Growing older brings many changes. When someone experiences limb loss later in life, it can feel overwhelming—both physically and emotionally. Simple tasks become harder. Muscles weaken. Confidence can slip. But there’s one gentle, science-backed way to rebuild strength and restore control: EMS.
EMS, or Electronic Muscle Stimulation, uses light electrical pulses to help activate muscles. For elderly amputees, it can be a safe and effective way to stay strong, reduce pain, and get ready for a prosthetic.
But like any tool, EMS needs to be used carefully—especially at home.
In this article, we’ll guide you step by step on how elderly amputees can safely use EMS at home. Whether you’re an older adult yourself, a caregiver, or a family member, you’ll learn how to set it up, when to use it, how to avoid risks, and how to get the most from every session.
Let’s begin with the basics.
Understanding EMS for Elderly Amputees
What Is EMS and How Does It Help?

EMS stands for Electronic Muscle Stimulation. It’s a method of gently activating muscles using small electrical pulses sent through the skin.
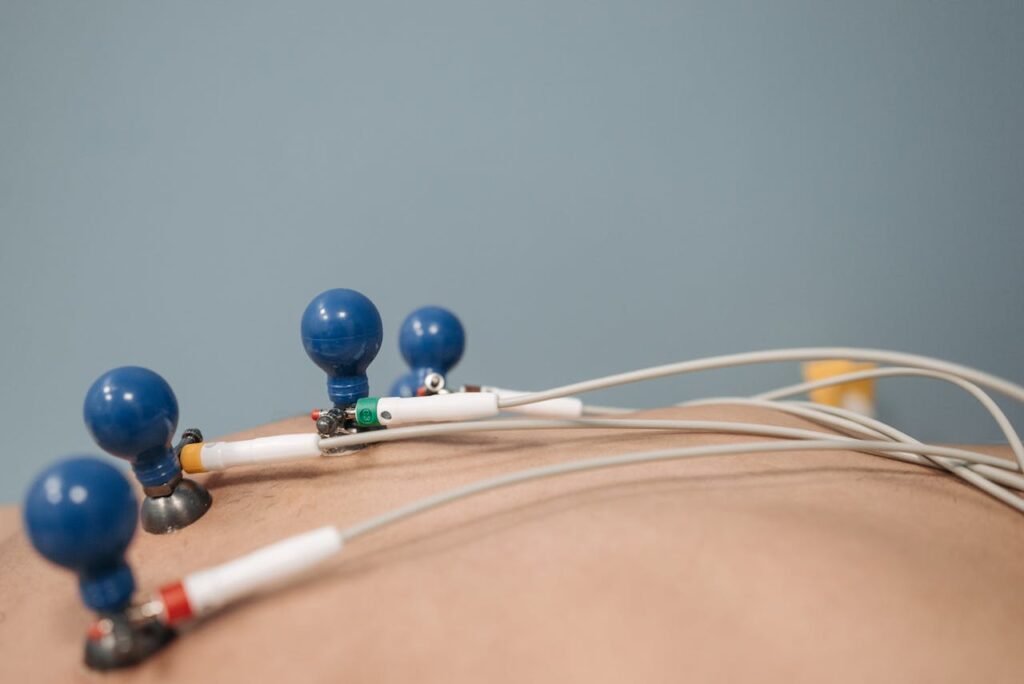
These pulses are delivered through sticky pads placed on the body. They make the muscle tighten and release, just like it would during natural movement.
For elderly people who have lost a limb, EMS can help keep the muscles around the stump strong and active. This is important because when muscles stay unused for too long, they become weaker.
With age, this happens even faster. That’s why EMS can play a big role in preventing muscle loss and improving blood flow in the residual limb.
Why Elderly Users Need a Gentle Approach
As we age, our skin becomes thinner. Muscles lose volume. Joints may become stiffer. The nervous system also becomes more sensitive.
Because of this, elderly users need a different approach to EMS. Settings must be lower. Sessions should be shorter. And placement must be done with great care.
When done properly, EMS is safe and comfortable. It can even feel relaxing, like a soft tapping or pulsing.
But the wrong settings—or rushed use—can lead to discomfort, skin irritation, or fatigue.
That’s why it’s so important to start slow, stay consistent, and adjust gently over time.
How EMS Helps With Daily Function
The goal of EMS isn’t just to build muscle—it’s to make daily life easier.
When muscles are stronger, it becomes easier to wear a prosthetic for longer hours. Getting in and out of bed, using the bathroom, or holding a spoon becomes less tiring.
EMS also helps reduce stiffness in the joints near the amputated limb. This makes movements smoother and more controlled.
With regular use, EMS supports better posture, reduces the risk of falls, and gives elderly users more independence in their daily routines.
Setting Up EMS at Home Safely
Choosing the Right Device
Not all EMS machines are the same. Some are designed for athletes. Others are made for hospital use.
For elderly amputees, it’s best to choose a device that is made for home rehabilitation. These devices often have simpler controls, gentle settings, and clear instructions.
BrawnBand, designed by Robobionics, is one such device. It’s light, easy to wear, and ideal for daily home use.
Always check that the device has adjustable intensity, preset programs, and safety certifications. This ensures you can tailor it to your comfort level.
Where to Place the Electrodes
Before placing the electrode pads, make sure the skin is clean and dry. Avoid areas with cuts, rashes, or scars that are still healing.
Electrodes should be placed over the muscle—not the bone, not directly over joints, and never on broken skin.
For a below-elbow amputee, pads are usually placed on the forearm muscles. For a below-knee amputee, the pads go on the upper calf or thigh.
If you’re unsure about placement, ask a physiotherapist to show you the correct spots during your first few sessions.
You can also take a picture of the setup to refer back to later.
Checking for Skin Safety
Older skin is more delicate. After each EMS session, check the area where the pads were placed.
Look for signs of redness, dryness, or irritation. If any discomfort lasts more than 30 minutes after the session, wait a day before using EMS again.
Apply a light, non-scented moisturizer once the skin is clean and dry. But never use lotion right before EMS—it can affect how the pads stick and how the current flows.
Replace the electrode pads every few weeks or sooner if they stop sticking well.
Comfort and skin health are more important than high settings or long sessions.
How to Begin EMS Therapy at Home
Start Slowly and Build Confidence

One of the biggest mistakes people make with EMS is trying to do too much, too soon. This is especially true for elderly users, whose muscles may not have been active for a while.
It’s important to start with very low intensity. On your EMS device, this is usually the lowest level where you can feel a light tingling or pulsing. It should not be painful or uncomfortable.
In the beginning, the goal is not to make the muscles move strongly. The goal is to wake them up gently. Even small contractions, or just a feeling of light tapping, are enough to begin.
The first few sessions should last no more than 10 to 15 minutes. This allows the body to adjust to the sensation without becoming tired or sore.
After a few days, once the user feels more comfortable, you can slowly increase the session time to 20 or 30 minutes—always under guidance from a physiotherapist or doctor.
If the user ever says the feeling is sharp, pinching, or burning, stop the session. That means the settings are too high or the pads are not placed properly.
Comfort is more important than speed. EMS is a journey—not a race.
Choosing the Best Time of Day
The right time for EMS is different for everyone, but it helps to pick a moment when the user is calm and not too tired.
Many elderly people feel stiff in the morning. A short EMS session after a warm bath or a gentle stretch can help loosen the muscles and make them feel more flexible.
Others may prefer using EMS in the afternoon, especially if they’ve had a busy morning and need to recharge their muscles.
Evening sessions are also common, as they can help relax the body before sleep.
No matter the time, try to create a quiet, peaceful environment. Turn off loud noise. Sit in a comfortable chair or lie down with a cushion for support.
Having a calm setting helps the user focus on the sensation and feel more in control of their therapy.
Use EMS as a Routine, Not a One-Time Treatment
Just like taking medicine or doing regular exercise, EMS works best when it becomes part of your daily routine.
Try to use it at the same time every day. This helps the body and mind get used to it, and makes it easier to keep the habit going.
You can create a small chart or notebook to track each session. Write down the date, time, settings used, and how the session felt.
This tracking is very useful—especially if you’re working with a doctor or therapist. They can look at your notes and guide you better on what to change or improve.
If the user ever feels too tired or unwell, it’s okay to skip a day. But try not to skip too many. The benefit of EMS comes from consistency over time, not from intensity.
Even short sessions done regularly will show better results than long sessions done once in a while.
Pair EMS With Gentle Activity for Better Results
While EMS is powerful on its own, it becomes even more helpful when used alongside light movement or stretching.
For example, after a session on the residual limb, you can encourage the user to do simple hand exercises if they have an upper-limb difference. This might include opening and closing the hand, wrist turns, or pretending to grip an object.
For a lower-limb difference, gentle seated leg lifts, ankle rolls, or hip movements can follow an EMS session.
These movements don’t have to be intense. They just help the brain and body work together, reinforcing the signals that EMS has activated.
If movement is not possible due to pain or weakness, even imagining the movement while EMS is running can be beneficial. This is called motor imagery, and it helps the brain rebuild its connection to the limb.
Tracking Results and Staying Comfortable
What Progress Really Looks Like

Many people expect EMS to show fast results, like stronger muscles or easier movement within days. But in elderly users, change often happens slowly and gently.
At first, progress might not be visible in the mirror. But there are still real signs that therapy is working.
You might notice that the limb feels warmer after a session. This is a good sign—blood flow is improving.
The user may say that their muscles feel more awake or lighter than before. They might sleep better, move more easily, or feel more confident wearing their prosthetic for longer.
Over weeks, you may begin to see clearer muscle tone or feel firmer tissue under the skin. You might notice better posture, balance, or energy during the day.
These are all important milestones.
Keep a notebook or calendar to write down what changes you observe. It could be a single line: “Felt more comfortable wearing prosthetic today” or “Lifted arm a little higher after EMS.”
These small wins, tracked over time, show that the therapy is working—even when it feels slow.
Adjusting Settings for Comfort and Effectiveness
The best EMS experience comes from using the settings that fit the person’s body—not from copying someone else’s routine.
As the body adjusts to EMS, it may become ready for slightly higher intensity. But don’t change it just because a certain number looks small. Change it only if the user says the current feels too light or the muscle isn’t responding anymore.
The same goes for session duration. If 15 minutes used to be enough, but the limb feels strong and not tired afterward, you might slowly increase to 20 or 25 minutes. But always ask how it feels during and after.
Pain is not a sign of progress. If the muscle contracts too hard, it can become sore, and the person might not want to continue.
It’s better to do gentle sessions that feel good than to force a strong session that causes discomfort.
You can also rotate where you place the electrodes slightly each week. This gives the skin time to rest and helps work different parts of the muscle.
When to Pause EMS or Ask for Help
Even when everything seems to be going well, there are moments when it’s best to take a break.
If the user has a fever, infection, or recent surgery, don’t use EMS until a doctor says it’s safe. EMS should never be used near open wounds, stitches, or heavily bruised areas.
If you notice redness that doesn’t fade after 30 minutes, or if the skin starts to peel, stop using EMS and let the skin heal. You can also try using a different brand of electrode pads, as some people react to the adhesive.
Other warning signs include:
- Sharp, electric-like pain during use
- Muscle twitching that doesn’t stop after the pulse ends
- Feeling dizzy, lightheaded, or very tired afterward
These signs mean something is off. Call your therapist or doctor and ask for help before continuing.
EMS should never be stressful or confusing. It’s a tool for healing—not a test of endurance.
Supporting Elderly Users as a Caregiver
Building Comfort and Trust

For many older adults, EMS might feel unfamiliar or even a little scary at first. The idea of using electricity on the body can bring up worries, especially for someone who is not used to machines.
This is where caregivers make a big difference.
Start by explaining EMS in simple words. You can say, “It’s just a gentle signal that tells your muscles to wake up.” Let them hold the pads. Show them how the machine works before turning it on.
During the first few sessions, stay close. Sit beside them. Hold their hand if needed. Watch their face for signs of discomfort or worry.
The more calm and patient you are, the more they’ll feel safe.
Sometimes, just knowing someone is there gives the confidence to try.
Making Therapy a Shared Activity
Instead of treating EMS like a medical chore, turn it into a daily ritual.
Play soft music. Read a short story aloud. Watch a favorite show together during the session. Let them sip warm tea while the machine runs.
These small touches turn therapy into something relaxing, even enjoyable.
And when EMS becomes something they look forward to, consistency follows naturally.
You can even use the same time each day, so it becomes a familiar part of their routine. For example, after breakfast, before a walk, or after evening prayers.
Familiarity builds trust—and trust brings better outcomes.
Helping With Setup and Cleanup
Many elderly users may struggle to place the electrodes themselves, especially if the amputation is in the upper limb. Their hands may be stiff, or they may have poor eyesight.
Help them apply the pads correctly. Make sure they’re flat, clean, and placed over the right muscles.
After each session, help remove them gently. Wipe the area with a clean, damp cloth. Let the skin breathe.
This kind of care doesn’t take long, but it makes the experience much easier and more comfortable for the user.
It also reduces the risk of skin irritation or misplaced pads—which can lead to poor results.
Long-Term Use of EMS and Life with a Prosthetic
Why Long-Term Use Still Matters

Some people think EMS is only needed right after surgery or during the first few weeks of rehab. But for elderly users, EMS often plays a bigger role after the early phase is over.
As the body continues to age, muscles naturally become weaker. Joints become less flexible. Nerve signals can slow down. Even the best prosthetic won’t work well if the muscles behind it are too weak to send proper signals.
That’s why continued EMS use—even just two to three times a week—can keep the muscles strong and the brain-muscle connection sharp.
Think of it like keeping the engine in your car running smoothly. Even if the car works today, a little maintenance now and then prevents problems later.
EMS and Prosthetic Use Go Hand in Hand
For elderly amputees who are fitted with a myoelectric prosthetic, EMS becomes even more important.
Myoelectric limbs, like the Grippy Bionic Hand, work by picking up signals from muscles near the stump. These signals control the movements of the prosthetic—like opening, closing, or gripping.
If the muscles are too weak or quiet, the prosthetic won’t respond correctly. It might feel slow or confusing to use.
By using EMS before putting on the prosthetic, you “wake up” the muscles. The signals become clearer. The limb becomes easier to control.
Some elderly users find that even 10 minutes of EMS in the morning helps them use their prosthetic more easily for the rest of the day.
It also reduces the time it takes to adjust to the device, especially for first-time users.
Preventing Fatigue and Improving Endurance
Wearing a prosthetic, especially for long hours, can be tiring. For older adults who may already feel low energy, this can become a reason to remove the device early—or stop using it altogether.
EMS helps solve that.
By building and maintaining muscle strength, EMS reduces fatigue. The prosthetic feels lighter. The body stays more balanced. Tasks like walking, cooking, or writing take less effort.
This builds confidence—and encourages longer use of the prosthetic, which improves both function and quality of life.
Adapting EMS Routines Over Time
As the user gets older or their routine changes, the EMS plan should also change. What worked last year might not be right today.
For example, if the user becomes more active and starts using their prosthetic daily, EMS might only be needed a few times a week to maintain strength.
But if their activity level drops—due to illness, travel, or changes in living arrangements—EMS might be used more often to prevent muscle loss.
This flexibility is one of the strengths of EMS. You can scale it up or down without major equipment or long clinic visits.
It gives the user control over their care in a way that feels manageable and safe.
The Role of Check-ins and Therapy Support
Even when using EMS at home, it’s a good idea to check in with a therapist every few months. These check-ins can be short and simple—just enough to see how the limb is doing, how the skin looks, and whether the current routine still fits the user’s needs.
Sometimes, a small change in pad placement or session time can lead to much better results.
These visits also give families and caregivers a chance to ask questions, share concerns, and learn new tips.
A good therapist understands the challenges of aging and limb loss. They’ll help you adjust EMS as the user’s body changes, ensuring safety and comfort at every stage.
A Future of Strength and Independence
Empowering Elderly Users With Safe, Simple Tools

At Robobionics, we believe that age should never be a barrier to strength or independence.
Elderly amputees face unique challenges—but with the right tools, they can overcome them.
EMS is one of those tools. It helps the body do what it already knows how to do—move, strengthen, and heal—just with a little extra support.
It’s safe. It’s simple. And with guidance, it’s something many elderly users can manage on their own.
Whether used to prepare for a prosthetic, maintain muscle tone, or ease daily discomfort, EMS becomes a trusted part of their routine.
And that trust brings freedom.
Reassurance for Families and Caregivers
If you’re supporting an elderly parent, grandparent, or loved one through their rehabilitation, you may feel unsure about how to help.
EMS gives you a way to be part of their care without needing special skills. You can help with setup, track progress, and offer comfort.
And as you see them gain confidence, move more freely, and smile at their own progress—you’ll know it was worth every effort.
Helping them feel strong again is a gift. EMS is simply the bridge that makes it easier to reach.
Ready to Begin the EMS Journey?
If you or your loved one is ready to explore EMS, we’re here to guide every step.
Schedule a free demo with us today at www.robobionics.in/bookdemo
We’ll help you choose the right settings, understand where to place the pads, and build a plan that works for your lifestyle.
Because recovery is not just about technology. It’s about people. And at Robobionics, we’re committed to helping people feel strong, independent, and cared for—at every age.