Step count, cadence, and symmetry may look like small numbers on a wearable device, but for people using lower-limb prosthetics, these numbers tell a deeper story. They show how safely a person moves, how steady they feel, and how well their prosthetic limb supports their daily life. For doctors, these wearable KPIs act like quiet signals that reveal progress long before bigger changes appear in the clinic.
A higher step count often shows growing confidence. A steady cadence reflects balance and rhythm. Good symmetry shows that the user is trusting their prosthetic limb instead of favoring one side. Each metric helps physicians understand real-world mobility in ways that simple clinic tests cannot.
This article explores how these KPIs work, why they matter, and how doctors can use them to guide better decisions in prosthetic care.
Understanding Step Count as a Clinical Signal
Why Step Count Matters in Prosthetic Care
Step count shows how much the user is actually moving in daily life.
It reflects not only strength and balance but also how confident they feel during ordinary tasks.
When step count rises, it often means the user is beginning to trust their body again.
For doctors, step count becomes a real-world measure of physical activity.
It shows whether the user is avoiding movement or actively rebuilding independence.
This helps guide safe decisions about therapy, energy demands, and mobility goals.
Even small changes in daily steps can show meaningful shifts in comfort and confidence.
How Low Step Count Reveals Hidden Problems
A sudden drop in step count often reveals discomfort, fear, or emotional fatigue.
Users may avoid walking because the socket is painful, the knee feels unstable, or the limb feels heavy.
Sometimes the problem is not physical at all.
Stress, sadness, or a recent scare can reduce movement without the user realizing it.
Step count becomes the quiet signal that says something deeper may need attention.
Doctors use these drops to look beyond the numbers and understand the whole person.
How Step Count Shows Recovery Over Time
As the user gets stronger, their daily steps usually rise slowly and steadily.
This upward trend shows that walking is becoming less tiring and more natural.
These improvements may be too small to see inside the clinic.
But wearables capture them in everyday life, where movement truly happens.
Doctors rely on these long-term patterns to shape therapy plans and adjust prosthetic components.
A rising step count often marks a turning point in emotional readiness as well.
How Step Count Supports Goal Setting
Goals become clearer when doctors understand how many steps the user takes each day.
A very low count shows that early goals must be small and gentle.
A higher count shows the user is ready for more challenging tasks.
These goals help users stay motivated.
They can see their steps rising each week, giving them a sense of progress.
This makes rehab feel more personal, hopeful, and achievable.
Step count becomes a simple yet powerful way to guide ambition safely.
Understanding Cadence and Why It Matters
What Cadence Reveals About Comfort

Cadence shows how many steps a person takes in a minute.
A smooth, steady cadence shows that the user feels safe and balanced with their prosthetic limb.
When cadence becomes uneven or slow, it often means something is interrupting this comfort.
The user may hesitate during each step, adjust their posture, or fear losing balance.
These small pauses lower cadence and signal deeper issues.
Doctors study cadence to understand how secure the user feels while walking.
How Cadence Reflects Rhythm and Balance
Walking is a rhythm.
When the user’s steps follow a natural pattern, movement feels easy and controlled.
A steady cadence shows this rhythm is intact.
An irregular cadence shows the rhythm is disrupted, often by pain, fear, or misalignment.
These changes appear even before the user says something feels wrong.
Cadence helps doctors catch subtle balance issues early, making rehab more effective.
Rhythm becomes a window into real-world safety.
How Cadence Shows Physical Endurance
As muscles get stronger and the prosthetic becomes more familiar, cadence naturally increases.
A higher cadence shows better endurance and stronger control over each step.
When cadence falls as the day goes on, it may show fatigue or mechanical strain.
Doctors use this information to design therapy that builds stamina in a safe and gradual way.
Cadence becomes a way to measure how long the user can walk before tiring.
How Cadence Helps Reveal Emotional State
People who feel confident and hopeful tend to walk with steadier, livelier steps.
People who feel nervous or stressed often move more cautiously and slowly.
Cadence captures these emotional shifts clearly.
A drop may show that the user is troubled, even if they do not speak about it.
An increase may show renewed confidence or joy.
Doctors use cadence to understand how emotions shape movement.
Understanding Symmetry and Its Clinical Importance
What Symmetry Shows About Trust
Symmetry shows how evenly the user loads their sound limb and their prosthetic limb.
Good symmetry means the user trusts the prosthetic side with real weight and real movement.
Poor symmetry means the user is protecting that side, often without noticing.
They may rely heavily on the sound limb, creating long-term strain and imbalance.
This protection slows recovery and increases injury risk.
Symmetry becomes a marker of trust — physical and emotional.
How Asymmetry Reveals Pain
When something hurts — even slightly — the body shifts its weight away from discomfort.
This creates uneven steps, shortened stride, and reduced loading on the prosthetic side.
These patterns appear clearly in symmetry measurements.
Even mild pressure issues, subtle skin irritation, or loose sockets can cause asymmetry.
Doctors use symmetry to detect early signs of pain long before it becomes serious.
How Symmetry Predicts Long-Term Health
Poor symmetry increases stress on the spine, hips, and sound limb.
Over years, this can lead to injury or chronic pain.
When doctors see improving symmetry, they know the user is moving toward safer long-term health.
It shows the prosthesis is supporting the body correctly.
It also means the user is developing confidence in each step.
Symmetry protects the user’s future mobility.
How Symmetry Helps Guide Prosthetic Adjustments
When symmetry is poor, prosthetic alignment may need attention.
The foot may be angled slightly too far inward or outward.
The knee may swing too quickly or slowly.
The socket may shift during weight bearing.
These small mechanical issues often appear first as asymmetric walking.
By correcting them, doctors restore comfort, confidence, and gait stability.
Symmetry becomes a valuable clinical signal for precision adjustments.
How Wearable Devices Capture These KPIs
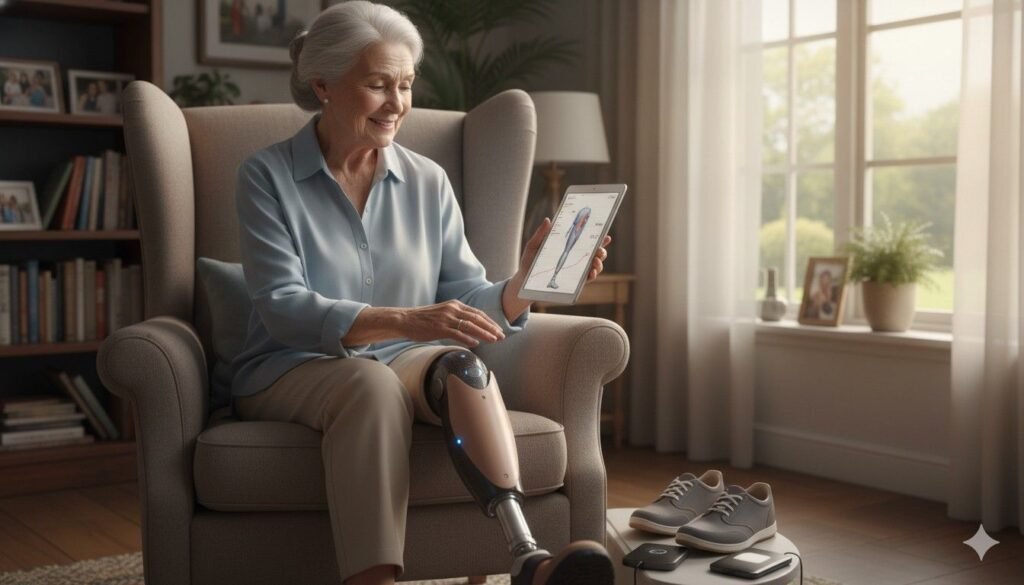
Why Wearables Offer a Clearer Picture of Daily Life

In the clinic, people often walk differently because they know they are being observed.
They may push harder for a short test or feel nervous about being judged.
Wearables remove this pressure.
They capture movement in the user’s natural environment — at home, at work, or in the community.
This gives doctors accurate insight into how the user truly moves every day.
Because wearables record thousands of steps, the data becomes rich, honest, and meaningful.
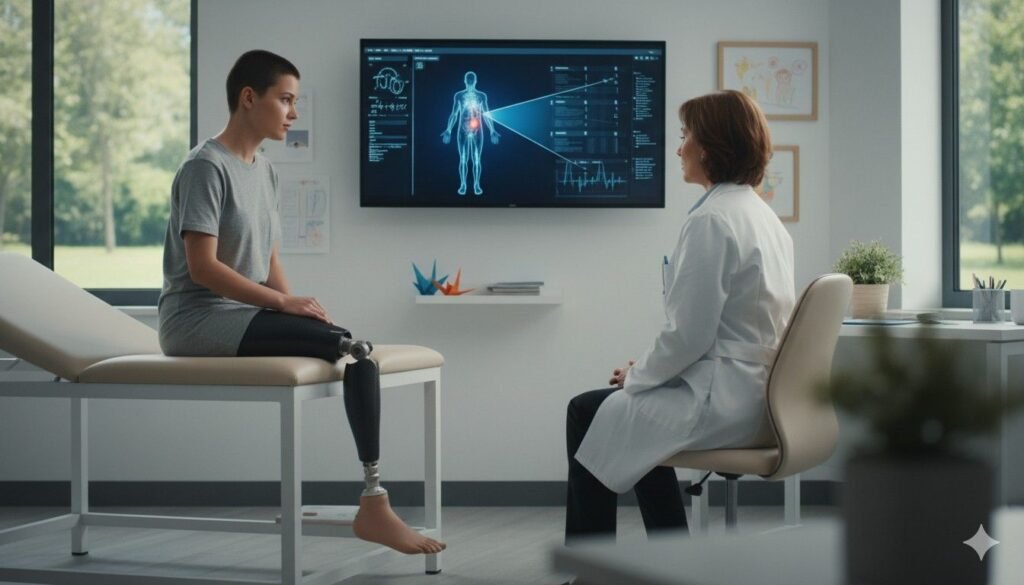
How Continuous Data Shows Real Patterns
A single walk test shows just a moment in time.
But wearables track the user’s movement across the entire day.
This shows when step count rises or falls, when cadence changes, and when symmetry improves.
It reveals whether progress is steady, fluctuating, or stalled.
Doctors use these patterns to spot trends that may not appear during a brief clinic visit.
Continuous data tells the story of real progress.
How Wearables Capture Micro-Changes
Tiny changes — like increasing 200 steps per day or adding one step per minute of cadence — can signal major victories.
These changes are often too small to notice through observation alone.
Wearables pick them up with precision.
They help doctors celebrate progress early, even when improvements feel invisible to the user.
They also catch declines at the earliest stages, allowing quick intervention.
Micro-changes often show the heart of recovery.
How Wearables Help With Personalized Planning
Each user has their own pace, history, fears, and strengths.
Wearable data helps doctors build plans that match these personal realities.
If step count rises quickly, rehab can progress faster.
If cadence stays low, balance training may be needed.
If symmetry improves suddenly, it may mean an alignment change was successful.
Personalized plans feel safer, more achievable, and more encouraging for the user.
How Doctors Interpret Step Count in Clinical Practice
How Step Count Shows Readiness for New Activities
When users begin walking more each day, it often means they feel confident enough to explore new challenges.
Doctors watch for steady rises in step count to introduce tasks like stairs, slopes, or longer walking sessions.
If step count drops, it may be too early to add complexity.
The body or emotions may need more time to adjust.
This makes step count a gentle guide for pacing progress.
How Step Count Reflects Motivation
Movement rises when users feel hopeful and motivated.
A growing step count often shows rising excitement about recovery.
It may even signal growing interest in returning to previous hobbies or routines.
A drop in step count may show discouragement or fatigue.
Doctors use these signals to offer support and adjust goals to keep the user motivated.
Step count becomes a conversation starter about emotional well-being.
How Step Count Supports Return-to-Work Decisions
Work may require long days and steady movement.
Step count helps doctors understand whether the user has enough stamina.
If the user consistently reaches healthy step counts, they may be ready for more active work tasks.
If step count remains low, part-time or modified duties may be safer.
These decisions protect users from burnout and build confidence gradually.
How Step Count Helps Prevent Sedentary Patterns
A low step count across weeks may show that the user is becoming less active.
This can lead to weight gain, muscle weakness, and emotional strain.
Doctors can use these numbers to start early conversations about healthy routines.
Gentle encouragement can help the user re-engage with movement in a safe way.
Step count becomes a protective tool for long-term health.
How Doctors Interpret Cadence in Clinical Practice
How Cadence Shows Walking Confidence
Cadence rises naturally when the user feels safe and comfortable.
When steps flow together without hesitation, cadence becomes smooth and predictable.
This steady pace shows the user trusts their prosthetic limb and feels balanced on both sides.
If cadence becomes uneven or slow, it often means the user is unsure about each step.
They may feel that the limb is not responding the way they expect, or that their posture feels unstable.
Doctors use these subtle shifts to understand how secure the user feels inside their body.
Cadence reveals confidence even more clearly than spoken words.
How Cadence Helps Identify Gait Deviations
Changes in cadence often signal early deviations in gait.
An uneven step pattern may show the user is swinging the leg too far, shortening stride, or leaning to compensate for discomfort.
These deviations may not be visible to the user, but cadence picks them up instantly.
A drop may show a new compensation pattern forming.
A sudden rise may reflect a breakthrough in balance and rhythm.
Doctors rely on cadence to catch these shifts before they create long-term habits.
How Cadence Helps Evaluate Energy Use
Walking takes effort, especially for new prosthetic users.
If cadence drops sharply during the day, it may show that the user is becoming fatigued too quickly.
Fatigue can come from weak muscles, a heavy prosthetic limb, or emotional stress.
It may also show that the user is overexerting themselves at certain times of the day.
By monitoring cadence fluctuations, doctors can create pacing strategies that protect both safety and stamina.
This makes daily life feel lighter and more manageable for the user.
How Cadence Supports Rehab Timing
Every rehab program has its own rhythm.
Users improve in stages, and cadence helps show where they are in that cycle.
A stable cadence shows the user is ready for more challenging activities, such as faster walking, controlled turns, or outdoor paths.
A drop in cadence signals that the user needs time to build strength or rediscover confidence.
This helps doctors avoid pushing too fast or holding back too much.
Cadence quietly shapes the pace of recovery.
How Doctors Interpret Symmetry in Clinical Practice
How Symmetry Reveals True Limb Confidence
When a user loads both limbs evenly, it shows deep trust in the prosthetic side.
This trust is essential for long-term health because it prevents overuse of the sound limb.
When symmetry is poor, it often means the user is unsure about placing full weight on the prosthetic side.
They may fear pain, instability, or loss of balance.
Doctors use symmetry data to understand whether the prosthesis feels like a natural extension of the body.
If symmetry improves, it means confidence is growing beneath the surface.
How Symmetry Helps Detect Alignment Issues
Even small changes in alignment can shift weight distribution dramatically.
A slightly rotated foot, a tilted socket, or a misaligned knee can make the user favor one side without noticing.
Asymmetry shows up immediately in wearable data.
It reveals uneven step lengths, uneven stance times, and uneven weight distribution.
Doctors can use these early signs to adjust alignment before discomfort grows.
These adjustments often lead to instant improvements in comfort and stability.
How Symmetry Supports Sound Limb Protection
The sound limb carries extra stress when symmetry is poor.
This can lead to knee pain, hip strain, or long-term joint issues.
Wearable symmetry data helps doctors ensure the sound limb is not doing too much work.
When symmetry improves, it means the user is moving in a safer, more balanced way.
This protects the user’s future mobility and reduces the risk of overuse injuries.
How Symmetry Guides Therapy Interventions
Therapists use symmetry patterns to design precise training plans.
If the user loads the prosthetic limb too lightly, therapy focuses on weight-bearing and side-to-side stability.
If the sound limb is overloaded, therapy helps reduce reliance on that side.
Symmetry drives these decisions with clarity.
It makes rehab more accurate and more personal.
Using Wearable KPIs to Shape Rehabilitation
How Step Count Shapes Daily Activity Plans
Step count helps doctors determine how active the user is across the day.
If steps are low, a gentle activity plan may help the user build confidence.
If steps are high but uneven, pacing strategies may protect against fatigue.
Doctors use step count patterns to recommend safe daily routines — not too much, not too little.
This keeps the user active without overwhelming them.
Over time, step count becomes a daily guide for sustainable movement.
How Cadence Shapes Strength and Balance Training
When cadence remains slow or uneven, specific exercises can help rebuild rhythm.
Strength work for the hips, core, and pelvic muscles often improves cadence dramatically.
Balance training also makes stepping more consistent and controlled.
Wearables help doctors see how cadence changes after each training period.
If cadence rises after strengthening, the plan is working.
If cadence stays low, the user may need more targeted work.
Cadence turns therapy from guesswork into precision.
How Symmetry Shapes Gait Retraining
Symmetry issues are common early in rehab.
Wearable data helps therapists understand exactly where the imbalance lies.
If the user spends too little time on the prosthetic limb, training may include controlled weight shifts, walking with feedback, or functional tasks like stepping sideways.
If the sound limb is overused, therapy may include strengthening of the prosthetic side and alignment adjustments.
Symmetry-guided retraining creates safer, more natural gait patterns.
How Wearable KPIs Support Emotional Coaching
Movement improves faster when users feel supported emotionally.
Wearable KPIs help doctors see when a person is discouraged, hesitant, or anxious.
A drop in step count may show fear.
A decline in cadence may show sadness or fatigue.
A shift in symmetry may show stress or insecurity.
These clues help doctors open gentle conversations about emotional challenges.
This makes recovery more compassionate and more human.
How Wearable KPIs Help Prevent Falls
How Step Count Shows Fall Avoidance
Users often reduce their daily steps after a fall or near-fall.
Even if they don’t mention it, their wearable data shows they are avoiding movement.
Doctors monitor step count to understand how fear shapes daily activity.
A drop may signal a hidden fall risk that needs attention.
Early support helps prevent future accidents and rebuild trust.
How Cadence Reveals Instability
Instability often shows up first as slowing cadence.
When stepping feels risky, the user walks more cautiously, reducing their pace.
A drop in cadence may show joint weakness, poor alignment, or trouble with the knee or foot mechanism.
It may also reveal declining balance.
This helps doctors intervene early with stability training or component adjustments.
How Symmetry Helps Predict Falls
Uneven loading makes falls more likely.
When the user relies too heavily on one side, they become unsteady during turns or when stepping on uneven surfaces.
Wearables show these asymmetric patterns clearly.
Doctors use this information to correct gait early and prevent dangerous situations.
How Combined KPIs Give a Full Risk Profile
Step count, cadence, and symmetry together create a complete picture of fall risk.
A decline in all three signals serious instability.
A change in just one signals a smaller but still important risk.
Doctors rely on this combined view to design fall-prevention plans that are proactive rather than reactive.
This protects the user’s long-term safety.
Wearable KPIs and Long-Term Prosthetic Success
How KPIs Guide Annual Prosthetic Reviews
Prosthetic needs shift every year as the user’s body changes.
Wearable KPIs help doctors see how these changes affect movement.
A slow drop in cadence or symmetry over months may show the socket is loosening or alignment is drifting.
A rise in step count may show that the user has outgrown their current foot or knee.
KPIs ensure the prosthesis evolves with the user.
How KPIs Predict Component Upgrade Needs
When users begin moving more, they often need components that can support higher activity.
A steady rise in cadence and symmetry may show they’re ready for a more dynamic foot or a microprocessor knee.
KPIs provide clear evidence for recommending advanced technology.
They help match components to real activity level.
How KPIs Support Healthy Aging
As users age, their movement patterns naturally shift.
Wearables help doctors track these changes gently and accurately.
A gradual decline in symmetry may show weakening muscles.
A drop in cadence may show fatigue or joint stiffness.
These insights help doctors adjust therapy and keep users active.
Aging becomes smoother with clear data to guide choices.
How KPIs Strengthen User Independence
People feel more empowered when they see their own progress.
Wearable KPIs give them real numbers that reflect their everyday triumphs.
A rising step count shows stronger confidence.
A smoother cadence shows improving rhythm.
Better symmetry shows deeper trust in the prosthetic limb.
These small wins help users stay motivated for life.
Using Wearable KPIs to Guide Prosthetic Adjustments
How Step Count Reveals Fit Issues
A drop in daily steps can signal that the prosthesis no longer feels comfortable.
The user may avoid movement because the socket rubs, the limb feels heavy, or the suspension feels insecure.
These discomforts show up in behavior long before a clinic visit.
When doctors see step count declining over days or weeks, it tells them to investigate fit.
Even when users do not describe pain clearly, numbers show the story.
Adjusting the socket or suspension often restores comfort and step count together.
Step count becomes a reliable way to identify fit problems early.
How Cadence Shows Knee and Foot Performance
Changes in cadence often reflect how well the prosthetic foot or knee responds during walking.
If the knee swings too slowly or too quickly, cadence becomes irregular.
If the foot lacks proper energy return, steps become heavier and slower.
Doctors use cadence to understand whether components are supporting the user’s rhythm.
If cadence improves after adjusting the foot stiffness or knee timing, it confirms the alignment is moving in the right direction.
Cadence becomes a guide for fine-tuning performance.
How Symmetry Exposes Alignment Shifts
Alignment changes can be subtle and difficult to see by eye.
Even small rotations or angling of the foot can pull the body out of balance.
Wearable symmetry data shows these shifts with clarity.
When one side consistently bears more weight or takes longer steps, it reveals that alignment needs correction.
After adjustments, symmetry often improves immediately.
Symmetry helps doctors protect the body from long-term strain.
How Combined KPIs Improve Component Selection
When step count, cadence, and symmetry all rise together, it shows the user is thriving with their prosthetic setup.
When one metric drops sharply, it shows the component may not be meeting their needs.
Doctors rely on these combined signals to recommend advanced feet, knees, or suspension systems.
These upgrades become guided by proof, not guesswork.
Wearables create a more accurate and compassionate decision-making process.
The Emotional Layer Behind Wearable KPIs
How Step Count Reflects Mood and Motivation

People walk more when they feel hopeful, supported, and motivated.
A rising step count often signals joy, stronger self-belief, or pride in progress.
When step count drops, it may reflect sadness, stress, or discouragement.
The user may stay indoors more or avoid activities they once enjoyed.
These emotional shifts appear clearly in their movement patterns.
Doctors use step count as a gentle indicator of emotional well-being.
It helps them open caring conversations that support the user beyond physical training.
How Cadence Reveals Internal Tension
When a user is tense, worried, or overwhelmed, their cadence slows.
They move more cautiously, take shorter steps, and hold more tension in their body.
This tension can come from fear of falling, worry about pain, or stress in daily life.
Cadence shows these emotional signals long before the user says anything aloud.
By noticing these changes, doctors can offer reassurance and adjust therapy to meet emotional needs.
This creates a safer, more comforting recovery environment.
How Symmetry Shows Hidden Fear
When users fear loading the prosthetic limb, they naturally shift weight to the sound limb.
This protectiveness shows up clearly in symmetry data.
Sometimes the user doesn’t realize they are avoiding the prosthetic side.
Wearables reveal these hidden fears and help doctors gently address them.
This may involve confidence-building exercises or adjusting the prosthesis to feel more stable.
Symmetry becomes a reflection of trust — and trust takes time to grow.
How Wearable KPIs Build User Confidence
As users see their own numbers improve, it strengthens their belief in their ability to walk safely and confidently.
A rising cadence or a steady symmetry score becomes proof that recovery is happening.
These small wins create emotional momentum that supports long-term success.
Wearables turn recovery into a story the user can see, understand, and celebrate.
How Wearable KPIs Support Return-to-Community Mobility
How Step Count Helps Prepare for Outdoor Walking
Community environments require consistent movement and steady endurance.
Wearables show how ready the user is by tracking whether their daily steps are rising.
If steps remain very low, outdoor walking may feel overwhelming.
If steps rise steadily, the user may be ready to explore parks, markets, and public spaces.
Doctors use step count trends to prepare the user for community challenges at the right time.
How Cadence Helps With Public Navigation
Crowded areas require quick reactions.
A controlled cadence means the user can adjust to people walking in different directions, narrow walkways, or sudden changes in pace.
If cadence remains low or inconsistent, community environments may stress the user.
Doctors can design training that builds quicker stepping and stronger balance.
Cadence becomes a sign that the user is ready for real-world mobility.
How Symmetry Supports Uneven Surfaces
Public spaces rarely offer perfect flooring.
Streets, ramps, bus platforms, and outdoor paths challenge the user’s balance.
Good symmetry helps the user manage these surfaces without leaning heavily to one side.
Poor symmetry increases the risk of stumbles and strains.
Wearable symmetry data helps doctors prepare the user for these environments safely.
How KPIs Reflect Community Confidence
Confidence in public spaces grows slowly.
When step count, cadence, and symmetry all rise during days spent outdoors, it shows the user is becoming more comfortable moving around others.
When any KPI drops, it may show anxiety, confusion, or overstimulation.
Doctors use these insights to pace community exposure in a supportive way.
KPIs reflect how deeply the user feels safe in the world beyond their home.
The Role of Wearable KPIs in Long-Term Health
How Step Count Supports Heart and Joint Health
Walking is the simplest and most powerful way to maintain heart and joint health.
Higher step counts show that the user is staying active and protecting their long-term mobility.
Low step counts may signal rising health risks like stiffness, weight gain, or weak muscles.
Doctors use this information to encourage gentle but steady activity.
Step count becomes a vital sign for lifelong health.
How Cadence Reflects Aging Changes
As people age, their cadence naturally slows.
Wearables help doctors track this shift carefully to understand whether it is normal aging or an early sign of decline.
If cadence drops sharply, it may show pain, weakness, or emotional worry.
A stable cadence shows aging is being managed well with the prosthesis.
This helps sustain safe movement for many years.
How Symmetry Protects the Sound Limb
Over time, uneven loading can strain the sound knee and hip.
This increases the risk of arthritis and joint pain.
Good symmetry spreads stress evenly across the body, reducing long-term wear.
Doctors use wearable symmetry data to ensure the sound limb remains protected.
Users move toward a healthier future when symmetry improves.
How KPIs Shape Lifelong Activity Plans
Wearables give doctors insight into how the user moves across different seasons of life.
They show when activity rises, when it slows, and when support is needed.
These patterns help doctors design long-term plans that match the user’s evolving needs.
Daily walking becomes a lifelong habit supported by real numbers.
KPIs guide mobility beyond rehabilitation into long-lasting independence.
Conclusion
Step count, cadence, and symmetry offer a simple but powerful window into the lives of lower-limb prosthetic users.
They reflect how much the person moves, how steady they feel, and how confidently they trust their prosthetic limb.
These wearable KPIs help doctors make precise decisions that shape safer, smoother, and more meaningful recovery paths.
Step count reveals daily activity and emotional courage.
Cadence reflects balance, rhythm, and inner confidence.
Symmetry shows trust, comfort, and long-term health.
Together, they create a full picture of real-world mobility that clinic tests alone cannot provide.
At Robobionics, we believe every step matters.
Our mission is to build advanced, affordable prosthetic limbs that support natural movement, real independence, and a life filled with possibility.
By combining thoughtful design with compassionate care, we help users walk with confidence — step by step, day by day.
If you’d like to see how Robobionics can support better outcomes for your patients, you can always book a demo through our website.
We would be honored to walk this journey with you.



