
Post-Op Follow-Up Schedule That Prevents Prosthetic Delays (For Clinicians)
For many clinicians, the surgery is only the first step. What happens after the operation

When a person loses an arm or hand, the loss goes far beyond the physical. It affects how they dress, eat, write, work, and even how they see themselves. Every gesture we take for granted — holding a cup, typing a message, shaking hands — suddenly feels out of reach.
But thanks to new-generation prosthetics, especially myoelectric hands, that reach is returning faster than ever. Myoelectric prostheses use the body’s natural muscle signals to control artificial limbs, letting people move and grip more intuitively.
For doctors, though, the big question isn’t just what prosthesis to recommend — it’s when. Should training with myoelectric systems begin early, right after healing, or should patients first adapt with mechanical devices?
Timing makes all the difference. Early myoelectric training can reshape recovery — rewiring the brain, building muscle coordination, and restoring function more naturally. But it also requires careful judgment, emotional readiness, and structured medical guidance.
This article explores how surgeons, physiatrists, and rehabilitation specialists can identify the right moment to begin myoelectric training, the signs of readiness in upper-limb amputees, and how early exposure can transform both physical and emotional recovery.
Because when motion returns early, so does confidence, purpose, and life itself.
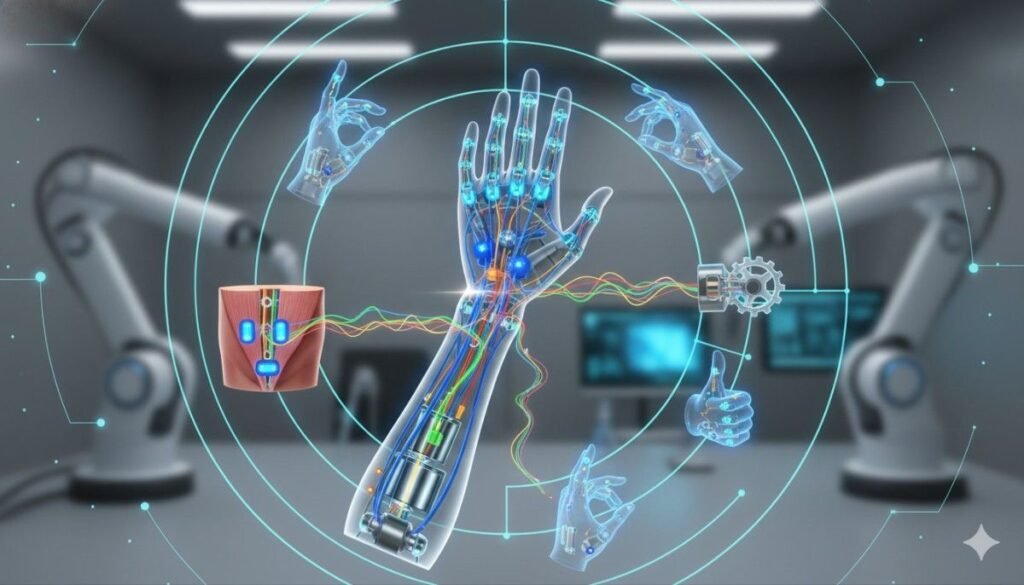
A myoelectric prosthesis works by reading the body’s own electrical signals — the tiny impulses muscles naturally create when they contract.
When a patient with an upper-limb amputation flexes or tenses their remaining muscles, those signals are detected by sensors inside the prosthetic socket. The prosthesis then translates those signals into movement — opening a hand, bending a wrist, or rotating fingers.
It’s not just movement through machinery. It’s motion through intent — the user thinks of moving, and the prosthesis responds almost instantly.
Traditional mechanical prostheses rely on cables and body motion to generate movement. For instance, pulling the shoulder might open a hook or move a joint. These systems are durable and simple, but they depend heavily on body strength and coordination.
Myoelectric systems, on the other hand, replace physical effort with electrical precision. They respond to thought-driven muscle activity, allowing smoother and more natural control.
For patients, this feels closer to having their own hand again — not just a tool attached to their arm.
The key to success with myoelectric systems lies in the sensors. These electrodes must be placed correctly over residual muscles capable of producing strong, consistent signals.
But muscles don’t automatically know how to send those signals accurately. That’s where early myoelectric training becomes critical.
Through guided exercises, patients learn how to contract specific muscles intentionally, strengthening the connection between thought, signal, and movement.
The earlier this training begins, the easier it is for the brain to adapt and create new neural pathways for control.
The human brain is incredibly adaptable — but only for a certain time after amputation. In the early months, it’s still “relearning” body maps and adjusting to sensory changes.
Starting myoelectric training during this phase can help the brain accept the prosthesis as part of the body. Delaying too long risks the brain “forgetting” how to control those muscles naturally, making learning harder later on.
For this reason, physicians now see early training not as an option but as a vital part of neuro-muscular recovery.
After an amputation, unused muscles begin to weaken — a process called atrophy. The longer these muscles stay idle, the weaker their electrical signals become.
Early myoelectric training keeps these muscles active. Even before the prosthesis is fitted, doctors can start simple exercises that maintain strength and signal clarity.
This early conditioning ensures that when the prosthesis is finally worn, the muscles are ready to communicate effectively with the sensors.
Movement is more mental than physical. Every time we move our hand, our brain sends electrical instructions to muscles. After amputation, that pathway gets disrupted.
If the brain stops sending those signals, it starts to “forget” the limb existed — a process known as cortical reorganization.
Starting myoelectric training early helps keep those neural pathways alive. The patient learns to send signals again, even without a natural limb. This helps integrate the prosthesis into their body’s sense of self — turning technology into extension.
Many amputees experience phantom limb pain — the feeling that the missing hand still exists and hurts.
Early myoelectric exercises can reduce this pain. When patients start moving muscles purposefully and see the prosthetic hand respond, it rewires how the brain perceives the missing limb.
It creates a visual and sensory feedback loop that soothes the confusion between brain and body.
For many patients, this becomes a form of therapy that eases both pain and emotional distress.
For someone who has lost a hand, the first time they see a myoelectric prosthesis move in response to their own thought is powerful. It’s not just a technical achievement — it’s hope made visible.
Early success motivates patients to participate actively in rehabilitation. They feel less like they’re being “trained” and more like they’re regaining control.
Physicians who encourage early myoelectric practice often notice stronger engagement and lower dropout rates in rehabilitation programs.
When patients spend too much time relying on their intact hand or shoulder, they develop habits that make using a prosthesis harder later.
Early training prevents these compensations. It teaches the body to distribute movement naturally, using both sides again — even if one side is artificial.
This balanced coordination reduces strain on the sound limb and promotes long-term musculoskeletal health.

Prescribing a myoelectric prosthesis isn’t a single decision — it’s a shared responsibility among surgeons, physiatrists, occupational therapists, and prosthetists.
Each specialist brings unique insights. The surgeon ensures healing and stump health. The physiatrist evaluates muscle strength and signal quality. The occupational therapist tests coordination and daily use potential.
When these professionals collaborate, they can decide not only who should begin early training but also how soon to start it safely.
Timing starts with healing. Before training begins, the surgical site must be fully closed, pain must be manageable, and swelling should have subsided.
Physicians monitor the residual limb for proper shape, scar flexibility, and muscle activation. Once these are stable, the patient can begin surface EMG (electromyography) training — even before receiving the prosthesis itself.
Early EMG conditioning ensures that the prosthesis feels intuitive from day one.
Each patient’s anatomy is different. Physicians and prosthetists work together to identify the most responsive muscle groups near the amputation site — often the biceps, triceps, or forearm flexors.
During pre-fitting sessions, electrodes are used to test signal strength and stability. The best sites are then chosen for sensor placement on the future prosthetic socket.
This careful preparation turns the first day of prosthesis use into a continuation of therapy, not a brand-new learning curve.
Myoelectric systems rely on consistent mental focus, especially during early stages of training.
Physicians assess whether the patient is emotionally ready to engage — whether they understand that progress takes time and practice. For many, early success builds motivation; for others, frustration can arise if expectations are not managed.
That’s why patient education is vital. Explaining how the system works, what to expect, and what small victories look like helps set a positive tone for the entire journey.
The best rehabilitation outcomes happen when patients can see their effort turning into action.
Doctors and therapists use visual EMG feedback systems that display muscle signal strength on a screen. Patients watch as their muscle contractions generate digital movement, reinforcing learning and motivation.
This feedback bridges the invisible gap between thought and control, preparing them for when they’ll do the same with their prosthesis.
Even before a prosthetic is fitted, doctors can start early conditioning. The goal is to help the patient learn which muscles to activate and how to produce consistent signals.
Therapists teach small, isolated contractions — tightening specific muscles while keeping others relaxed. Sessions are short but frequent, focusing on control and accuracy rather than strength.
By the time the prosthesis arrives, the brain-muscle connection is already established.
Once the prosthetic is fitted, patients begin basic control exercises. These might include opening and closing the hand, flexing the wrist, or switching grip modes.
At first, these actions require concentration, but over time, they become automatic. The key is repetition — turning intentional control into instinctive movement.
Physicians monitor progress and adjust the electrode sensitivity to ensure comfort and responsiveness.
As control improves, training moves into real-life activities. Patients learn to use their prosthesis for tasks like picking up small objects, holding utensils, or performing personal grooming.
These exercises are both physical and psychological. They help the user see the prosthesis as a natural extension of the body rather than an external device.
Therapists encourage gradual complexity — from single tasks to multi-step actions that mimic daily routines.
Every step forward deserves recognition. Physicians and therapists celebrate milestones — the first grasp, the first smooth motion, the first successful meal prepared independently.
Acknowledgment strengthens emotional resilience and helps patients push through the tougher phases of rehabilitation.
This emotional aspect is as important as the physical one because motivation drives mastery.
The first consideration for early myoelectric prescription is always the health of the residual limb.
The skin should be fully healed, free of infection, and flexible enough to handle gentle movement. Scar tissue should be soft and mobile, not tight or painful. Any persistent swelling or tenderness can delay training until the limb stabilizes.
Physicians also look at the limb’s shape. A well-contoured, cylindrical shape allows better socket fit and electrode contact — essential for consistent signal pickup.
If healing is complete and the patient can tolerate light compression without discomfort, early training can begin safely.
The second criterion is signal clarity. Myoelectric prostheses rely entirely on electrical impulses generated by muscle contractions.
Physicians use electromyography (EMG) testing to measure whether these signals are strong, stable, and repeatable.
If the signals are inconsistent, therapists introduce pre-training exercises to help the patient isolate and strengthen specific muscle groups. Once two or more reliable control sites are established, the patient is ready for active training.
Even small, consistent signals are enough to start — the key is predictability, not power.
Before fitting an upper-limb prosthesis, physicians evaluate shoulder and elbow mobility. Restricted movement in these joints can affect the control and comfort of the prosthetic.
Gentle stretching and range-of-motion exercises are prescribed early to ensure smooth, pain-free motion.
This preparation prevents muscle imbalance and improves the accuracy of muscle signals once the prosthesis is in place.
Emotional readiness is just as crucial as physical healing. Patients dealing with shock, grief, or depression may struggle to engage with technology early on.
Physicians assess mood, motivation, and overall mental well-being before prescribing early myoelectric use.
When emotional stability is restored — through counseling, peer support, or early rehabilitation success — the patient’s ability to learn and adapt increases dramatically.
Doctors often say that a motivated patient can overcome even technical challenges with time and consistency.
Myoelectric prostheses demand focus, patience, and the ability to follow structured instructions.
Physicians evaluate whether the patient can understand and remember operational guidelines — such as turning the prosthesis on or off, charging it, or recognizing signal feedback.
Cognitive readiness ensures safety and independence, especially in the early stages when daily adjustment and care are essential.
Early myoelectric success depends heavily on structured follow-up.
Physicians must confirm that patients have access to occupational therapy, prosthetic adjustment, and consistent training environments.
Those who live near active rehabilitation centers or can attend regular sessions are ideal candidates for early prescription. For those in remote areas, tele-rehabilitation or home-based exercise plans can fill the gap.
A strong support network keeps progress continuous and prevents frustration.
Traumatic amputees — those who lose a limb due to accidents or injuries — often have strong emotional drive to recover quickly.
They usually possess good muscle tone and neural response in the residual limb, which makes them excellent candidates for early myoelectric training.
Doctors recommend beginning EMG conditioning as soon as healing allows. Within weeks, these patients can start basic myoelectric control exercises.
Early exposure helps rebuild confidence, especially for those eager to return to work or active lifestyles.
For congenital limb absence — where the limb never developed fully — timing is more complex.
Children born with partial limbs may not have pre-existing muscle memory for certain movements. Yet, early introduction to myoelectric systems can stimulate their brain to learn control from a young age.
Physicians often start training around the ages of two to four, depending on attention span and cooperation. The goal isn’t perfection but exposure — helping the child understand cause and effect between thought and movement.
Over time, these early lessons form the foundation for advanced prosthetic control later in life.
For patients who lose limbs due to poor circulation or diabetes, early myoelectric introduction can be more cautious.
Their residual limbs may take longer to heal, and sensory feedback might be reduced. However, once stable, these patients can still benefit from early signal training.
Doctors focus on gentle muscle activation, avoiding strain, and gradually building endurance. The advantage of early myoelectric work here is improved circulation and muscle engagement, which promote healing and prevent further degeneration.
Patients with amputations on both sides face unique challenges, particularly in learning control and performing daily activities.
For them, early myoelectric training is essential — not only to regain independence but also to prevent overreliance on caregivers.
Doctors and therapists prioritize one side at a time, teaching signal control gradually before introducing dual-arm coordination.
In these cases, early training doesn’t just restore motion — it restores autonomy and dignity.
Children adapt faster than adults when introduced to new systems, including prosthetics. Their brains are still developing motor pathways, making early myoelectric exposure ideal for lifelong integration.
Physicians typically begin with lightweight systems and short training sessions. As children grow, prostheses are upgraded to match strength and coordination levels.
Early exposure helps children accept their prosthesis naturally, reducing stigma and building confidence from school age.
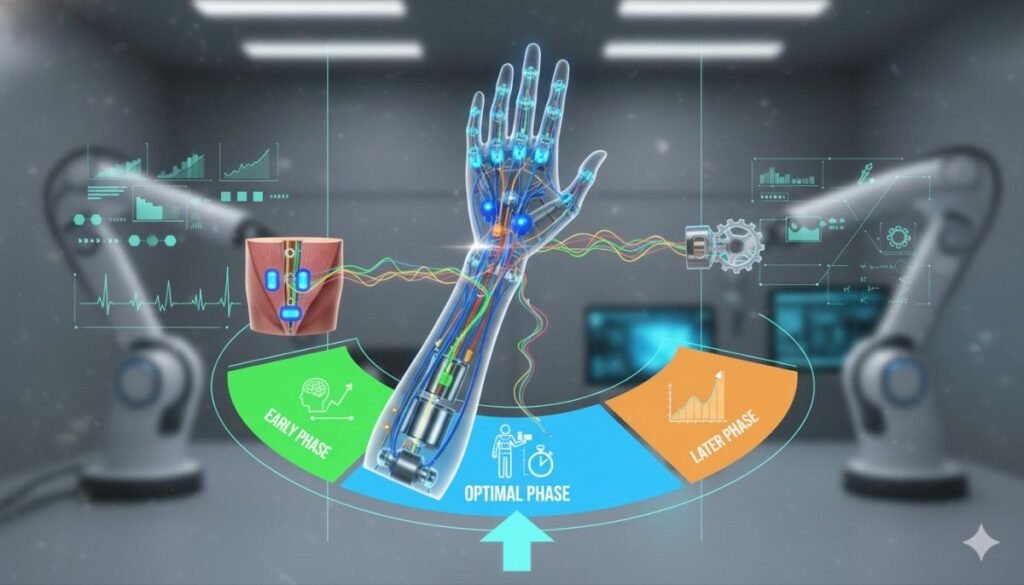
Most physicians consider the first six months after amputation as the “golden window” for introducing myoelectric concepts.
During this time, the brain’s neural plasticity is high — meaning it can form new connections rapidly. The body is healing, but muscles are still responsive and capable of generating strong signals.
Starting training within this period helps bridge the gap between loss and adaptation. Patients feel progress instead of stagnation, which accelerates emotional recovery.
Even if the prosthesis isn’t fitted yet, EMG practice during this phase lays a strong foundation for later control.
Between six months and a year, adaptation remains possible but requires more structured reinforcement.
If patients have delayed rehabilitation, they might develop compensatory habits or mild muscle disuse. Myoelectric training during this phase should therefore focus on reactivation — rebuilding lost muscle coordination and control.
Physicians adjust training intensity gradually to prevent fatigue while restoring responsiveness.
After a year or more, delayed myoelectric training is still effective but may take longer. The brain has settled into compensatory habits, and muscles might require longer retraining.
Still, many late-start users achieve excellent results when guided with patience and persistence.
Doctors may combine myoelectric training with sensory feedback therapy and mirror exercises to reawaken dormant pathways.
This shows that while early is best, it’s never too late to begin.
Patients who begin early develop smoother, more coordinated movements. Their brain learns to associate thought with prosthetic response naturally, without overthinking each motion.
This makes their gait, gestures, and daily actions more fluid and lifelike. Over time, these users exhibit better endurance and faster reaction times compared to those who started late.
Early adopters tend to achieve higher functional independence scores in clinical evaluations. They can perform daily tasks — from eating and dressing to typing and carrying objects — more efficiently.
This independence directly impacts self-esteem and quality of life, reducing dependence on family or caregivers.
Delayed rehabilitation often leads to overcompensation by the sound limb.
Patients who start early myoelectric control distribute effort more evenly between both sides, reducing strain on the intact shoulder and spine.
This balance prevents long-term musculoskeletal pain and promotes sustainable mobility.
Early results breed motivation. When patients see progress within weeks — moving, gripping, holding — they stay engaged with therapy.
This consistent effort ensures steady improvement and reduces dropout rates, which are a common challenge in long-term prosthetic training.
Perhaps the most profound impact of early training is psychological integration.
The sooner patients start using a myoelectric prosthesis, the sooner they stop viewing it as “equipment” and start experiencing it as part of themselves.
That sense of ownership — of this is my hand — defines successful rehabilitation. It bridges the gap between medical recovery and personal rebirth.
Every successful myoelectric journey starts with a plan. For physicians, the process begins long before the prosthesis arrives. The first step is to create a timeline that bridges surgery, healing, and training seamlessly.
Surgeons, physiatrists, prosthetists, and therapists work together to align goals. Once healing is stable, the team introduces the concept of myoelectric control gently, showing the patient what’s possible and setting clear, achievable expectations.
This early planning keeps the process structured, reducing fear and confusion while keeping patients focused on progress.
Even without a prosthesis, early EMG (electromyography) training can begin. Doctors and therapists attach small surface sensors to the residual limb and display real-time muscle signals on a screen.
The patient learns which muscles control which actions. They practice tensing specific areas and observing feedback visually. It becomes a form of biofeedback therapy — teaching the body how to communicate effectively again.
These sessions are short, often just ten to fifteen minutes, but their impact is lasting. When the prosthesis finally arrives, the user already knows how to “speak” to it through their muscles.
Once the socket and electrodes are fitted, training shifts from simulation to reality. Early sessions focus on simple actions — opening and closing the hand, flexing the wrist, or holding light objects.
Physicians ensure that electrode placement is comfortable and that the system responds correctly to the user’s natural signals. Adjustments are made frequently in this stage to fine-tune sensitivity.
Progress is celebrated step by step. Every successful grasp or motion is a reminder that control is returning, not as a miracle, but as a result of persistence and partnership between patient and physician.
After mastering basic control, the patient begins using the prosthesis for everyday tasks. Therapists incorporate real-world activities — eating, buttoning clothes, typing, and carrying objects — into rehabilitation.
Doctors monitor for fatigue, frustration, or discomfort and adapt sessions accordingly. These exercises teach the patient not only control but endurance and confidence in unpredictable environments.
By gradually blending training with daily life, myoelectric use becomes less of an exercise and more of a lifestyle.
Early stages of training are a time of learning, not perfection. Doctors encourage constant feedback — from both the patient and the rehabilitation team.
If signals are inconsistent or control feels awkward, adjustments are made immediately. Sometimes the socket needs refitting; other times, the user needs more focused muscle isolation practice.
Frequent fine-tuning ensures that the prosthesis feels intuitive, not foreign. This personalized approach keeps adaptation smooth and frustration low.
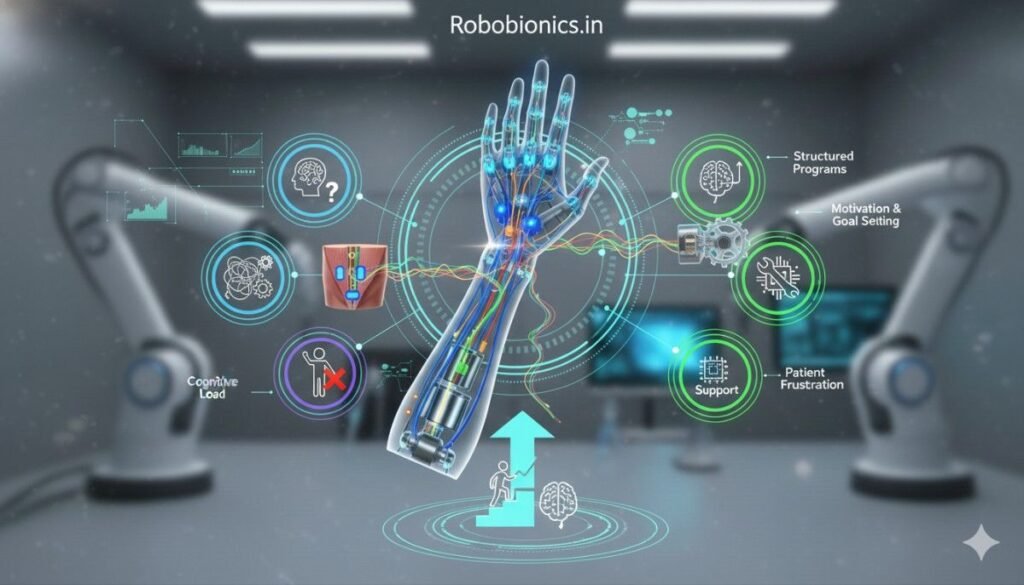
In the first weeks, patients may feel tired or discouraged when movements don’t come easily. The brain and muscles are working together in unfamiliar ways, which can be mentally draining.
Physicians reassure patients that this struggle is normal and temporary. Regular rest breaks, positive reinforcement, and short, frequent sessions help maintain energy and motivation.
By turning frustration into small victories, doctors keep recovery emotionally steady and sustainable.
Some patients experience phantom movements or sensations while training. Interestingly, these sensations can be used therapeutically.
When patients “move” their phantom hand and see the prosthetic respond, it helps the brain link the two, reducing discomfort and confusion.
Doctors use this phenomenon to reinforce the natural connection between thought and movement — a subtle but powerful form of mental rehabilitation.
Trust is one of the biggest barriers early on. Patients may hesitate, fearing the prosthesis will slip, fail, or misread their signal.
Physicians build trust by demonstrating reliability through repeated success. The more the prosthesis responds correctly, the more confidence grows.
Once trust is established, users stop overthinking. They move spontaneously, the way they once did before amputation. That moment — when hesitation becomes instinct — is a major milestone.
Early training succeeds when communication between the care team is strong. Physicians, prosthetists, and therapists must share progress updates constantly.
If the prosthesis feels too sensitive, or if training exercises need modification, information flows freely so that adjustments happen quickly.
This collaboration prevents setbacks and keeps recovery dynamic, responsive, and personalized to each individual’s needs.
A 28-year-old mechanical engineer lost his right hand in an industrial accident. Within three months of surgery, his wound was healed, and EMG training began.
Because his mind was sharp and his motivation strong, he progressed quickly. By the time his myoelectric hand was fitted, he could already control the opening and closing motions smoothly.
Within weeks, he was writing emails, eating independently, and even sketching designs again. His success came from early exposure — the ability to learn before fear or muscle decline set in.
A 45-year-old woman with a below-elbow amputation struggled initially with depression and fear of technology. The medical team introduced her gradually to EMG exercises, focusing on confidence before complexity.
When she finally started using her prosthesis, she adapted quickly, saying it felt like “her hand listening to her again.”
She soon resumed cooking, folding clothes, and caring for her family — all tasks that once felt impossible. Early myoelectric introduction not only restored function but reignited identity.
At 63, the teacher lost her hand due to diabetic complications. Doctors waited for full healing but started muscle stimulation exercises early to preserve strength.
By the fourth month, she began myoelectric control training using gentle practice sessions. The early start kept her muscle signals clear and consistent.
Today, she teaches her grandchildren handwriting exercises using her prosthetic hand — a testament to both technology and timing.
For many years, access to advanced myoelectric prosthetics in India was limited to imported models priced beyond reach for most families. This financial gap delayed many patients from receiving technology that could transform their lives.
RoboBionics has changed that landscape. By designing and manufacturing 60 of 64 components domestically, we’ve made bionic technology both world-class and affordable.
Our flagship product, the Grippy™ Bionic Hand, brings advanced myoelectric control to Indian users at a price point between ₹2.15–3 lakh — a fraction of international alternatives.
This accessibility allows doctors to recommend early myoelectric training without hesitation about affordability. It ensures that cost never delays care.
Indian lifestyles are diverse and demanding. People work in varying environments — from offices to farms — and need prosthetics that can handle it all.
RoboBionics designed Grippy™ to be lightweight, durable, and adaptable. Its ergonomic structure makes it comfortable for long hours of wear, even in humid or warm climates.
For physicians, this reliability means early fitting can proceed confidently, knowing the device will perform consistently in real conditions.
One of the most unique aspects of RoboBionics’ technology is our Sense of Touch™ feature — a tactile feedback system that lets users “feel” pressure when holding objects.
This sensory connection transforms training outcomes. When patients start early with feedback-enabled systems, their brain learns faster, developing coordination that feels natural instead of mechanical.
This sensory realism speeds up emotional acceptance and functional mastery, shortening the rehabilitation timeline significantly.
RoboBionics works hand in hand with physicians, prosthetic clinics, and rehabilitation centers across India. Together, we run awareness programs, early training workshops, and patient counseling sessions.
For surgeons and physiatrists, this partnership ensures smooth coordination between surgery, healing, and prosthetic training.
For patients, it creates a continuum of care — one that begins at the hospital and continues seamlessly into home life.
We also collaborate with hospitals to gather clinical outcome data. By tracking recovery through metrics like the AMPnoPRO, 6MWT, and TUG tests, we help doctors measure the true impact of early prosthetic fitting.
This evidence-based approach supports better decision-making and highlights how early myoelectric introduction improves outcomes across diverse patient groups.
For the medical community, data transforms belief into proof — and proof inspires confidence to act sooner.
For most patients, losing a hand feels like losing part of their identity. Early myoelectric training helps rebuild that identity by returning control faster.
When movement returns, so does dignity. Patients start to look at their prosthesis not as a replacement but as an extension of self. That psychological transformation is just as important as the physical one.
One of the subtle but significant benefits of early training is the confidence it gives patients in social situations. Instead of hiding their limb or avoiding interaction, they engage freely, often showing pride in what they’ve achieved.
Doctors often observe that early mobility correlates strongly with higher self-esteem and lower rates of social withdrawal.
Family plays a vital role in this process. When loved ones see progress early — when they watch a parent or child move their prosthetic hand — their encouragement becomes even stronger.
Physicians are now emphasizing family education during training, ensuring they understand how to support, not overprotect, the user. This shared journey strengthens relationships and speeds recovery.
As technology becomes more accessible, early myoelectric introduction should move from exception to standard. Hospitals and rehabilitation centers can include EMG conditioning as part of post-surgical care rather than waiting months.
This integration will not only shorten recovery timelines but also raise national standards for upper-limb rehabilitation.
RoboBionics is actively working to bring myoelectric technology to smaller towns through mobile prosthetic units and tele-rehabilitation platforms.
These programs ensure that distance never becomes a barrier to recovery. Patients can begin early muscle training even before their first in-person fitting, guided remotely by specialists.
We continue to refine our devices based on real-world patient feedback. Every improvement — whether in grip precision, battery life, or tactile response — is designed to make early adaptation smoother.
Our mission remains simple: to empower physicians and patients with tools that restore not just motion, but meaning.
When it comes to myoelectric training, timing isn’t just technical — it’s life-changing.
Starting early keeps muscles active, preserves brain pathways, and prevents emotional stagnation. It bridges the gap between loss and control, between surgery and independence.
For physicians, prescribing early myoelectric training isn’t just about giving access to advanced technology. It’s about giving patients the best chance to rediscover movement, identity, and hope.
And for patients, every small signal — every flicker of control — marks the beginning of something extraordinary.
At RoboBionics, we believe that rehabilitation should begin with readiness, not delay. That’s why our prosthetic systems, like the Grippy™ Bionic Hand, are built to make early recovery possible, affordable, and deeply personal.
If you’re a surgeon, physiatrist, or therapist ready to help your patients move sooner and heal stronger, connect with us today.
Book a demo or schedule a consultation at robobionics.in/bookdemo.
Let’s make early mobility the new standard in India — because every patient deserves to feel whole again, one signal, one movement, one step at a time.

For many clinicians, the surgery is only the first step. What happens after the operation

For trauma amputees, the journey does not begin at the prosthetic clinic. It begins much

Amputation after cancer is not just a surgical event. It is the end of one

When a child loses a limb, the challenge is never only physical. A child’s body
Last updated: November 10, 2022
Thank you for shopping at Robo Bionics.
If, for any reason, You are not completely satisfied with a purchase We invite You to review our policy on refunds and returns.
The following terms are applicable for any products that You purchased with Us.
The words of which the initial letter is capitalized have meanings defined under the following conditions. The following definitions shall have the same meaning regardless of whether they appear in singular or in plural.
For the purposes of this Return and Refund Policy:
Company (referred to as either “the Company”, “Robo Bionics”, “We”, “Us” or “Our” in this Agreement) refers to Bionic Hope Private Limited, Pearl Haven, 1st Floor Kumbharwada, Manickpur Near St. Michael’s Church Vasai Road West, Palghar Maharashtra 401202.
Goods refer to the items offered for sale on the Website.
Orders mean a request by You to purchase Goods from Us.
Service refers to the Services Provided like Online Demo and Live Demo.
Website refers to Robo Bionics, accessible from https://robobionics.in
You means the individual accessing or using the Service, or the company, or other legal entity on behalf of which such individual is accessing or using the Service, as applicable.
You are entitled to cancel Your Service Bookings within 7 days without giving any reason for doing so, before completion of Delivery.
The deadline for cancelling a Service Booking is 7 days from the date on which You received the Confirmation of Service.
In order to exercise Your right of cancellation, You must inform Us of your decision by means of a clear statement. You can inform us of your decision by:
We will reimburse You no later than 7 days from the day on which We receive your request for cancellation, if above criteria is met. We will use the same means of payment as You used for the Service Booking, and You will not incur any fees for such reimbursement.
Please note in case you miss a Service Booking or Re-schedule the same we shall only entertain the request once.
In order for the Goods to be eligible for a return, please make sure that:
The following Goods cannot be returned:
We reserve the right to refuse returns of any merchandise that does not meet the above return conditions in our sole discretion.
Only regular priced Goods may be refunded by 50%. Unfortunately, Goods on sale cannot be refunded. This exclusion may not apply to You if it is not permitted by applicable law.
You are responsible for the cost and risk of returning the Goods to Us. You should send the Goods at the following:
We cannot be held responsible for Goods damaged or lost in return shipment. Therefore, We recommend an insured and trackable courier service. We are unable to issue a refund without actual receipt of the Goods or proof of received return delivery.
If you have any questions about our Returns and Refunds Policy, please contact us:
Last Updated on: 1st Jan 2021
These Terms and Conditions (“Terms”) govern Your access to and use of the website, platforms, applications, products and services (ively, the “Services”) offered by Robo Bionics® (a registered trademark of Bionic Hope Private Limited, also used as a trade name), a company incorporated under the Companies Act, 2013, having its Corporate office at Pearl Heaven Bungalow, 1st Floor, Manickpur, Kumbharwada, Vasai Road (West), Palghar – 401202, Maharashtra, India (“Company”, “We”, “Us” or “Our”). By accessing or using the Services, You (each a “User”) agree to be bound by these Terms and all applicable laws and regulations. If You do not agree with any part of these Terms, You must immediately discontinue use of the Services.
1.1 “Individual Consumer” means a natural person aged eighteen (18) years or above who registers to use Our products or Services following evaluation and prescription by a Rehabilitation Council of India (“RCI”)–registered Prosthetist.
1.2 “Entity Consumer” means a corporate organisation, nonprofit entity, CSR sponsor or other registered organisation that sponsors one or more Individual Consumers to use Our products or Services.
1.3 “Clinic” means an RCI-registered Prosthetics and Orthotics centre or Prosthetist that purchases products and Services from Us for fitment to Individual Consumers.
1.4 “Platform” means RehabConnect™, Our online marketplace by which Individual or Entity Consumers connect with Clinics in their chosen locations.
1.5 “Products” means Grippy® Bionic Hand, Grippy® Mech, BrawnBand™, WeightBand™, consumables, accessories and related hardware.
1.6 “Apps” means Our clinician-facing and end-user software applications supporting Product use and data collection.
1.7 “Impact Dashboard™” means the analytics interface provided to CSR, NGO, corporate and hospital sponsors.
1.8 “Services” includes all Products, Apps, the Platform and the Impact Dashboard.
2.1 Individual Consumers must be at least eighteen (18) years old and undergo evaluation and prescription by an RCI-registered Prosthetist prior to purchase or use of any Products or Services.
2.2 Entity Consumers must be duly registered under the laws of India and may sponsor one or more Individual Consumers.
2.3 Clinics must maintain valid RCI registration and comply with all applicable clinical and professional standards.
3.1 Robo Bionics acts solely as an intermediary connecting Users with Clinics via the Platform. We do not endorse or guarantee the quality, legality or outcomes of services rendered by any Clinic. Each Clinic is solely responsible for its professional services and compliance with applicable laws and regulations.
4.1 All content, trademarks, logos, designs and software on Our website, Apps and Platform are the exclusive property of Bionic Hope Private Limited or its licensors.
4.2 Subject to these Terms, We grant You a limited, non-exclusive, non-transferable, revocable license to use the Services for personal, non-commercial purposes.
4.3 You may not reproduce, modify, distribute, decompile, reverse engineer or create derivative works of any portion of the Services without Our prior written consent.
5.1 Limited Warranty. We warrant that Products will be free from workmanship defects under normal use as follows:
(a) Grippy™ Bionic Hand, BrawnBand® and WeightBand®: one (1) year from date of purchase, covering manufacturing defects only.
(b) Chargers and batteries: six (6) months from date of purchase.
(c) Grippy Mech™: three (3) months from date of purchase.
(d) Consumables (e.g., gloves, carry bags): no warranty.
5.2 Custom Sockets. Sockets fabricated by Clinics are covered only by the Clinic’s optional warranty and subject to physiological changes (e.g., stump volume, muscle sensitivity).
5.3 Exclusions. Warranty does not apply to damage caused by misuse, user negligence, unauthorised repairs, Acts of God, or failure to follow the Instruction Manual.
5.4 Claims. To claim warranty, You must register the Product online, provide proof of purchase, and follow the procedures set out in the Warranty Card.
5.5 Disclaimer. To the maximum extent permitted by law, all other warranties, express or implied, including merchantability and fitness for a particular purpose, are disclaimed.
6.1 We collect personal contact details, physiological evaluation data, body measurements, sensor calibration values, device usage statistics and warranty information (“User Data”).
6.2 User Data is stored on secure servers of our third-party service providers and transmitted via encrypted APIs.
6.3 By using the Services, You consent to collection, storage, processing and transfer of User Data within Our internal ecosystem and to third-party service providers for analytics, R&D and support.
6.4 We implement reasonable security measures and comply with the Information Technology Act, 2000, and Information Technology (Reasonable Security Practices and Procedures and Sensitive Personal Data or Information) Rules, 2011.
6.5 A separate Privacy Policy sets out detailed information on data processing, user rights, grievance redressal and cross-border transfers, which forms part of these Terms.
7.1 Pursuant to the Information Technology Rules, 2021, We have given the Charge of Grievance Officer to our QC Head:
- Address: Grievance Officer
- Email: support@robobionics.in
- Phone: +91-8668372127
7.2 All support tickets and grievances must be submitted exclusively via the Robo Bionics Customer Support portal at https://robobionics.freshdesk.com/.
7.3 We will acknowledge receipt of your ticket within twenty-four (24) working hours and endeavour to resolve or provide a substantive response within seventy-two (72) working hours, excluding weekends and public holidays.
8.1 Pricing. Product and Service pricing is as per quotations or purchase orders agreed in writing.
8.2 Payment. We offer (a) 100% advance payment with possible incentives or (b) stage-wise payment plans without incentives.
8.3 Refunds. No refunds, except pro-rata adjustment where an Individual Consumer is medically unfit to proceed or elects to withdraw mid-stage, in which case unused stage fees apply.
9.1 Users must follow instructions provided by RCI-registered professionals and the User Manual.
9.2 Users and Entity Consumers shall indemnify and hold Us harmless from all liabilities, claims, damages and expenses arising from misuse of the Products, failure to follow professional guidance, or violation of these Terms.
10.1 To the extent permitted by law, Our total liability for any claim arising out of or in connection with these Terms or the Services shall not exceed the aggregate amount paid by You to Us in the twelve (12) months preceding the claim.
10.2 We shall not be liable for any indirect, incidental, consequential or punitive damages, including loss of profit, data or goodwill.
11.1 Our Products are classified as “Rehabilitation Aids,” not medical devices for diagnostic purposes.
11.2 Manufactured under ISO 13485:2016 quality management and tested for electrical safety under IEC 60601-1 and IEC 60601-1-2.
11.3 Products shall only be used under prescription and supervision of RCI-registered Prosthetists, Physiotherapists or Occupational Therapists.
We do not host third-party content or hardware. Any third-party services integrated with Our Apps are subject to their own terms and privacy policies.
13.1 All intellectual property rights in the Services and User Data remain with Us or our licensors.
13.2 Users grant Us a perpetual, irrevocable, royalty-free licence to use anonymised usage data for analytics, product improvement and marketing.
14.1 We may amend these Terms at any time. Material changes shall be notified to registered Users at least thirty (30) days prior to the effective date, via email and website notice.
14.2 Continued use of the Services after the effective date constitutes acceptance of the revised Terms.
Neither party shall be liable for delay or failure to perform any obligation under these Terms due to causes beyond its reasonable control, including Acts of God, pandemics, strikes, war, terrorism or government regulations.
16.1 All disputes shall be referred to and finally resolved by arbitration under the Arbitration and Conciliation Act, 1996.
16.2 A sole arbitrator shall be appointed by Bionic Hope Private Limited or, failing agreement within thirty (30) days, by the Mumbai Centre for International Arbitration.
16.3 Seat of arbitration: Mumbai, India.
16.4 Governing law: Laws of India.
16.5 Courts at Mumbai have exclusive jurisdiction over any proceedings to enforce an arbitral award.
17.1 Severability. If any provision is held invalid or unenforceable, the remainder shall remain in full force.
17.2 Waiver. No waiver of any breach shall constitute a waiver of any subsequent breach of the same or any other provision.
17.3 Assignment. You may not assign your rights or obligations without Our prior written consent.
By accessing or using the Products and/or Services of Bionic Hope Private Limited, You acknowledge that You have read, understood and agree to be bound by these Terms and Conditions.