Older adults experience prosthetic care very differently from younger users.
Their bodies change more quickly, their balance becomes more delicate, and even small discomforts can lead to big setbacks.
Because of this, doctors need outcome measures that reflect the realities of aging—frailty, fall risk, day-to-day stability, and goals that feel safe, realistic, and meaningful.
Frailty indices help doctors understand how strong or vulnerable the patient is before and after prosthetic fitting.
Falls per 1,000 days reveal how safely the patient moves through daily life.
Goal-setting keeps care plans personal, purposeful, and deeply human.
Why Geriatric Prosthetic Care Requires a Different Lens
How Aging Changes the Body’s Response to Prosthetic Use

Older adults have weaker muscles, slower reaction times, and reduced endurance.
These changes affect how they walk, how long they can stand, and how confidently they shift weight onto the prosthetic side.
Even a small alignment issue can feel overwhelming because the body cannot compensate the way it once did.
This is why doctors must assess prosthetic outcomes with tools designed specifically for aging physiology.
Measures that work for younger adults fail to capture the nuances of frailty, fatigue, and slow healing seen in geriatric care.
Why Frailty Becomes Central to Every Decision
Frailty increases the risk of falls, pressure injuries, joint strain, and exhaustion.
A frail patient may struggle with simple activities like stepping off a curb or turning around in a tight space.
If frailty is not measured, clinicians might set goals that are too hard, too fast, or too risky.
Frailty indices help doctors create safer plans by revealing the patient’s true physical reserve.
Why Safety Takes Priority Over Speed
Older adults value stability and comfort more than speed or performance.
A prosthesis that feels steady builds trust, while one that feels uncertain increases fear and reduces use.
This emotional component affects gait, posture, and even willingness to socialize.
Doctors rely on outcome measures that prioritize safety and confidence over technical perfection.
Understanding Frailty in Prosthetic Users
What Frailty Really Means in Clinical Practice
Frailty is not just weakness—it is the body’s reduced ability to bounce back from stress.
A frail patient may tire easily, lose balance quickly, or struggle to recover from small medical setbacks.
In prosthetic care, frailty influences every part of the journey, from wound healing to gait training.
Understanding frailty helps doctors predict how much support the patient will need and how fast they can safely progress.
Why Frailty Must Be Measured Before Fitting
If frailty is high before fitting, the first prosthesis may need extra stability, lighter materials, or simpler components.
Doctors can adjust expectations for walking distance, weight-bearing, and outdoor mobility.
This protects patients from frustration and reduces the risk of early falls.
Frailty scores guide safe pacing and reduce the chance of complications during early rehab.
How Frailty Scores Change After Fitting
A well-fitted prosthesis can reduce frailty by improving activity levels.
Walking becomes easier, muscles stay engaged, and circulation improves.
But a poor fit can worsen frailty by increasing fatigue, pain, and fear.
Tracking frailty over time helps doctors understand whether the prosthesis is enhancing health or adding stress.
Key Frailty Indices MDs Can Use
Grip Strength and Sit-to-Stand
Grip strength and sit-to-stand tests offer quick insights into total body strength.
Low scores suggest that the patient may struggle with sudden weight shifts or quick posture changes.
These tests help predict fall risk and guide exercise recommendations.
They also help determine whether the patient can safely manage higher-activity prosthetic components.
Walking Speed and Gait Quality
Walking speed is one of the strongest predictors of overall survival in older adults.
Slower walking—especially with uneven step lengths—signals reduced stability.
Doctors track these changes to adjust the prosthetic design, alignment, and training plan.
Walking speed also helps predict whether the patient can manage community ambulation or should focus on indoor-only routines.
Fatigue Levels and Recovery Time
Older adults often take longer to recover from activity.
If the patient becomes exhausted after short tasks, it suggests high frailty and low endurance.
These insights help shape goals that feel achievable and supportive.
Fatigue patterns also guide decisions about walker use, home safety planning, and fall prevention.
Why Falls per 1,000 Days Is a Critical Metric
How This Metric Shows True Safety Over Time
Single fall assessments do not capture the full risk.
But tracking falls per 1,000 days offers a clear, long-term picture of stability.
This metric shows whether the patient is improving or becoming more vulnerable as time passes.
It also highlights whether interventions—like alignment changes or strength training—are actually reducing falls.
Why Falls Reveal More Than Gait Assessments
A patient may walk well in the clinic but still fall at home.
Falls show how the prosthesis performs during real-life challenges—dim lighting, uneven surfaces, wet floors, or crowded spaces.
They reveal whether the patient can react quickly and maintain balance under stress.
This makes falls per 1,000 days one of the most honest indicators of prosthetic success.
How Falls Impact Emotional Health
Falls create fear.
Even one fall can make an older adult avoid walking, withdraw socially, or rely too much on caregivers.
This fear reduces prosthetic use and accelerates frailty.
Tracking falls helps clinicians identify early emotional impact and address it before confidence fades.
How Doctors Can Reduce Falls Using Outcome Data
Adjusting Socket Fit and Suspension Early

Older adults cannot tolerate loose or rotating sockets.
Even slight movement inside the socket can cause missteps or knee instability.
By tracking falls and frailty, doctors can identify when socket changes are urgently needed.
A stable socket dramatically improves confidence and balance.
Revising Alignment to Match Strength
Weak hip and core muscles increase the need for precise alignment.
If alignment is too aggressive or too neutral, the patient may struggle to control the prosthesis on slopes, stairs, or uneven ground.
Fall patterns alert clinicians to alignment problems that are not visible during short clinic walks.
Even small adjustments can prevent major falls.
Adding Stability Components Thoughtfully
Sometimes older adults need prosthetic feet that offer more ground contact or better shock absorption.
Other times they need stance-control knees or softer heel cushions to reduce impact.
Falls per 1,000 days helps clinicians decide when to introduce these components.
These upgrades often lower fall frequency significantly.
How MDs Should Approach Goal Setting in Geriatric Prosthetic Care
Why Goals Must Fit the Patient’s Life
Older adults value simple, meaningful goals—walking to the bathroom safely, cooking for themselves, attending social gatherings, or visiting family.
Goals that align with daily routines create motivation and reduce frustration.
Doctors set goals based on functional outcomes, not unrealistic expectations.
When goals feel personal, patients stay engaged and hopeful.
Why Goals Should Be Flexible
A frail patient may have good days and bad days.
Goals must adjust to energy levels, pain patterns, and emotional changes.
Flexible goals reduce guilt and help the patient feel supported, not pressured.
This approach encourages a steady, compassionate recovery pace.
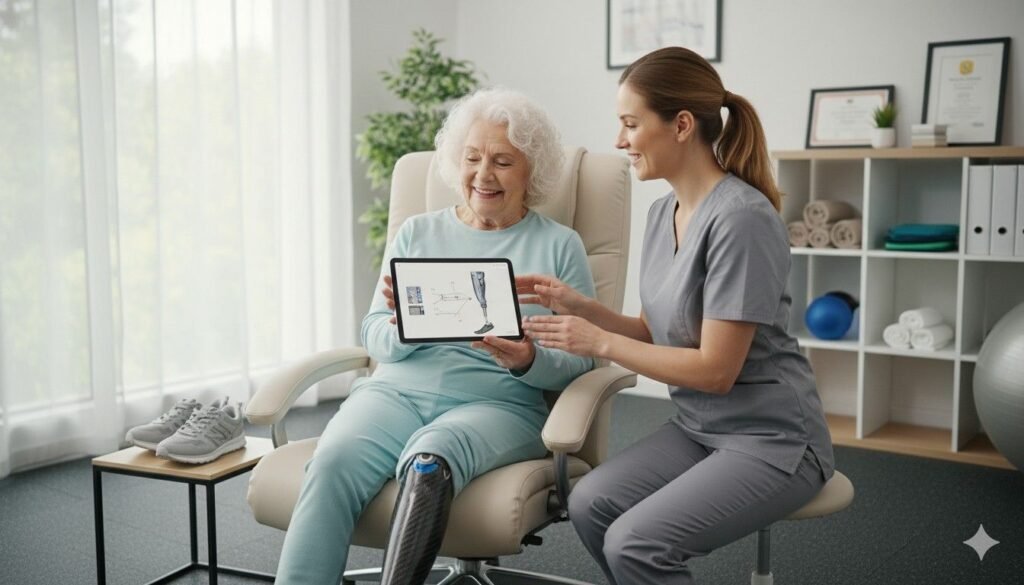
Why Collaborative Goal Setting Matters
Doctors, therapists, caregivers, and patients all play a role.
When everyone understands the goals, care becomes smoother and more coordinated.
Shared goal setting also ensures that expectations remain consistent and achievable.
This reduces confusion and increases the likelihood of sustained prosthetic use.
How Aging Affects Balance, Coordination, and Prosthetic Adaptation
How Balance Declines With Age
As people grow older, their inner ear function weakens, their reflexes slow down, and their vision becomes less sharp.
These changes make balance more fragile, especially when using a prosthesis.
Even simple movements—turning quickly, stepping backward, or reaching sideways—become harder to manage safely.
When balance declines, confidence declines as well.
Older adults may shorten their steps, look down constantly, or avoid walking outdoors.
These adaptations protect them in the short term but increase frailty in the long term.
This is why balance assessments remain essential in geriatric prosthetic care.
Why Coordination Becomes More Challenging
Coordination relies on the brain, muscles, and joints working together smoothly.
With age, neural processing slows, muscles weaken, and joint stiffness increases.
When a prosthesis is added to the mix, the body must work harder to maintain smooth motion.
Older adults may struggle with multi-step movements like stepping onto curbs, turning around, or reaching for support while walking.
These challenges increase fall risk and reduce independence unless addressed early.
Doctors can use frailty scores and fall metrics to detect these coordination issues before they cause injury.
How Speed Loss Impacts Prosthetic Adaptation
Older adults naturally move more slowly.
This affects their ability to react to sudden changes—like tripping, uneven surfaces, or slippery floors.
A prosthesis that feels slightly unstable can be overwhelming for someone with slowed reaction time.
This is why prosthetics for older adults must prioritize stability over speed.
Predictable foot behavior, smooth knee reactions, and secure socket suspension help offset slower reflexes.
Outcome metrics help clinicians ensure these features match the patient’s capabilities.
How to Use Frailty and Fall Data to Personalize Prosthetic Components
Matching Foot Type to Frailty Level
A frail patient often needs a prosthetic foot with strong ground contact and gentle roll-over.
Feet with aggressive push-off or high energy return may feel too unstable.
Foot selection should match the patient’s balance, endurance, and walking speed.
Fall frequency helps clinicians identify when the foot is too “lively.”
If falls increase on uneven ground, switching to a more stable foot often reduces the risk significantly.
Selecting Knees That Match Reaction Ability
Older adults may struggle to control fast-moving prosthetic knees.
They benefit from stance-support mechanisms that lock or resist bending during weight-bearing.
Knees with built-in safety features reduce fall risk for users with slower reactions.
Frailty indices and fall patterns guide clinicians in choosing knees that keep patients steady during both planned and unplanned movements.
The right knee transforms fear into confidence.
Choosing Socket Designs That Prevent Skin Breakdown
Older adults have thinner skin and reduced circulation.
This increases the risk of bruising and pressure sores.
A well-designed socket distributes pressure evenly and avoids sharp edges or rigid areas.
Falls and frailty scores help clinicians see when skin health is becoming compromised.
If discomfort increases, it may be time for softer liners, more breathable materials, or a new socket shape.
Comfort and safety always go hand in hand in geriatric care.
How Falls Influence Mental Health and Prosthetic Acceptance
Why One Fall Can Change Everything
A single fall can erase weeks of progress.
Older adults may become suddenly fearful, avoiding walking unless absolutely necessary.
They may refuse to use the prosthesis altogether and turn to wheelchairs or caregivers for support.
This emotional reaction is natural, but it must be addressed quickly.
Doctors and therapists can use fall metrics to identify when emotional support and targeted training are urgently needed.
How Fear of Falling Creates a Vicious Cycle
When older adults avoid walking, their muscles weaken even more.
Weakness increases risk of falling, which creates even more fear.
This cycle leads to rapid loss of independence.
Clinicians break this cycle by creating goals that rebuild confidence—safe indoor walking, supported training, and gentle balance exercises.
These small steps help the patient believe in their body again.
Why Emotional Support Improves Outcomes
Older adults often feel embarrassed after a fall.
They may hide the incident, fearing they will lose independence or be seen as a burden.
But acknowledging the emotional impact helps clinicians create a supportive environment.
Encouragement, patience, and reassurance help the patient move past fear and return to safe, steady use of their prosthesis.
How Doctors Can Use Goal Setting to Improve Geriatric Outcomes
Setting Goals That Match Energy Levels

Older adults may not have the stamina for long walks or high-intensity activities.
Goals must match their physical limits while still encouraging progress.
Short, achievable tasks—like walking from the bedroom to the dining area—build steady improvement.
These small successes reinforce confidence and reduce resistance to using the prosthesis.
Allowing Goals to Change With Health Status
Geriatric patients experience fluctuations due to illness, fatigue, medication effects, or pain.
Rigid goals fail because they do not account for these changes.
Flexible goals help patients feel supported instead of pressured.
When doctors adapt goals to meet health status, patients stay engaged without feeling overwhelmed.
Making Goals Meaningful, Not Mechanical
Older adults are motivated by purpose, not precision.
A goal like walking to the garden, attending family events, or enjoying a daily routine feels more inspiring than a target distance.
Meaningful goals also reduce the emotional impact of small setbacks.
When goals feel personal, patients work harder and stay connected to their prosthesis.
How to Integrate Frailty and Fall Metrics Into Daily Practice
Using Frailty Scores to Guide Visit Frequency
Frailer patients need closer follow-ups to prevent complications.
Doctors can schedule appointments based on frailty levels rather than fixed timelines.
This ensures problems are caught early and addressed before they become serious.
This approach also reduces emergency visits and hospital readmissions.
Using Falls per 1,000 Days to Predict Equipment Needs
A rise in fall frequency often signals that the prosthesis needs adjustment.
It may mean the knee is too loose, the foot lacks stability, or the socket fit is slipping.
Tracking falls helps clinicians see these issues long before injury occurs.
This proactive approach leads to faster interventions and fewer long-term complications.
Charting Progress Using Both Metrics Together
Frailty indices show vulnerability.
Fall metrics show real-world safety.
Together they create a full picture of the patient’s mobility and confidence.
Doctors can track improvement over months and adjust goals, devices, and therapy plans accordingly.
How Families Support Geriatric Prosthetic Outcomes
Why Caregivers Must Understand Frailty and Falls
Caregivers often assist with walking, bathing, dressing, and household movement.
If they understand frailty and fall patterns, they can offer safer, more appropriate help.
Educated caregivers prevent accidents and improve emotional well-being.
Doctors can guide caregivers with simple instructions that make daily care easier.
Encouraging Safe Independence Without Overprotection
Caregivers often try to help too much, fearing the patient may fall.
But too much help reduces confidence and increases frailty.
Safe independence is the goal—movement that is monitored but not restricted.
Clinicians teach caregivers how to strike this balance.
Building a Supportive Emotional Environment
Older adults often feel guilty asking for help.
A supportive family environment reduces pressure and encourages positive self-esteem.
This emotional safety helps the patient engage more with their prosthesis.
Family involvement is one of the strongest predictors of long-term prosthetic use.
How Clinicians Can Optimize Home Environments Using Outcome Data
Reducing Fall Hazards Based on Patient Risk

Frailty and fall metrics tell doctors where to focus home modifications.
If falls occur during turning, wider walkways may help.
If falls occur at night, better lighting may be needed.
Each intervention lowers risk.
This targeted approach prevents accidents and makes the home safer.
Choosing the Right Walking Aids Based on Mobility Score
Some older adults need walkers or canes alongside their prosthesis.
Outcome metrics help clinicians determine the right tool and the right timing.
Choosing the correct walking aid improves stability and reduces caregiver strain.
This improves confidence and encourages more daily walking.
Teaching Safe Movement Strategies in Real Rooms
Clinicians can help patients practice navigating their kitchen, bathroom, or bedroom using personalized fall and frailty data.
This real-life training improves safety far more than clinic-only exercises.
It also reduces anxiety about moving at home.
Conclusion
Geriatric Prosthetic Care Requires Deep Understanding and Gentle Precision
Older adults deserve prosthetic care that honors their limits, respects their dignity, and supports their daily routines.
Frailty indices help doctors understand physical vulnerability.
Falls per 1,000 days reveal real-world safety and emotional readiness.
Thoughtful goal setting keeps care grounded in what truly matters to the patient’s life.
When clinicians use these tools consistently, they create safer pathways, reduce injuries, and build stronger confidence in every step the patient takes.
With the right prosthesis, the right goals, and the right support, older adults can move forward with comfort, dignity, and renewed independence.