
This feedback loop keeps care dynamic, ensuring that both the device and the therapy evolve with the patient’s progress.
Demonstrating Value to Stakeholders
For hospitals, rehabilitation centers, and prosthetic manufacturers, these measurable outcomes also provide evidence of quality.
When data shows consistent improvement in post-fit results, it reflects the effectiveness of clinical processes and technologies. This transparency builds confidence among patients, physicians, and insurers.
In India, where affordability and accountability are increasingly important in healthcare, such data-driven validation is transforming how prosthetic rehabilitation is delivered.
The Personal Transformation Behind the Numbers
Behind every improved score is a story of regained independence — a farmer walking back to his fields, a grandmother returning to her kitchen, a student climbing stairs again.
Doctors who use objective outcomes aren’t just collecting data; they’re helping write stories of recovery with precision and compassion.
These metrics prove that with the right timing, technology, and teamwork, progress is not a matter of luck — it’s measurable, repeatable, and real.
Long-Term Tracking and Follow-Up
Why Continued Measurement Matters

Recovery doesn’t stop once a prosthesis is fitted — it evolves. Muscles strengthen, confidence grows, and daily movement becomes smoother. But this progress needs consistent tracking.
Doctors who continue using objective outcome measures like AMPnoPRO, 6MWT, and TUG beyond the first few months can detect subtle changes that might otherwise go unnoticed.
Sometimes performance plateaus or declines because of socket wear, pain, or reduced motivation. Regular testing helps identify these shifts early, ensuring timely adjustments that keep patients moving confidently.
Turning Data Into a Roadmap
Each test result becomes a signpost in the patient’s recovery journey.
By comparing data across months or years, physicians can create a personalized mobility timeline. This not only helps fine-tune prosthetic alignment but also guides physical therapy goals.
It’s like tracking a heartbeat of progress — consistent, reliable, and deeply personal to each patient.
For example, if a patient’s 6MWT distance gradually drops, it might signal fatigue, muscle loss, or even depression. With data in hand, the physician can respond quickly and holistically, adjusting both physical and emotional support.
The Importance of Baseline Comparisons
The most valuable data in prosthetic rehabilitation comes from comparison — not between patients, but within the same person over time.
Every individual’s body, motivation, and healing rate are unique. That’s why pre-fit tests like AMPnoPRO set the foundation. Later 6MWT and TUG scores build upon it, showing tangible improvement unique to that person.
These comparisons give doctors a true measure of success: not perfection, but steady, meaningful growth.
Encouraging Lifelong Engagement
Objective outcomes also help maintain long-term motivation. Many patients, once they regain mobility, stop follow-up visits because they feel “done.” But rehabilitation is ongoing — especially as the body and prosthesis both change over time.
When doctors show patients their progress in numbers, it renews motivation. Seeing how far they’ve come — and what goals still lie ahead — keeps them invested in their own mobility journey.
Even a small improvement in walking distance or reduced time in TUG can reignite determination to keep training and maintaining their device.
Interpreting the Results in Practice
More Than Just Data Points
Numbers tell part of the story, but not all. Good doctors interpret results with context — understanding how each patient feels, moves, and lives.
A 6MWT result of 300 meters might be incredible progress for a senior amputee recovering from vascular disease, while the same distance might mean something different for a younger, athletic patient.
Interpreting results in context ensures fairness and accuracy. It also reinforces to patients that they’re not being compared to others — only to their own progress.
Combining Metrics for a Complete Picture
Each test — AMPnoPRO, 6MWT, and TUG — captures a different dimension of mobility.
When results are combined, they form a full portrait of capability: readiness, endurance, agility, and confidence.
For example, a high AMPnoPRO score with a low 6MWT result might indicate strong balance but poor stamina. A high 6MWT with a slower TUG time might mean endurance is good but turns and transitions are still challenging.
By seeing how these scores interact, doctors can personalize rehabilitation programs to close specific gaps.
Identifying Prosthetic-Related Barriers
Sometimes test results reveal issues that have nothing to do with fitness — they point to prosthetic challenges.
If a patient’s endurance suddenly declines, the socket may be causing discomfort or poor suspension. If balance scores fall, alignment might be off.
Objective data helps distinguish between physical and mechanical barriers. This clarity allows physicians and prosthetists to make quick, precise adjustments rather than relying on guesswork.
Tracking the Psychological Component
Mobility is as much mental as it is physical. Data trends often mirror emotional states.
A patient who’s discouraged might show reduced walking distance or slower movement, even when physically capable of more. A motivated, confident patient often performs better than expected.
Doctors who combine empathy with data can read these signs early. Encouraging counseling or peer support alongside training can help lift motivation and performance simultaneously.
Turning Data Into Dialogue
The most powerful part of these results is not the numbers themselves — it’s how doctors communicate them.
When data is shared with warmth and context, it transforms clinical assessment into a conversation of empowerment.
Saying “Your walking distance improved by 30%” isn’t just feedback — it’s validation of the patient’s effort, willpower, and discipline. It tells them they’re not just healing — they’re succeeding.
Building a Culture of Measurement in Prosthetic Care
Making Objective Testing Routine
For years, many clinics treated prosthetic rehabilitation as an art more than a science. While experience and intuition are invaluable, combining them with data creates stronger, more reliable outcomes.
Doctors should make tests like AMPnoPRO, 6MWT, and TUG a standard part of every prosthetic journey — not just optional extras.
When these become routine, they raise the quality of care across the board, ensuring every patient receives structured, evidence-based guidance.
Bridging the Gap Between Hospitals and Prosthetic Centers
In India, one major challenge is coordination between medical facilities and prosthetic providers. Hospitals handle surgeries, while prosthetic centers focus on fitting and training — often working separately.
Objective outcomes create a shared language between both.
When hospitals record pre-fit results and prosthetic centers track post-fit data, the transition becomes smoother and more transparent. Both sides can clearly see what’s working — and what needs more attention.
This collaboration ensures continuity of care from surgery to recovery, giving every patient a seamless experience.
Data as a Tool for Education and Training
For medical students and rehabilitation specialists, outcome measures are invaluable teaching tools. They help new professionals learn how to assess, document, and interpret progress systematically.
Using these tests during clinical rotations or workshops helps young doctors and therapists understand the subtle differences between observation and evidence.
It trains them to rely not only on their eyes but also on measurable facts — a skill that elevates patient care.
Improving Accessibility in India
While these tests are simple and inexpensive, they’re not yet universally used across smaller clinics in India. Increasing awareness among physicians, especially in semi-urban and rural areas, can help standardize care nationwide.
Because tests like 6MWT and TUG require minimal equipment — just space, time, and guidance — even small centers can adopt them easily.
This democratization of testing ensures that amputees in every corner of the country can benefit from structured, scientific rehabilitation.
How RoboBionics Integrates Objective Outcomes
The Role of Technology in Tracking Progress

At RoboBionics, our approach to prosthetic care is deeply rooted in both compassion and measurable results. We design devices that empower users, but we also believe in data that proves their impact.
When a patient is fitted with our Grippy™ Bionic Hand or similar prosthetic solutions, we encourage doctors and therapists to track performance through standardized tests like AMPnoPRO, 6MWT, and TUG.
This not only validates the prosthesis’ performance but also helps us continuously improve our designs based on real-world outcomes.
Designed for Function, Measured for Results
Our products are built to reflect human movement — intuitive, responsive, and reliable. But their success isn’t just about engineering; it’s about how they improve people’s daily lives.
When users walk further, grip more steadily, or move more confidently after fitting, those results are proof of what thoughtful design can achieve.
Doctors who track these outcomes can clearly see how early fitting and personalized prosthetic selection lead to faster rehabilitation and stronger long-term results.
Closing the Loop Between Doctor and Maker
RoboBionics works closely with physicians and rehabilitation centers across India to create a feedback loop — from the clinic floor back to our design team.
Every test result, every data point, every patient milestone contributes to making prosthetic technology smarter and more accessible.
Our mission isn’t just to build prosthetics, but to build partnerships — with doctors who believe in measurable progress and patients who trust that their recovery is guided by science and care combined.
Accessible, Affordable, and Proven
Imported prosthetics often remain out of reach for most Indian families, costing over ₹10 lakh. RoboBionics bridges that gap by creating locally manufactured, world-class devices priced between ₹2.15–3 lakh.
By keeping 60 of our 64 components made in India, we ensure affordability without compromise.
This accessibility means that outcome-driven rehabilitation is no longer reserved for the privileged few — it’s available to anyone who dares to take the next step forward.
The Human Story Behind Every Test
Beyond the Numbers
Each AMPnoPRO score, each six-minute distance, each TUG time — they all tell stories far deeper than data can express.
They’re the stories of patients who refused to stop moving, families who refused to give up hope, and doctors who believed that progress can always be measured — not in perfection, but in persistence.
Every second shaved off a TUG time is a second gained in independence. Every extra meter walked in six minutes is a meter closer to normalcy. Every improved AMP score is a reminder that mobility is not just a function of limbs, but of willpower.
The Doctor’s Satisfaction
Few things in medicine are as rewarding as watching measurable recovery unfold.
When doctors track objective outcomes, they see their expertise reflected in real, visible progress. They witness science translating directly into human impact — step by step, test by test.
It’s a reminder that behind every prosthetic device and every data sheet stands the shared goal of restoring life’s rhythm — the joy of walking, the pride of self-sufficiency, the peace of confidence regained.
The Future of Objective Care
The future of prosthetic rehabilitation in India lies in data — but guided by empathy.
As more physicians adopt objective measures, rehabilitation will become faster, safer, and more effective. Patients will not only recover but thrive.
With innovation from companies like RoboBionics, data and design will continue to merge, creating a system where every test result not only informs treatment but also inspires the next generation of mobility technology.
Conclusion: Progress You Can Measure, Freedom You Can Feel
Prosthetic rehabilitation is both a science and a story. The science lies in the data — AMPnoPRO scores, six-minute distances, and timed transitions. The story lies in what those numbers mean — the courage, persistence, and freedom behind every step.
For doctors, objective outcomes aren’t just clinical metrics; they’re tools of transformation. They show where a patient begins, how far they’ve come, and how much further they can go.
At RoboBionics, we believe in measurable progress — because data proves what the heart already knows: mobility is not just movement; it’s life in motion.
If you’re a physician, therapist, or rehabilitation specialist who believes in empowering patients through evidence-based care, we invite you to partner with us.
Book a demo or connect at www.robobionics.in/bookdemo — and together, let’s redefine recovery, one measured step at a time.