For someone recovering from limb loss, every step forward feels like a battle—and a breakthrough. One day it’s about reducing swelling. Another day it’s about getting your muscles to fire again. Then it’s about pain—phantom, nerve, or just from overusing the other side of your body.
If you’ve been navigating this journey, you’ve likely heard of two terms that sound similar but do very different things: EMS and TENS. Both involve electrical stimulation. Both use small devices with sticky pads on your skin. And both are often suggested during rehab.
But here’s where it gets confusing: when is EMS the right choice? When should you use TENS? Can you use both? And most importantly—what should you do, especially if you’re an amputee trying to recover strength, reduce pain, or prepare for a prosthesis?

Understanding EMS: What It Does and When Amputees Need It
What is EMS, Really?
EMS stands for Electrical Muscle Stimulation. It’s a therapy that uses tiny electrical impulses to make your muscles contract. Think of it as giving your muscles a small nudge to “wake up” and do the job they’re supposed to do—even if your brain isn’t quite ready to send the signal naturally yet.
That’s a big deal after amputation.
When a limb is removed, the muscles that used to control it don’t just stop being important. They’re still there, especially in cases of partial limb loss. But without regular use, they weaken fast. This weakening is called muscle atrophy, and it happens surprisingly quickly.
Sometimes, within just a week of non-use, your muscles start shrinking and losing strength. Once that happens, regaining mobility and preparing for a prosthesis becomes much harder.
That’s where EMS can help.
By using EMS early—under the guidance of your rehab team—you can keep those muscles active. Even if you can’t physically move them, EMS can keep them strong by simulating movement.
How Does EMS Work for Amputees?
Let’s say you’ve had a below-knee amputation. The muscles in your residual limb—like the hamstrings, quads, and calf muscles—used to control your foot and ankle.
Now, without that foot, your brain has fewer ways to send movement commands. That muscle group isn’t doing its usual job anymore, so it risks becoming weak or uncoordinated.
An EMS device sends gentle electrical pulses through pads placed on your skin. These pulses make your muscles contract in a pattern similar to what would happen during natural movement.
Over time, this keeps the muscles responsive, improves blood flow, and prevents stiffness or tightness that can interfere with prosthetic fitting.
What’s more, EMS can sometimes retrain your brain-muscle connection. After amputation, your brain needs to adjust to a new map of your body.
Using EMS may help reinforce those neural pathways, especially if combined with mirror therapy or visual feedback systems.
Why Strength Matters Before Prosthetic Use
A lot of people think the prosthetic limb does all the heavy lifting. It doesn’t. Your muscles are still very much in charge.
Think about walking. The socket of a prosthetic rests against your residual limb. If the muscles in that limb are weak or underused, wearing a prosthetic can feel like dragging weight around.
It can cause discomfort. It can lead to poor balance. It can even create wounds or pressure sores because your limb isn’t strong or coordinated enough to handle the load.
But if you’ve kept your muscles active with EMS, your residual limb becomes ready and resilient. It can bear weight, stabilize your body, and adapt to changes in movement. This shortens your overall rehabilitation time and improves your chances of returning to normal life activities.
When is EMS Most Useful?
The timing of EMS matters. Ideally, EMS should be started soon after surgery, once your wound is closed and your doctor gives the go-ahead. At this stage, EMS plays a preventive role—it keeps your muscles from weakening.
As healing progresses, EMS can be adjusted to help with muscle strengthening, especially for muscles that will support prosthetic use.
Later in recovery, EMS can support targeted training. For example, if you’re having trouble activating a certain muscle group—say, your hip abductors on the amputated side—EMS can help you isolate and engage those muscles better during physical therapy.
At each stage, the settings of the EMS device—like pulse width, frequency, and intensity—should be tailored to your needs.
That’s why working with a trained physiotherapist or rehabilitation specialist is key. They can make sure the stimulation is safe, effective, and aligned with your long-term goals.
What Does EMS Feel Like?
If you’ve never tried EMS before, you might imagine it feels shocking or painful. It doesn’t. Most people describe it as a tingling sensation that becomes a gentle tightening of the muscles. It’s not unpleasant—just unusual at first.
You remain in control. The intensity can be adjusted so that it stays comfortable. A good session might leave your muscles feeling like they’ve just had a light workout.
Some amputees even find it satisfying, especially once they get used to the rhythm of contraction and relaxation.
Over time, it becomes part of your routine. Some people use it while sitting and watching TV, reading, or doing upper-body exercises. Others integrate it directly into their physical therapy sessions.
Other Benefits EMS Brings to the Table
EMS isn’t just about strength. It offers a few hidden perks that can make a real difference in recovery:
- Improved circulation: By triggering muscle contractions, EMS helps move blood through your tissues. This supports healing, reduces swelling, and prevents fluid buildup.
- Better skin condition: Good circulation also keeps your skin healthier—critical when you’ll eventually wear a prosthetic socket that presses against your residual limb daily.
- Pain relief: While EMS is not primarily for pain relief, some amputees report feeling less residual limb discomfort after regular sessions. This is possibly due to muscle relaxation and improved local blood flow.
- Quicker prosthesis training: Therapists often find that amputees who use EMS adapt more quickly to prosthetics. Their bodies are more responsive, their posture improves faster, and they experience fewer setbacks during gait training.
Are There Any Risks or Things to Watch Out For?
EMS is generally safe, but like any medical tool, it needs to be used wisely.
Avoid using EMS over open wounds, infected skin, or near surgical staples or sutures. If you have a heart condition, pacemaker, or epilepsy, you should speak to your doctor first.
Always follow the placement guidelines provided by your rehab team—incorrect pad placement can reduce effectiveness or even cause discomfort.
It’s also worth mentioning that EMS is not a replacement for physical therapy. It’s a partner. The best outcomes happen when EMS is part of a bigger plan that includes stretching, strength training, balance work, and eventually gait training with your prosthesis.

TENS Therapy: Managing Pain and Discomfort After Amputation
What is TENS and How is it Different from EMS?
TENS stands for Transcutaneous Electrical Nerve Stimulation. Like EMS, it uses electrical impulses delivered through pads on your skin. But the goal isn’t to make muscles move—it’s to help manage pain.
This is where a lot of confusion happens. People often mix up EMS and TENS because the devices look similar. But while EMS focuses on muscles, TENS focuses on nerves.
For amputees, pain after surgery isn’t just expected—it’s complex. You might feel pain from the surgical wound, pressure from swelling, or a deep ache in the bones and tissues that remain.
But there’s also something more puzzling: phantom limb pain. That strange, stubborn pain you feel in a part of your body that’s no longer there.
TENS doesn’t “cure” pain, but for many amputees, it becomes a powerful tool to help control and reduce it—especially when medications either don’t work well enough or cause side effects like drowsiness or nausea.
How TENS Works for Amputees in Pain
Your nervous system is constantly sending signals to and from your brain. When something hurts—like an injury—your nerves fire signals up to your brain saying, “Pain here!” TENS works by blocking or scrambling some of those pain signals.
By applying low-voltage electrical pulses around the area of pain, TENS can “distract” your brain and interrupt the pain message before it reaches full intensity. It may also encourage the body to release endorphins, which are natural painkillers.
You don’t have to understand all the science behind it to benefit. What matters is this: TENS doesn’t fix the cause of the pain, but it can help reduce how much it affects you. That can mean fewer painkillers, better sleep, and a clearer head for doing physical therapy.
Where and When Can You Use TENS?
TENS can be used almost anywhere on the body, but when it comes to amputation recovery, the placement of the electrodes is important. You don’t place them directly on the residual limb unless your doctor says it’s safe.
Instead, the pads are usually placed around the painful area, or even at the spine level, depending on how the pain travels through your nerves.
If you have phantom limb pain, your therapist might experiment with different placements to find what works best. Some studies suggest that applying TENS near the nerve root—where the nerves that used to serve your missing limb connect to the spine—can be especially effective.
TENS can also help with residual limb pain, which comes from the part of the body that’s still there but healing. It’s especially helpful when swelling puts pressure on nerves or when tight muscles start cramping.
In many cases, TENS is used during the early recovery period, when pain is high but movement is limited. But it’s also useful later, especially during prosthetic training, when your body is adjusting to new types of pressure and weight distribution.
What Does TENS Feel Like?
TENS doesn’t cause your muscles to move. It doesn’t contract your limb like EMS does. Instead, it creates a tingling or buzzing sensation on the skin.
Some people say it feels like ants crawling. Others say it’s like a massage or vibration. Once your skin adjusts, it becomes almost soothing.
You control the intensity. A good session should never hurt. The goal is comfort—not to push through discomfort. Most TENS units let you change the pulse rate and intensity so you can find the sweet spot that works for your body.
Sessions usually last between 15 to 30 minutes, and you can use TENS multiple times a day if needed. Many amputees keep a unit at home and use it as part of their daily pain management routine.
Why Amputees Choose TENS Therapy
Pain affects everything: your mood, your energy, your sleep, your willingness to do rehab. Even when pain doesn’t stop you from doing something, it can make everything harder.
TENS helps in ways that go beyond just pain scores. Many of our clients tell us:
- “TENS gives me control over my pain, which helps my mental health.”
- “It’s the only thing that touches my phantom pain at night.”
- “I can finally sleep again without needing extra pills.”
- “My residual limb felt too sensitive to touch. TENS helped desensitize it.”
There’s no one-size-fits-all answer for pain. But having another tool in your pocket—one that doesn’t involve medicine—can be incredibly empowering.
And in India, where access to regular pain specialists may be limited, especially in smaller towns or rural areas, TENS provides an accessible, low-cost way to manage pain at home.
TENS vs. Pain Medications
Let’s be clear: TENS doesn’t replace medical pain relief. But it can reduce your dependence on it.
Pain medications, especially opioids, come with risks—drowsiness, constipation, addiction. Even over-the-counter painkillers like paracetamol or ibuprofen can cause issues if taken for too long. That’s why doctors and physiotherapists often recommend a combination of approaches.
TENS is safe for long-term use, doesn’t build tolerance, and has very few side effects. The worst most people experience is mild skin irritation from the pads, which can usually be fixed by adjusting placement or switching to hypoallergenic gel pads.
When used alongside medication, ice, heat therapy, massage, or movement, TENS becomes part of a balanced pain management plan.
Can TENS Help with Phantom Limb Pain?
This is one of the biggest questions amputees ask. And while the answer is different for everyone, the short version is: Yes, it can.
Phantom limb pain is complex. It’s not just in your mind—it’s real pain, caused by mixed signals in the nervous system. Since TENS interacts with your nerves and influences how pain messages travel, it can sometimes “reset” the system a bit.
We’ve seen people who couldn’t sleep because of sharp phantom pain try TENS and finally get a full night’s rest. Others use it before their physical therapy sessions to reduce the discomfort that comes from moving their residual limb.
Some research even suggests that using TENS regularly in the early stages of recovery might reduce the chances of chronic phantom pain forming at all. While more studies are still needed, it’s an encouraging thought—and another reason to explore TENS early in your journey.

Choosing Between EMS and TENS: What’s Right for Your Stage of Recovery
Understanding Timing and Purpose
One of the most common questions amputees ask us at Robobionics is whether they should be using EMS or TENS—or both. The answer depends on where you are in your recovery journey and what your body needs most at that time.
These two therapies serve very different purposes. EMS helps your muscles stay strong and engaged, while TENS helps you manage pain. You don’t have to choose one over the other for life. Instead, it’s about matching the tool to the moment.
In the early stages of recovery, usually right after surgery, your body is adjusting to the trauma of amputation. Pain levels are often high, and your mobility is limited.
This is where TENS tends to shine. Its main job is to calm the nervous system and offer some relief without putting any extra stress on your healing tissues.
If your doctor clears it, you may begin using TENS even before you’re able to walk or move much. It provides comfort when you’re most vulnerable, helping you get rest, eat properly, and stay mentally strong—all of which are essential for healing.
Once your wound has healed and swelling begins to reduce, your rehab team might introduce EMS. At this point, you’re no longer just surviving—you’re starting to rebuild. Your body needs to re-learn how to activate muscles, especially those around the residual limb.
EMS can now support this phase by mimicking natural muscle contractions. It keeps your muscles from shrinking and helps re-establish neuromuscular connections that may have gone dormant after surgery.
If you begin EMS early enough, your muscles may remain toned and prepared for the physical demands of prosthetic use.
Combining EMS and TENS Strategically
Some people imagine that EMS and TENS can’t be used together, but that’s not the case. In fact, they can complement each other beautifully if used with care and expert supervision.
For example, you might use TENS in the morning to take the edge off your phantom pain, giving you a better mental state to handle the day. Later in the afternoon, once you’re feeling more relaxed, you could switch to EMS for muscle conditioning exercises during your physical therapy session.
It’s not uncommon for therapists to alternate between the two during a single appointment. They might begin with TENS to reduce residual limb sensitivity, then shift to EMS to stimulate deeper muscle groups.
This combined approach doesn’t just relieve discomfort—it helps prepare your body for more advanced tasks like standing, walking, and balancing.
But while this sounds ideal, it’s important to remember that not everyone responds the same way. Some amputees find EMS uncomfortable in the beginning, especially if the residual limb is still tender. Others find that their pain isn’t significantly reduced with TENS alone.
That’s why the guidance of a physiotherapist or rehabilitation specialist is essential. They can help tailor the intensity, duration, and placement of both therapies to suit your specific condition and goals.
Making the Right Choice Based on Your Needs
Let’s say you’re three weeks post-op. Your pain is still fairly high, and you haven’t started much movement training yet. At this stage, TENS is likely the better choice.
It helps manage your discomfort, supports better sleep, and makes it easier to sit, shift, and begin light stretches. Trying to use EMS too early might cause unnecessary strain on healing tissues and discourage you from continuing therapy.
Now, fast forward a few more weeks. Your wound has healed. You’re starting to sit upright more, perhaps even practicing standing or gentle weight-bearing. This is the perfect moment to introduce EMS. Your body is now capable of tolerating light muscle activation.
You may even notice that areas of your residual limb feel “asleep.” EMS can help wake up those muscle groups and restore your sense of control over them.
In the months that follow, the focus of therapy often shifts. You’re now thinking about prosthetic readiness. Can your limb tolerate pressure? Are your muscles responsive enough to support a socket? Are you able to balance, step, and recover from minor slips?
At this stage, EMS becomes more prominent, while TENS may take a backseat—unless your pain flares up again due to overuse or prosthetic adjustments.
Even during later stages of recovery, it’s smart to keep a TENS unit handy. Adjusting to a new prosthesis often causes temporary muscle soreness, nerve irritation, or phantom sensations.
Instead of reaching straight for more medication, many of our clients find that TENS provides fast and calming relief. It’s also useful on days when you’re not doing much physical activity but still need to address low-level, lingering discomfort.
What About Emotional and Mental Considerations?
One thing people don’t talk about enough is how pain and muscle loss affect your emotional state. Chronic pain drains your energy and makes even small tasks feel overwhelming.
On the other hand, muscle atrophy and weakness can make you feel helpless or disconnected from your body. Choosing the right therapy can help you rebuild not just your physical capacity but your confidence.
When you use TENS and finally feel relief after a day of struggling, you feel more in control. You can eat better, rest better, and engage more in your rehab.
And when you use EMS and see your muscles working again—even just twitching for the first time in weeks—you get this spark of hope. It reminds you that your body is still capable of healing and rebuilding. These emotional wins add up. They keep you going.
That’s why the decision between EMS and TENS isn’t just clinical. It’s deeply personal. It’s about what your body needs, yes—but it’s also about what gives you peace of mind, what restores your energy, and what helps you feel strong enough to keep moving forward.
Tailoring Your Recovery Plan Over Time
Your recovery won’t follow a straight line. Some days your pain might flare up unexpectedly. Other days you might feel strong enough to try walking for longer stretches. Your therapy plan, including how you use EMS and TENS, should evolve with your changing needs.
There may be weeks when EMS is your main focus, helping you build strength for gait training or prepare for a socket fitting. Then, if you overdo it, you may rely more on TENS for a while to ease discomfort and inflammation.
These shifts are normal. They show that you’re listening to your body and responding with care.
At Robobionics, we encourage all our clients to check in regularly with their therapists. As your body changes, your therapy strategy should too. What worked a month ago might not be the best fit today. That’s not a failure—it’s progress.
How to Use EMS and TENS Safely: Practical Advice for Amputees at Home
Why Safety and Setup Matter More Than You Think
Whether you’re using EMS to activate muscles or TENS to calm nerve pain, these tools only work well when used correctly. That doesn’t just mean pressing the “on” button.
It means understanding how your body reacts, knowing where to place the electrodes, adjusting settings mindfully, and avoiding common mistakes that could reduce the therapy’s effectiveness—or worse, slow down your recovery.
At Robobionics, we’ve seen that amputees who learn how to use these devices safely from the start often make faster progress. They feel more confident. They avoid unnecessary setbacks.
And they build a rhythm that fits smoothly into their everyday life. So let’s break down the most important parts of using EMS and TENS at home—without the jargon, without the guesswork.
Start With Guidance, Then Build Independence
No matter how eager you are to start therapy on your own, your first few sessions should always be guided by a rehabilitation expert or physiotherapist. Even if you’ve used EMS or TENS in the past, your post-amputation body is different now.
The nerve paths are altered. Your muscle groups are under different levels of strain. And your skin may be more sensitive or reactive than before.
Your therapist will help you understand how to safely place the electrodes based on your unique anatomy. They’ll also guide you on ideal pulse settings—things like frequency, duration, and intensity.
These numbers may sound technical, but with a few sessions of hands-on practice, they become easy to understand. Think of this as training your brain and body to use a powerful tool the right way.
Once you’ve been shown how to do it safely, you can begin building your own routine at home. Many amputees we work with set aside specific times of the day for EMS or TENS.
For example, some use TENS before bedtime to reduce phantom pain, while others schedule EMS after a morning walk to support muscle recovery. Whatever schedule you choose, what matters most is consistency and mindfulness.
Choosing the Right Areas for Electrode Placement
This is where many people get tripped up. Placing the pads too far from the target area, too close to the surgical scar, or over bony areas can reduce the effect—or even cause discomfort. With EMS, the goal is to trigger muscle contractions.
That means placing the electrodes over muscle bellies, not tendons or joints. For amputees, these muscles are usually located around the residual limb, but placement varies depending on whether you’ve had a below-knee, above-knee, below-elbow, or above-elbow amputation.
TENS, on the other hand, is more flexible. Since its focus is on nerves, you can place the electrodes near the source of pain, or even along the path of the nerve that used to serve your missing limb.
Some amputees get better results when placing the pads on the spine or lower back—especially for phantom limb pain.
One key thing to remember is to avoid open wounds, inflamed skin, or recent surgical stitches. Never place electrodes directly on these areas, as it can interfere with healing or cause irritation. Also, make sure your skin is clean and dry before applying the pads. Oils or lotions can affect how the current flows and may cause the pads to slip.
If you ever feel sharp, burning pain under the pads—or if your skin becomes red and itchy afterward—that’s a sign something isn’t right. Either the pads are in the wrong place, or the intensity is too high.
Stop and reassess. Don’t try to “push through” it. Pain isn’t a sign that it’s working harder—it’s a sign that something needs adjusting.
Finding the Right Intensity and Settings
One of the most common mistakes we see is people turning up the device too quickly. With EMS, it might feel like more intensity equals more muscle gain. With TENS, some people assume stronger stimulation will block more pain. But that’s not how these systems work.
For EMS, your goal is to stimulate the muscle without causing fatigue or cramping. Start at the lowest setting that causes a visible contraction and gradually increase until the contraction feels firm but not painful.
If your limb twitches too hard or becomes sore after a session, you’re likely using too much intensity. You’re not training for a marathon—you’re training your body to respond, rebuild, and reset.
For TENS, you want to find the level that provides relief without discomfort. The sensation should feel like tingling or soft pulsing—not stabbing, shaking, or stinging. If you can’t feel it at all, turn it up slightly.
If it distracts you or feels annoying, turn it down. The best setting is often somewhere in the middle, where your brain registers the sensation but doesn’t fixate on it.
Every body reacts differently, and your tolerance may change over time. Some days you’ll need more intensity, other days less. That’s okay. Pay attention to how you feel during and after each session. Keep a simple notebook if needed—just jotting down what settings worked best and how you felt afterward can help you track your progress.
Creating a Sustainable Routine
Using EMS or TENS once or twice won’t transform your recovery. The results come from steady, repeatable habits. That doesn’t mean hours of daily therapy. Most sessions last between 20 to 30 minutes. What matters is that you do them regularly, in a way that fits into your life.
Start small. If you’re just beginning, two or three sessions a week might be enough. As you grow more confident, you can increase frequency based on your goals. For muscle training with EMS, most people benefit from 3 to 5 sessions per week. For pain relief with TENS, some people use it daily, especially during flare-ups.
The key is to make it part of your day, not a disruption. Maybe you use TENS while reading the newspaper or listening to music. Maybe you schedule EMS right after your home exercises. Whatever rhythm you find, the point is to build consistency—not perfection.
Understanding When to Pause or Seek Help
Even though these therapies are generally safe, there are times when it’s better to pause and speak with a professional. If your residual limb becomes swollen, red, or painful during or after sessions, stop and consult your physiotherapist. If your phantom limb pain suddenly becomes more intense after using TENS, it may be time to adjust placement or settings.
Some medical conditions require extra care. If you have a pacemaker, heart arrhythmia, epilepsy, or severe diabetes-related nerve damage, always get medical clearance before using EMS or TENS. And never use these devices near the chest, head, or over the carotid artery without supervision.
It’s also smart to schedule regular check-ins with your rehab team—even after you feel confident. As your body changes, your device settings and therapy focus might need to shift. New muscle growth, prosthetic alignment changes, or surgical revisions can all affect how your body responds to stimulation.
Owning Your Recovery Journey
One of the most empowering things about EMS and TENS is that they give you a sense of control. After an amputation, it’s easy to feel like everything is being done to you—by doctors, therapists, prosthetists. But these devices give you the tools to do something for yourself, every day.
They remind you that healing isn’t passive. It’s active. It’s built on small, consistent choices. When used wisely, EMS and TENS become more than just medical devices.
They become part of your new normal—a way to listen to your body, respond to its needs, and take one more step forward, on your terms.

Mind-Muscle Connection After Amputation: How EMS and TENS Help You Rebuild Body Awareness
Losing a Limb Changes More Than Just Movement
When someone loses a limb, it’s not just the body that undergoes a change—it’s the brain too. The area in the brain that once controlled that limb doesn’t just disappear. It lingers, often confused, searching for signals that are no longer there.
This is one of the reasons why amputees often experience phantom sensations, and why some feel disconnected from the rest of their body, even long after healing has begun.
But here’s something we’ve learned through years of supporting amputees at Robobionics: your brain can relearn, remap, and reconnect—especially when you combine movement with focused intention.
This is where EMS and TENS, when used properly, go beyond just muscle stimulation or pain relief. They become tools for rebuilding your mind-body awareness.
Why Body Awareness Matters in Rehabilitation
Body awareness—or proprioception—is the sense of where your body is in space. It’s what allows you to walk without looking at your feet or reach for something without staring at your arm. When you lose a limb, that sense of awareness is disrupted. Your brain’s internal map of your body becomes incomplete or outdated.
Rebuilding that map is essential—not just for learning how to use a prosthetic, but for regaining balance, coordination, and trust in your body. The more accurate this mental map becomes, the better your chances of walking confidently, adapting to different surfaces, and performing daily tasks without fear of falling or straining.
But this remapping doesn’t happen on its own. It requires repeated stimulation—both physical and neurological. That’s where EMS and TENS can help, in ways most people don’t even realize.
How EMS Supports Neurological Remapping
When EMS triggers a muscle to contract, your brain doesn’t just observe passively. It receives feedback—electrical, physical, and sensory. That feedback tells your nervous system, “This muscle is alive. It’s working. It’s part of me.”
Now, imagine pairing that feedback with intention. Instead of just letting the machine stimulate your limb, you actively focus on the movement, even visualizing it as you would during a workout.
For example, during a session targeting your hamstring, you close your eyes and think about curling your leg. As the EMS kicks in, your brain connects the mental command with the physical response. This builds a bridge between intention and sensation.
Over time, that bridge grows stronger. You start to regain control—not just mechanically, but mentally. Therapists sometimes refer to this as building the mind-muscle connection, and for amputees, it can make a huge difference.
We’ve seen clients who were struggling with balance suddenly feel more stable, simply because their brain was better attuned to their residual limb.
This isn’t magic—it’s neuroplasticity, the brain’s ability to form new pathways. And EMS, especially when used thoughtfully, acts as a spark that helps fire up those new paths.
How TENS Can Calm the Nervous System and Restore Focus
TENS, while different in function, also plays a role in mind-body reconnection. When you’re in pain, your brain shifts into protection mode. It avoids certain movements.
It tenses muscles. It becomes overly focused on discomfort rather than coordination. This leads to poor posture, stiffness, and even fear of movement.
By calming nerve signals and reducing pain, TENS allows your brain to relax and shift its focus back to movement quality and awareness. In other words, when you’re not overwhelmed by pain, you can pay attention to how your body feels and moves.
Many of our clients tell us that after a TENS session, they’re able to stand longer, walk with better posture, or engage more confidently in physical therapy. It’s not that the TENS changed their body structure—it changed the brain’s ability to engage with the body without the noise of pain.
This is especially helpful when dealing with phantom limb pain. The more phantom pain you feel, the more your brain clings to the idea of the “missing” limb. But when you introduce soothing sensations through TENS—particularly in the surrounding areas—the brain begins to recalibrate.
It updates its internal map. Over time, this may reduce phantom sensations and improve your sense of integration with the rest of your body.
Integrating Mental Focus Into Your Sessions
So how do you make the most of this mind-body connection? It starts with intention. Before starting your EMS or TENS session, take a minute to ground yourself. Sit comfortably. Breathe deeply. Visualize the area you’re about to stimulate. If it’s your residual thigh, picture the muscle. If it’s your lower back, feel its weight against the chair.
During EMS, try to mentally engage the muscle before it contracts. Say to yourself, “Now I’m moving this muscle,” even if the machine is doing the work. That mental rehearsal reinforces the signal pathways and makes the stimulation more effective over time.
During TENS, especially for pain relief, use the moment to relax your nervous system. Don’t multitask. Focus on your breath. Think of the tingling sensation as washing away discomfort. This calm state helps your brain register the session as healing, not just distracting.
These are small changes, but they matter. We’ve found that amputees who approach EMS and TENS with this kind of focused attention often experience faster and deeper improvements—not just in movement, but in how connected they feel to their bodies again.
Healing Isn’t Just Physical—It’s Neurological and Emotional Too
After amputation, people often focus on the visible signs of recovery: reduced swelling, stronger muscles, better balance. But what’s happening inside the nervous system is just as important.
When EMS and TENS are used with awareness, they support not just tissue healing but neural healing. They help rebuild confidence, rewire movement pathways, and calm the chaos that often follows surgery and trauma.
You’re not just reconditioning a limb. You’re reclaiming your sense of self.
And that—more than any device, therapy, or medication—is what true recovery is all about.

The Future of EMS and TENS in Amputee Care: What’s Next?
Beyond Devices: The Next Chapter in Neuromuscular Recovery
Electrical stimulation therapy has come a long way. What started as basic machines sending jolts to nerves and muscles has now evolved into intelligent, user-friendly systems that are reshaping how amputees recover.
But this is just the beginning. At Robobionics, we constantly keep our eyes on the horizon—because tomorrow’s care isn’t just about replacing what was lost, it’s about enhancing what remains.
The future of EMS (Electrical Muscle Stimulation) and TENS (Transcutaneous Electrical Nerve Stimulation) lies not just in stronger devices or longer battery lives, but in smarter, more personalized, and neuro-integrated systems that adapt to the individual, not the other way around. And for amputees, this shift could completely redefine the pace, comfort, and effectiveness of recovery.
Smarter Devices That Learn With You
One of the most exciting developments in EMS and TENS therapy is the rise of AI-powered stimulation units. These are not just devices that deliver fixed pulses at set intervals. They learn from your body’s response. They track how your muscles contract, how quickly you fatigue, and even how your skin conductivity changes with sweat or stress.
Soon, your EMS device may come with adaptive programs that shift stimulation patterns based on real-time data. If your muscles are more fatigued than usual, the session might scale down intensity automatically.
If your nerve sensitivity is high, the device could adjust pulse widths to maintain comfort while still being effective. You won’t have to guess or rely entirely on trial-and-error. The device itself will help fine-tune the session, creating a smarter therapy loop.
For TENS, this might mean more intuitive pain management. Imagine a unit that learns which pulse frequencies reduce your phantom pain most effectively and prioritizes those settings in future sessions. This level of responsiveness could reduce overuse, lower skin irritation, and help you get better results in less time.
Wearable Integration and Remote Monitoring
Another key innovation is the integration of EMS and TENS into wearable platforms. These are sleek, flexible, fabric-like systems that wrap around your limb—no more fiddly gel pads or tangled wires.
They can be worn under clothes, making therapy easier to do while working, walking, or even relaxing. They offer discreet, continuous stimulation, programmed to deliver gentle pulses throughout the day in intervals based on your needs.
But what makes these wearables even more promising is how they can connect wirelessly to your phone or a therapist’s dashboard. That’s right—rehabilitation is becoming remote-friendly.
With secure health data syncing, your physio can monitor how often you’re using EMS or TENS, see how your muscles are responding, and even adjust settings remotely. This is a game changer, especially for amputees in rural or underserved areas, where access to specialist clinics may be limited.
This technology gives you independence without sacrificing support. You don’t have to wait for your next appointment to tweak your program. Adjustments can happen in real-time, guided by professionals who can see your progress from afar. It makes recovery more flexible, faster, and data-driven.
Combining EMS with Brain-Computer Interfaces
Perhaps the most futuristic—and incredibly promising—area of development is the combination of EMS with brain-computer interfaces (BCIs).
These systems read brain activity and translate your intention to move into action via electrical stimulation. In simple terms, you think about moving a muscle, and the EMS device contracts it accordingly.
This kind of integration is already being tested in stroke recovery, but it holds massive potential for amputees too.
For someone with partial limb loss, this technology could bridge the gap between the brain and residual muscles, helping re-establish natural movement patterns. It’s like putting the brain directly back in charge, with EMS acting as the messenger.
When combined with advanced prosthetics—especially bionic limbs—this level of control could bring a sense of natural movement and feedback that’s never been possible before. You’d no longer feel like the machine is separate from you. Instead, it becomes an extension of your intention, your strength, and your awareness.
EMS as a Gateway to Myoelectric Control
In the world of bionic limbs, myoelectric control is the gold standard. It uses electrical signals from your muscles to control a robotic prosthesis. But here’s the catch: not all amputees have strong enough residual signals to make this work—especially if their muscles were inactive for too long after surgery.
That’s where EMS becomes more than just a therapy—it becomes a training ground. By regularly stimulating and activating the target muscle groups, EMS can help “wake up” those signals, making them readable by myoelectric sensors.
This means more amputees will be eligible for high-tech prosthetic control systems. It also means faster adaptation, better grip precision, and fewer frustrations during training.
We’ve already started incorporating this into our approach at Robobionics. By using EMS during the early stages of recovery, we prepare the muscles for eventual myoelectric training. This proactive method has shown promising results—not only in signal strength but also in user confidence.
Greater Personalization Through Data and Feedback
The future isn’t just about more advanced machines—it’s about more personalized rehabilitation. Soon, your EMS or TENS device might collect detailed data not just on your sessions, but on your gait, your sleep, your heart rate, and even your mood. This data, analyzed together, can reveal deeper insights into what helps you recover faster.
You might get notifications like: “Your pain scores are lower when you do EMS sessions after walking,” or “Try reducing stimulation frequency on days when your sleep is disrupted.” It’s no longer guesswork—it’s a continuous loop of observation, adjustment, and improvement.
This kind of real-time feedback empowers amputees to become active partners in their recovery, not just passive recipients. And the more informed you are, the more in control you feel.
Affordability and Access: Bringing the Future to Everyone
All of this sounds exciting—but it also raises a big question: will these advanced systems be available to everyone? Or will they remain out of reach for most amputees, especially in a country like India where rehabilitation resources vary widely?
At Robobionics, we believe technology must be inclusive. We’re already working with partners and developers to design low-cost, mobile-connected EMS and TENS systems that can deliver many of these features without massive price tags.
We envision a future where a farmer in rural Bihar has the same access to smart therapy tools as someone recovering in a top hospital in Delhi.
This isn’t just a dream. With government support, public-private partnerships, and innovations in local manufacturing, smart rehab is becoming scalable. A
nd when combined with tele-rehab platforms, even the most remote corners of India can be connected to world-class prosthetic care.
A Future Built on Action, Intention, and Belief
Electrical stimulation therapy is no longer just a niche tool in the rehab toolkit. It’s becoming a foundation for how amputees can regain strength, reduce pain, and reclaim control. But as it grows more advanced, it’s important not to forget the heart of it all: your intention.
The future belongs to those who show up daily. Who strap on the electrodes even when they’re tired. Who visualize movement even when it feels distant. Who believe that every pulse, every contraction, every moment of relief is one small step closer to a life that feels whole again.
And we, at Robobionics, are walking that path with you—one signal at a time.
Conclusion
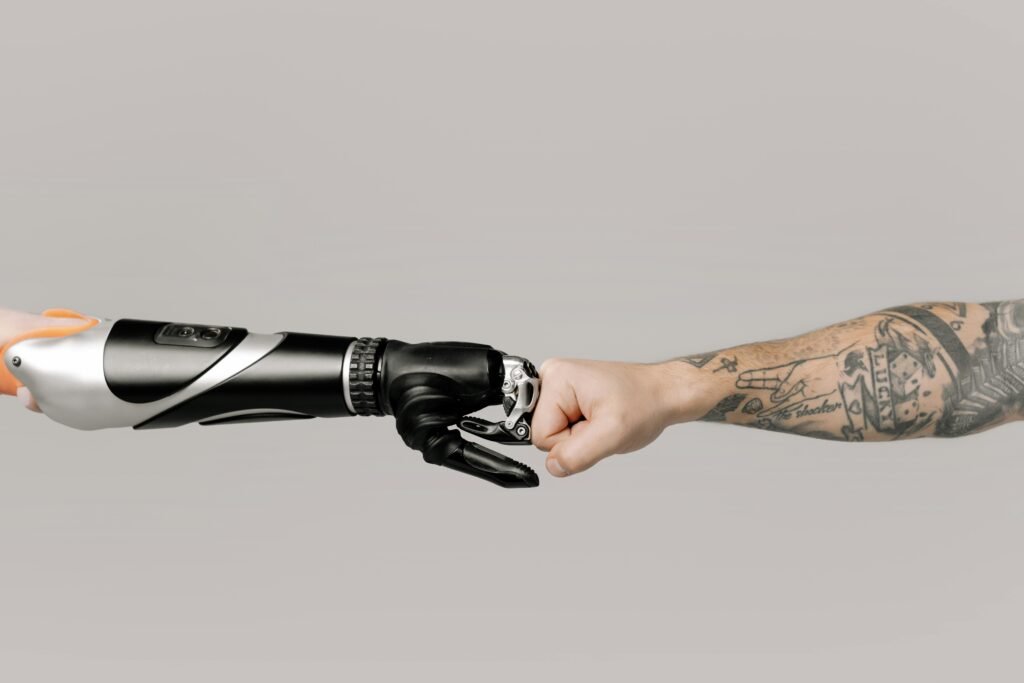
Recovery after limb loss isn’t just about healing wounds or fitting a prosthetic—it’s about rebuilding strength, easing pain, and reconnecting with your body. EMS and TENS offer two powerful ways to support that process. EMS helps your muscles stay active and ready, while TENS provides relief from pain that can slow your progress. Used together, with intention and care, they can transform your recovery journey.
As technology evolves, these tools are becoming smarter, more accessible, and more personalized than ever before. But their real power lies in how you use them—with patience, purpose, and a deep belief in your body’s ability to adapt and grow.
At Robobionics, we’re not just building prosthetics—we’re building paths to possibility. And we believe every pulse, every contraction, and every moment of relief is a step toward a stronger, more confident you.
Your recovery is yours to shape. And with EMS and TENS by your side, you’re never alone on that path.



