Every person’s journey with limb loss is different. So is their road to recovery. At RoboBionics, we understand this deeply. That’s why when it comes to using Electrical Muscle Stimulation (EMS), one size doesn’t fit all.
Whether someone has lost part of their arm below the elbow, above it, or even just a finger—how their muscles work, heal, and respond to therapy is unique. EMS can do wonders when used right. It helps wake up muscles, build strength, and even reduce pain. But to really work, it has to be customized to the person’s specific needs.
In this article, we’re going to walk you through how to tailor EMS therapy based on the level of amputation. We’ll cover everything from the science behind it to how to set up a session that’s just right for each individual. This guide is packed with practical tips and clear steps. No confusing terms. No fluff. Just real help for real people.
Let’s dive in.
Understanding EMS and Its Role in Recovery
What is EMS?
Electrical Muscle Stimulation, or EMS, uses small electrical pulses to make muscles contract. It’s not new, but in prosthetic rehab, it’s a game-changer.
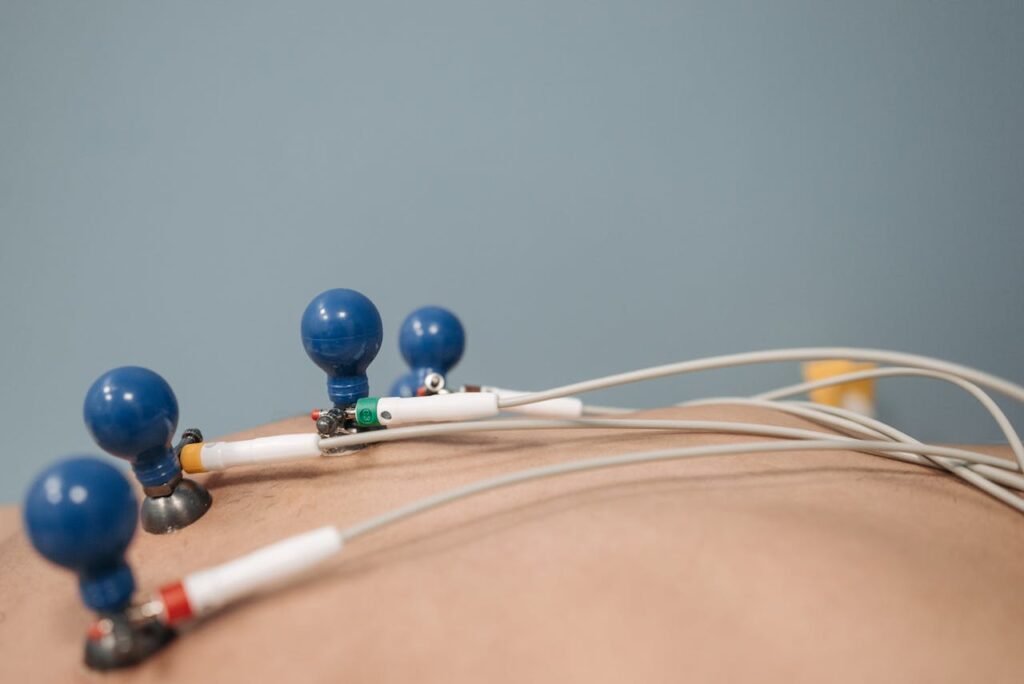
These signals are sent through pads placed on the skin. They trigger the muscles underneath to move, even if the person can’t move them on their own yet.
This helps the brain and body “remember” how to use those muscles. Over time, it strengthens the muscles and improves control.
Why EMS Matters After Amputation
After an amputation, the body doesn’t just lose a limb. It also loses muscle use, blood flow, and nerve activity in that area. Muscles that aren’t used can weaken quickly.
EMS helps keep these muscles active. This is key, especially when a person is preparing to use a myoelectric prosthesis, like the Grippy™ Bionic Hand. These devices rely on signals from the muscles to work properly.
EMS can also reduce phantom limb pain. Many people feel pain in the limb that’s no longer there. Regular stimulation helps calm those nerves.
The Need for Customization
Not everyone has the same type of amputation. Some people lose their hand, others the whole forearm, and some lose fingers or parts of fingers.
So why should everyone get the same EMS session?
They shouldn’t. The level of amputation changes which muscles are available. It affects where the electrodes should go, how strong the pulses need to be, and what goals the therapy should focus on.
That’s why customization is so important.
Customizing EMS for Finger-Level Amputations
What Happens at This Level?
Finger-level amputations may seem small, but they come with real challenges. Fine motor skills, grip strength, and daily functions like typing or holding small objects can all become difficult.
The muscles that control the fingers are mostly in the hand and forearm. If only the finger is gone, most of those muscles are still there.
That’s good news. It means EMS can still be very effective.
Setting Up EMS
For people with finger amputations, the goal is to keep the remaining muscles strong and responsive.
Pads should be placed over the intrinsic muscles in the hand and the flexors/extensors in the forearm. These are the muscles that open and close the fingers.
The pulses should be low to medium strength. The goal is not to overwork but to support natural movement.
Start with short sessions—maybe 10 to 15 minutes. Slowly increase the time as the muscles adapt.
Goals to Aim For
With finger-level EMS therapy, you’re mainly helping the person keep strength, prevent stiffness, and prepare the body to work with assistive tools or devices.
It can also help people who get a Grippy Mech Finger, our mechanical solution that boosts grip for partial hand amputees.
Consistency is key. The more regular the sessions, the better the results.
Customizing EMS for Partial Hand or Wrist-Level Amputations
Muscle Challenges at This Level
When someone loses more than just a finger—like the palm or wrist—the situation changes. The hand’s power comes from the combined work of the hand and forearm.
At this level, many of the fine control muscles are gone, but some large ones in the forearm are still usable.
That’s where EMS comes in. It helps rebuild connection to these remaining muscles.
Electrode Placement Tips
In this case, electrode pads should be placed along the forearm muscles—mainly the flexor and extensor groups.
You may need to try a few spots to find the best response. Every person’s muscle layout is a little different.
Use medium pulse strength. Make sure the person can feel the stimulation but isn’t in pain.
If they feel a “tug” or light muscle contraction, you’re in the right zone.
Recommended Sessions
Sessions can start around 15 to 20 minutes. Focus on both stimulation and rest time.
Alternate days work well, especially in the beginning. Once the muscles get stronger, daily sessions are okay.
Encourage slow, controlled movements during EMS. Ask the person to try and move their limb while the device stimulates. This helps reconnect brain and muscle.
Customizing EMS for Below-Elbow (Transradial) Amputations
Understanding the Muscle Map

In below-elbow amputations, the hand and wrist are gone, but the forearm remains—at least partly. This is where many of the muscles that control the hand live.
This level is actually great for EMS because it gives us a lot of muscle to work with. These muscles are also the ones used in myoelectric control for bionic hands like Grippy™.
But, without the hand, these muscles can become lazy. EMS helps bring them back to life.
Where to Place the Electrodes
You want to target both the flexor group (palm-side of the forearm) and the extensor group (back of the forearm).
Start by placing electrodes over the thickest part of the muscle. You can ask the person to try and squeeze or move their phantom hand while you feel for muscle movement.
This helps you find the right spots. You’ll often need to adjust slightly to get a clear, strong contraction.
Some users benefit from dual-channel EMS—stimulating both flexors and extensors at the same time.
Pulse Strength and Session Design
At this level, you can usually go with medium to high pulse strength. The person should feel a firm but comfortable contraction.
Start with 20-minute sessions. Break it into cycles—5 seconds on, 10 seconds off. This prevents fatigue and trains the muscle in short bursts.
It’s important to combine EMS with active attempts. Ask the user to try and move the phantom limb along with the pulse. This builds a strong brain-muscle link.
Building Toward Prosthetic Use
If the person is planning to use a bionic hand, EMS is more than just therapy—it’s training.
Each session helps improve muscle response and signal quality. This is exactly what a myoelectric prosthetic like Grippy™ needs.
Think of EMS as step one. The better the muscles respond, the better control the person will have over their bionic hand.
Customizing EMS for Above-Elbow (Transhumeral) Amputations
What Makes This Level Different?

In above-elbow amputations, the entire forearm is gone. This changes everything.
The muscles we once used for hand and wrist control are no longer there. But the biceps, triceps, and deltoids in the upper arm and shoulder are still present.
This means EMS needs to shift focus. Now, we’re not just trying to activate old pathways—we’re trying to create new ones.
This is one of the most advanced levels of EMS customization.
Electrode Placement at This Level
Electrodes should be placed over the biceps and triceps to begin with. These muscles can be trained to send myoelectric signals for prosthetic control.
You can also target the deltoid muscle, especially if the prosthesis will include shoulder or upper-arm movement.
Placement is trickier here. The muscles are deeper and respond differently. You might need to test different spots and strengths before finding what works.
Use larger pads to cover more area, and make sure the stimulation is strong enough to feel but never painful.
Adjusting Intensity and Timing
Start with low to medium pulse strength. Slowly increase as the muscles get used to it.
Sessions should be shorter—about 15 minutes—to avoid fatigue early on.
As the muscles strengthen, you can work up to 25–30 minutes with breaks in between.
Train each muscle group separately first. Then, begin combining movements—like contracting biceps and relaxing triceps in sequence. This helps simulate natural movement.
Goals and Expectations
The goal here is muscle education. These muscles weren’t built to control a hand—but with EMS and practice, they can learn.
Some users may need targeted muscle reinnervation (TMR) surgery. EMS helps prepare the muscles for this, and supports recovery afterward.
Don’t expect fast results. Progress is slower, but incredibly meaningful. With time, these sessions open the door to real, functional prosthetic control.
Special Considerations: Congenital Limb Differences
EMS for Those Born Without a Limb
Not every person with an amputation lost their limb later in life. Some were born without it.
This creates a unique challenge. Their brain never had a map for that missing limb. The muscles are often underdeveloped or used for different tasks.
Can EMS still help? Yes—but with a few changes.
Finding Muscles That Can Learn
In congenital cases, you have to look at what muscles are available and active. Even if they’ve never controlled a hand, they can still be trained.
EMS should start gently. Use very low pulse strengths and short sessions—just 5 to 10 minutes at first.
The goal isn’t muscle strength, but neuromuscular learning. You’re building a bridge between the brain and a new function.
Start Small, Grow Slowly
Progress will be slower than in acquired amputations. But don’t be discouraged.
With careful planning and regular sessions, many people with congenital limb differences learn to use myoelectric devices effectively.
BrawnBand and EMS tools can become powerful allies in this learning journey.
Integrating EMS with Daily Life
Making EMS a Habit

The best EMS sessions aren’t just about what happens in the clinic. They’re about building a routine that fits naturally into daily life.
Set a regular time for therapy—like after breakfast or before bed. Having a fixed time makes it easier to stay consistent.
Even short sessions matter. Just 15 minutes a day can create real progress over time. Skipping a day occasionally is fine, but staying regular gives the best results.
If the user is working, studying, or traveling, try to adjust the timing—not cancel it. Portable EMS units can make therapy easy to carry anywhere.
Listening to the Body
EMS should never hurt. It might feel strange—like tingling or pulsing—but pain is a sign to stop and readjust.
Each person will have a different tolerance. What feels strong to one may feel mild to another.
Encourage users to speak up if something feels off. Pay attention to redness, muscle fatigue, or discomfort during or after sessions.
Give muscles time to rest. Just like exercise, muscles need recovery time too.
Combining EMS with Other Therapies
EMS works best when it’s part of a bigger plan.
Pair it with stretching, resistance exercises, or mirror therapy. These support both physical and mental healing.
For those using the Gamified Rehabilitation App by RoboBionics, EMS can be synced with fun, interactive movements. This makes therapy engaging and purposeful.
You can even use EMS while doing basic tasks—like trying to pick up objects or squeeze a ball. This trains the brain to connect the pulse with real action.
Keeping Track of Progress
Keep a journal or log of each session. Note things like:
- Where the electrodes were placed
- How strong the pulse was
- How the muscle responded
- How the user felt after
Over time, this creates a personal map of what works best.
It also helps if you’re working with a physiotherapist or prosthetist. They can adjust sessions based on these notes and keep progress moving forward.
EMS for Pain Management and Phantom Limb Sensation
What is Phantom Limb Pain?

After amputation, many people feel pain or tingling in the limb that’s no longer there. This is called phantom limb pain.
It can feel like burning, itching, or squeezing—and it’s very real, even though the limb is gone.
It happens because the brain still “thinks” the limb exists. The nerves keep sending signals, and the brain keeps listening.
EMS can help quiet this miscommunication.
How EMS Reduces Pain
By stimulating nearby muscles, EMS tells the brain, “this area is active and okay.”
This changes how the brain sees the limb and reduces the faulty pain signals.
Use low-frequency EMS—this is better for calming the nerves rather than building muscle.
Electrode placement depends on the pain location. Sometimes it’s best to place them above the amputation site, or even on the opposite limb.
Start with very gentle pulses. Pain relief should feel like a soft massage, not a workout.
Emotional Impact of Pain Relief
Reducing phantom pain isn’t just about comfort. It helps people feel normal again. It improves sleep, mood, and even social confidence.
Some users say that once the pain goes, they start feeling “connected” to their prosthetic. EMS helps create that connection.
And when paired with the Sense of Touch™ feedback in the Grippy™ hand, it creates an even stronger brain-body bond.
Safety Tips for Using EMS
Who Should Avoid EMS?
While EMS is safe for most people, there are a few who should be careful or avoid it completely.
People with heart problems, pacemakers, epilepsy, or skin infections should check with a doctor before using EMS.
Pregnant women should also avoid EMS unless approved by a medical expert.
Never place electrodes on the chest, neck, or head unless specifically trained to do so.
Proper Care and Use
Always clean the skin before placing pads. Dirty or oily skin can block signals or cause irritation.
Use fresh pads regularly. Worn-out pads won’t stick well and can reduce the session’s quality.
Follow the instructions for your EMS device carefully. Start slow, and never increase intensity too quickly.
If the skin becomes red or sore, take a break and let it heal before the next session.
Creating a Personalized EMS Plan
Start with an Assessment
Before starting EMS, it’s important to understand the person’s condition fully. What is their level of amputation? How much muscle remains? Are there any medical conditions or pain issues?
A detailed physical assessment helps set the direction for therapy. This is usually done by a prosthetist, physiotherapist, or a trained rehabilitation expert.
At RoboBionics, we always begin with a full review before suggesting any EMS or device plan. Each body is different, and so is every recovery.
Set Clear, Achievable Goals
Without goals, EMS can feel pointless. So the first step after assessment is setting clear goals.
These might include:
- Strengthening specific muscles
- Preparing for prosthetic use
- Reducing phantom pain
- Improving muscle memory
- Increasing control for fine movements
Each goal will shape the type, timing, and intensity of EMS sessions. And when you hit a goal, it builds motivation to keep going.
Adjust Based on Progress
A good EMS plan is never static. It changes as the person changes.
In the first few weeks, the focus may be on gentle stimulation. Later, it may shift to muscle building or coordination.
Track how the muscles are reacting. Are contractions getting stronger? Is pain going down? Is the person feeling more confident?
Use this feedback to tweak the plan—change pad positions, increase session length, or add new exercises.
Always check in emotionally too. If the user feels anxious, bored, or unsure, the plan should adapt to support them.
Bring the User Into the Process
Customization doesn’t just mean adjusting settings. It means listening to the person using EMS.
Let them ask questions. Teach them how the device works. Show them how to adjust it safely at home.
This builds independence and trust. The more the user understands EMS, the more likely they are to stick with it—and benefit from it.
Prosthetic success isn’t just about machines. It’s about people. Empowering someone with knowledge, tools, and a voice is the real win.
The Future of EMS and Prosthetic Integration
Smarter Devices, Smarter Therapy

Technology is moving fast. EMS is no longer just a standalone therapy. It’s starting to connect with smart prosthetics, apps, and feedback systems.
In the future, we’ll see EMS units that can adjust automatically based on muscle signals or prosthetic movements.
We’re already exploring ways to connect our Grippy™ systems with EMS and feedback loops to make training even more intuitive.
Imagine a world where your bionic hand helps guide your therapy—and learns with you.
AI, Data, and Real-Time Feedback
With AI, we can analyze how each muscle reacts to stimulation. We can fine-tune sessions in real-time. We can even predict what kind of prosthetic control a person will have—before they put on the device.
This means fewer mistakes, less frustration, and better outcomes.
And when EMS is linked to apps—like our Gamified Rehabilitation Platform—it becomes not just useful, but enjoyable. Users can see their progress, play games, and stay motivated.
Building Confidence with Care
As EMS becomes more advanced, we’ll never forget the most important part: the people using it.
Technology must serve human goals—like independence, dignity, and joy.
At RoboBionics, we design every EMS plan with these values in mind. We’re not just helping muscles fire. We’re helping people write new chapters in their lives.
Final Thoughts
No two people are the same. No two journeys are alike. That’s why customizing EMS sessions based on the level of amputation is not just helpful—it’s essential.
Whether someone has lost a finger or a whole arm, EMS can make a difference. It can rebuild strength, restore control, ease pain, and prepare the body and mind for a new kind of movement.
But it only works when it’s personal. That’s what we do best at RoboBionics.
We listen. We adjust. We walk with each user through their journey—step by step, pulse by pulse.
Want to explore how EMS and bionic technology can support your recovery or help a loved one?
Schedule a free demo today: https://www.robobionics.in/bookdemo
We’re here to help. Always.



