Walking on a flat floor tells only a small part of a prosthetic user’s story.
Real life happens on stairs, ramps, gravel paths, broken roads, and places where the ground is never perfectly smooth.
For doctors and physical therapists, these uneven spaces reveal how strong, stable, and confident a user truly feels with their prosthesis.
Functional outcome tests built for stairs, slopes, and unstable surfaces help clinicians see what the user can handle today and what they may need tomorrow.
Why Real-World Mobility Matters in Prosthetic Care
How Uneven Surfaces Reveal True Ability
Flat floors hide challenges.
Almost anyone can walk straight and steady on a smooth surface, even with balance issues or a poor socket fit.
But uneven ground shows the truth.
It reveals how well the user stabilizes their body, controls their steps, and trusts their prosthesis when every inch of the surface feels different.
In daily life, people step over stones, avoid potholes, climb stairs at home, and walk on slippery ramps in public places.
These movements demand strength, coordination, and confidence that simple indoor walking cannot measure.
This is why clinicians rely on functional tests made for non-flat surfaces.
Why MDs and PTs Need Specialized Functional Tests
Doctors track healing, limb health, and pain.
Therapists track balance, posture, and movement skill.
Both need clear, structured ways to measure how the user performs on surfaces they face every day.
Tests for stairs, slopes, and uneven terrain allow teams to see if the prosthesis supports safe movement under stress.
These tests help them understand whether the user needs training, alignment changes, or a new socket.
They also help predict fall risk before injuries happen.
The Link Between Real-Life Tasks and Long-Term Independence
A prosthesis becomes valuable only when it helps the user move through the world without fear.
When a person can climb stairs confidently, face a slope without slipping, and walk on rough paths without feeling unstable, they feel more independent.
This independence shapes their emotional strength, their physical health, and their overall quality of life.
Functional outcome tests give doctors the information they need to build this independence step by step.
Understanding Stair-Based Functional Tests
Why Stairs Challenge Prosthetic Users Deeply

Stairs require a strong sense of balance, a stable core, and trust in the prosthetic side.
Going up demands power and forward drive.
Going down demands control, slow movement, and careful weight placement.
Even small discomfort in the socket or poor suspension becomes obvious on stairs.
The user may hesitate, grip railings tightly, or lean heavily on the sound side.
These reactions show clinicians exactly where the problem lies.
What Stair Tests Aim to Measure
Stair-focused tests explore how the user handles:
upward stepping, downward stepping, controlled descent, foot placement, rhythm, and confidence during repetitive steps.
The goal is not speed.
The goal is safety, posture, and step quality.
These tests show how the prosthesis supports functional strength in both legs.
What Stair Performance Reveals About Fit and Alignment
If the socket fits poorly, the user may feel unstable when lifting the prosthetic side onto the next step.
If alignment is off, the knee may buckle or the user may shift weight awkwardly.
If suspension is weak, the limb may feel like it is moving inside the socket.
These signs help clinicians refine the device to restore safety and confidence.
Understanding Slope and Ramp Functional Tests
Why Slopes Are Harder Than Flat Ground
Slopes demand a constant shift in body mechanics.
Walking uphill pushes the hip and knee into stronger activation.
Walking downhill requires slow, controlled movements that place more stress on the sound side.
For prosthetic users, both directions feel challenging because ground forces change with every step.
This tests balance, endurance, and control far more than normal walking.
What Clinicians Look for During Ramp Tests
Clinicians observe how much the user leans, how quickly they fatigue, and how steady their steps look.
They also watch how the prosthetic foot reacts on the incline—whether it rolls smoothly or feels unstable.
Good performance shows that the foot design, alignment, and socket fit all work together.
Poor performance shows that something is making movement unsafe.
How Slope Tests Reveal Strength and Confidence
Slopes force the user to trust their prosthesis fully.
If fear or hesitation appears, it often means deeper training needs are present.
Slope tests reveal balance limits, strength deficits, and mental barriers that might not appear on flat surfaces.
Understanding Uneven Terrain Functional Tests
Why Uneven Surfaces Are the Real Test of Mobility
Real life is rarely smooth.
People walk across gravel, grass, broken pavements, shop floors, sandy paths, and wet ground.
Each step feels different, making balance harder and body reactions less predictable.
For prosthetic users, uneven terrain tests how well they adapt when the ground itself changes beneath their feet.
What Clinicians Observe on Rough Ground
They watch how the user shifts weight, how often they pause, and whether they look at the ground constantly.
They also observe any sudden movements, stumbles, or stiff posture.
These reactions show whether the prosthesis supports reactive balance and shock absorption—two key parts of safe mobility.
How Uneven Terrain Testing Helps Prevent Falls
Most falls happen outdoors, not inside clinics.
Testing on rough ground reveals hidden risks early.
Clinicians can then teach safer walking techniques, adjust alignment, or recommend foot designs that improve stability.
How Clinicians Break Down Real-World Functional Ability
Separating Strength From Skill

A user may be strong enough to climb stairs but still fear them.
Or they may feel confident but lack the physical ability to control their movements safely.
Stair, slope, and uneven ground tests help clinicians see whether the issue is strength, confidence, or both.
This allows them to design better training plans.
Identifying Movement Compensations
Prosthetic users often lean, twist, or shorten steps to protect themselves.
These compensations may help in the short term but cause long-term pain in the back, hips, or sound side knee.
Functional tests expose these compensations clearly so clinicians can correct them early.
Understanding Speed vs Safety
Users sometimes rush through tasks to “get them over with.”
Others move too slowly because they fear slipping.
Both patterns show deeper issues that stair and terrain tests help uncover.
Clinicians use this information to guide safe walking habits that protect the patient long-term.
How Socket Fit Influences Real-World Movement
The Connection Between Fit and Confidence
A good socket creates calmness in the user’s mind.
They know the prosthesis will stay secure during each step.
A poor socket creates fear because the limb may slip, rotate, or cause pain on impact.
Stairs and slopes make this difference obvious.
How Fit Affects Power
Going uphill requires strong hip drive.
If the socket distributes pressure poorly, the user cannot produce enough power.
They may resort to pulling themselves upward using railings.
This reveals the need for immediate adjustments.
How Fit Affects Control
Going downhill demands slow and steady braking.
If the socket does not hug the limb securely, the user cannot control descent safely.
This increases fall risk and reduces confidence outdoors.
How Foot Design Shapes Stair and Terrain Performance
Why Foot Mechanics Matter
Prosthetic feet behave differently depending on their design.
Some feet offer strong push-off for going uphill.
Others offer stable braking for going downhill.
Some feet adapt to uneven ground better than others.
Functional testing helps clinicians determine whether the foot matches the user’s lifestyle.
Understanding How Energy Return Affects Movement
Feet with more energy return help users climb stairs with less effort.
Feet with less return may feel heavy, causing fatigue and slow steps.
Testing on slopes shows whether the foot supports smooth rolling without sudden jolts.
Understanding How Terrain Adaptation Improves Stability
Some feet bend and twist slightly to match uneven ground.
Others stay rigid.
Uneven terrain tests show whether the foot absorbs shocks or forces the user to overcompensate.
How Alignment Affects Stairs, Slopes, and Rough Ground
How Small Alignment Changes Affect Big Movements
Alignment may look like a small technical detail, but it shapes every step.
Even a slight forward or backward shift can change how the prosthesis behaves on stairs, slopes, and uneven surfaces.
If alignment is off, the knee may feel unstable, the foot may not roll smoothly, or the user may feel shock with every step.
Functional tests on challenging surfaces show these problems clearly.
They reveal whether alignment helps the user move safely or forces them into compensations that drain energy and increase fall risk.
Alignment Errors That Show Up on Stairs
When alignment tilts backward, users often struggle to lift the prosthetic foot onto the next step.
This forces them to drag the foot or push harder with the sound side.
If alignment tilts forward, the knee may feel unsafe during descent, causing hesitation or stiff stepping.
These reactions help clinicians identify which adjustments will restore smooth, natural movement.
Alignment Errors That Show Up on Slopes
On slopes, even tiny alignment mistakes become amplified.
If the foot is too angled, the user might feel like they are sliding down while descending.
If the alignment pushes too far forward, the user may struggle to push uphill.
Slope tests provide clinicians with clear insights into how alignment supports or limits movement under changing ground forces.
How Clinicians Use Functional Tests to Guide Training
Building Confidence Before Skill
Users often fear stairs and slopes long before they struggle physically.
The mind reacts to uncertainty by tightening muscles and reducing movement.
Clinicians watch this fear during tests and help users rebuild trust gently.
By teaching simple, safe steps first, the user learns how to relax, breathe, and trust their body again.
This emotional foundation allows skill training to progress smoothly.
Strengthening the Right Muscle Groups
Stair and slope performance often depends on hip strength, core stability, and glute control.
Weakness in these areas becomes obvious during uneven terrain tests.
Clinicians then design targeted exercises to improve power, balance, and endurance so that daily tasks feel easier over time.
Teaching Safe Weight Shifting
Uneven surfaces require constant micro-adjustments in weight.
Prosthetic users often avoid shifting fully onto the prosthetic side due to fear or discomfort.
Functional tests show this avoidance clearly.
Clinicians use specific drills to help users trust weight transfer, improving stability in daily life.
Improving Step Timing and Rhythm
Natural movement relies on rhythm.
When steps become uneven, slow, or overly cautious, it signals a deeper coordination challenge.
Stair and slope tests reveal exactly where timing breaks down.
Therapists then use guided walking, metronome practice, or controlled step drills to restore smooth rhythm.
How Functional Outcome Tests Guide Prosthetic Adjustments
When a Socket Update Is Needed
If the user avoids stairs or slopes due to pain, pressure, or instability, the socket may be the root cause.
Functional tests show how the socket behaves under real stress—not just gentle walking.
Issues like gapping, rotation, or pinching become more obvious on uneven surfaces.
Clinicians use this information to fine-tune or rebuild the socket for better safety and comfort.
When Foot Selection Needs Review
Some users feel strong on flat surfaces but struggle immediately on ramps or gravel.
This often indicates that the foot design does not match their daily needs.
Functional tests help clinicians choose a foot that bends, grips, or returns energy in ways that support the user’s lifestyle.
This prevents long-term frustration and improves real-world independence.
When Alignment Must Be Corrected
Misalignment can cause knee instability, foot slippage, or excessive strain on the sound leg.
Stairs and slopes magnify these problems.
How Surface-Based Tests Predict Fall Risk
Identifying Early Signs of Instability
Most falls happen during unexpected movements—tripping on a stone, stepping off a curb, or slipping on a slope.
Functional tests recreate controlled versions of these moments so clinicians can spot danger signs.
If the user grabs railings tightly, pauses often, or shows stiff posture, it signals instability.
These cues help clinicians act early and reduce fall risk.
Understanding Compensations That Lead to Injury
Some users lift their hip too high, overbend the knee, or lean heavily to one side when walking on uneven surfaces.
These compensations cause long-term pain and joint stress.
Functional tests reveal these patterns before they cause injury, allowing clinicians to correct them quickly.
Tracking Improvements Over Time
As the user trains and the device is adjusted, performance on slopes and rough ground improves.
Their steps become smoother, posture improves, and they rely less on the sound side.
Regular testing helps clinicians track this progress clearly and document safer movement patterns.
How Doctors and PTs Work Together Using Functional Tests
Doctors Monitor Medical Safety
MDs use test results to track stump health, wound condition, joint safety, and overall healing.
They ensure that stair or slope training does not strain the limb, hurt the skin, or create new medical risks.
Functional tests give doctors visible evidence of how the limb responds to real movement.
Therapists Build Skills Step by Step
PTs use these tests to design personalized training routines.
They help users improve balance, strength, posture, and coordination based on test findings.
They also teach safe techniques for climbing stairs, descending slopes, and handling rough terrain.
This teamwork gives the user complete protection and guidance.
Shared Decisions Lead to Better Outcomes
Doctors and therapists combine their test findings to plan the next steps—socket changes, foot upgrades, training intensity, or alignment checks.
This collaboration ensures that the user receives care that matches their real-world needs.
How Functional Tests Improve Daily Life for Prosthetic Users
Walking More Confidently Outdoors
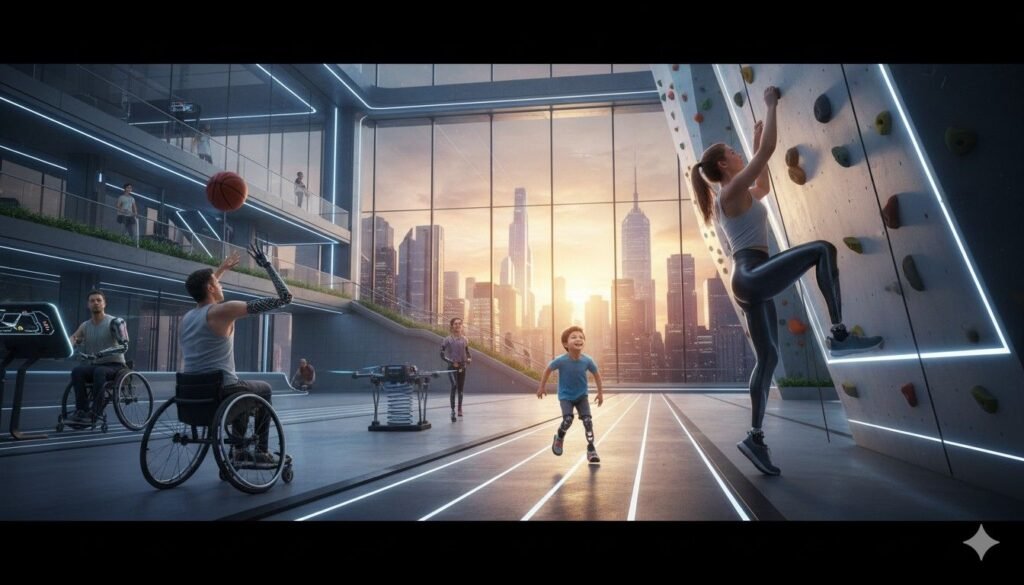
When users master slopes and uneven terrain, outdoor movement becomes easier.
They feel safer walking to the market, traveling through busy streets, or visiting parks.
This freedom strengthens emotional well-being and social participation.
Moving Around the Home With Ease
Homes often include stairs, steps, and uneven flooring.
As stair confidence grows, users feel more independent inside their homes—climbing easily, moving freely, and performing daily tasks without fear.
Reducing Long-Term Wear and Tear
Functional tests help prevent compensatory habits that harm the back, hips, and sound-side knee.
By correcting these early, clinicians protect long-term physical health and reduce future complications.
How Clinics and Rehab Centers Can Use Functional Tests to Strengthen Their Practice
Turning Real-World Testing Into a Competitive Advantage
Clinics and rehab centers that rely only on flat-ground walking tests often miss deeper mobility issues that shape long-term patient success.
This gap affects patient satisfaction, referral strength, and even the clinic’s reputation in the community.
By adopting stair, slope, and uneven-terrain testing as a standard part of assessment, a clinic signals a higher level of care.
It shows commitment to real-world outcomes—not just clinical performance.
This immediately positions the facility as forward-thinking and patient-centered, which strengthens trust with surgeons, referrers, and payors.
Clinics that use these tests consistently can market themselves as specialists in “real-life mobility training,” something patients value deeply and families look for when choosing a provider.
Documenting Real-World Function for Stronger Communication With Surgeons
Surgeons often receive limited feedback from therapy teams about how their patients perform on complex surfaces.
Functional outcome tests create clear, structured data that surgeons can trust.
When a clinic reports stair cadence, slope control, and uneven terrain stability—not just walking distance—it gives surgeons meaningful evidence of recovery progress.
This strengthens professional relationships, improves cross-department collaboration, and increases the likelihood that surgeons will refer future cases to the center.
Surgeons want partners who help their patients return to safe, independent movement.
These tests prove the clinic is delivering that.
Improving Payor Confidence Through Measurable, Surface-Specific Results
Insurance companies want objective proof that a patient is improving and that the interventions provided are necessary.
Stair and terrain test scores give quantifiable evidence of real functional gain, making it easier for clinics to justify ongoing therapy, socket changes, or prosthetic upgrades.
Payors respond positively to clear, measurable progress.
Clinics that show consistent data from stair and slope tests can strengthen authorization requests and reduce the likelihood of denials.
This improves financial predictability and reduces time spent appealing rejected claims.
Creating Premium Training Programs That Add Value
Clinics can turn surface-based mobility training into specialized programs that attract more patients and partnerships.
For example:
A “Confident Stairs Program” for new amputees.
A “Safe Outdoor Walking Program” for community reintegration.
A “Return-to-Work Terrain Readiness Program” for industrial workers or active adults.
These programs not only improve patient outcomes but also differentiate the clinic’s services.
They can be highlighted in marketing materials, community awareness campaigns, and surgeon education sessions.
Using Functional Tests to Guide Staff Training and Skill Development
Functional tests help clinical leaders understand where their team excels and where skills need improvement.
If several patients struggle with slopes due to confidence issues, staff may need new coaching techniques.
If uneven terrain reveals recurring compensations, PTs may benefit from advanced gait-training workshops.
This data-driven approach helps clinics invest in training that directly improves patient outcomes—and that efficiency becomes a business strength.
Creating a Unified Language Across the Team
Functional outcome tests become a shared language between prosthetists, therapists, and physicians.
Everyone discusses mobility using the same terms—slope control, descent quality, foot placement, stabilization time—reducing confusion and improving coordination.
This clarity boosts productivity, reduces miscommunication, and leads to faster problem-solving for each patient.
Why These Tests Matter for Hospital and Rehab Outcomes
Faster Identification of Problems
Functional tests reveal issues earlier than simple flat-ground walking.
This helps hospitals intervene faster, reducing delays and preventing setbacks during rehabilitation.
Better Data for Documenting Progress
Stair, slope, and uneven terrain scores provide clear, measurable evidence of improvement.
This helps clinicians track recovery, justify care decisions, and support insurance documentation.
More Predictable Discharge Planning
When users show safe performance across multiple surfaces, doctors can confidently approve discharge or transition to rehabilitation.
This helps hospitals maintain efficient care pathways.
Conclusion
Real-World Mobility Is the True Measure of Prosthetic Success

Flat surfaces tell only a small piece of the story.
Real life challenges the user with stairs, slopes, broken roads, and unpredictable ground.
Functional outcome tests help clinicians understand whether the prosthesis supports safe, confident movement in these environments.
These tests guide training, socket design, alignment updates, and daily-life coaching.
They help prevent falls, improve independence, and build emotional confidence.
Above all, they help MDs and PTs create care plans that match the world the user truly lives in—not the perfect floor of a clinic.