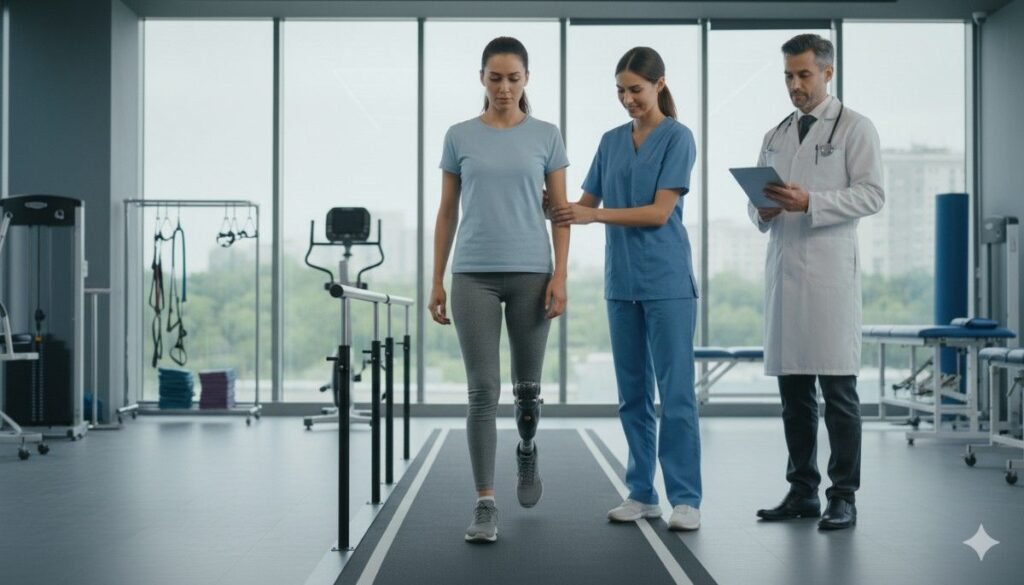
How long a person actually wears their prosthesis each day says more about comfort, trust, and usefulness than almost any other measure in prosthetic care.
When a device stays on, it becomes part of life.
When it stays off, it becomes a barrier to daily movement.
Clinicians use wear-time and real-usage tracking to understand this difference clearly and to make sure every user gets the most out of their device.
Why Device Uptime Matters in Prosthetic Care
How Daily Wear Shapes Real Progress
Daily wear is the heart of prosthetic success.
A device can be advanced, strong, and beautifully built, but if it stays on the table more than it stays on the user, it cannot change their life.
Uptime tells the real story.
It shows how often the prosthesis becomes part of daily movement instead of remaining a tool that feels difficult or tiring to use.
When a user wears their device for long, steady periods, their body adapts faster.
Joints stay flexible, muscles stay active, and balance becomes more natural.
These improvements cannot happen when the prosthesis is used only once in a while.
How Wear Time Reflects Comfort and Trust
People wear what feels good.
They remove what hurts or scares them.
This simple truth makes wear time one of the clearest signs of comfort.
If a user removes the prosthesis often, clinicians know something is wrong—maybe a pressure point, maybe sweat buildup, maybe fear of slipping, or maybe emotional distress.
If a user keeps the device on from morning to evening, clinicians gain confidence that the socket fits well, alignment is stable, and control is intuitive.
This connection between comfort and wear time helps guide care more accurately than quick clinic evaluations.
Why Wear-Time Data Helps Clinicians Make Better Decisions
In the clinic, a user walks for only a few minutes.
They stand, move, sit, and show what the device can do.
But real life lasts all day.
It includes heat, long walks, waiting for buses, working, cooking, and interacting with others.
Wear-time data shows how the prosthesis behaves in this real world.
Clinicians use this information to understand what is working and what needs attention.
It helps them adjust the fit, alignment, suspension, or training plan based on actual behavior, not assumptions.
Understanding Device Uptime and Adherence
What Uptime Means in Practical Terms
Uptime shows how long the device stays on and active.
It reflects the total hours the user feels comfortable wearing and moving with their prosthesis.
High uptime means good fit, strong confidence, and meaningful integration into daily routines.
Low uptime warns clinicians that the user may be struggling, even if they do not say it directly.
In prosthetic care, uptime is not simply a number.
It is a picture of how well life and device are blending.
What Adherence Means for Prosthetic Users
Adherence is not about forcing the user to wear the device.
It is about supporting them so much that they want to wear it.
When adherence is high, users engage more with therapy, practice movements regularly, and push themselves to improve mobility.
Low adherence often signals deeper issues—skin irritation, socket discomfort, poor suspension, emotional overwhelm, or lack of training.
Clinicians look at adherence as a natural outcome of good care, not as a rule the user must follow.
How Real Usage Differs From Wear Time
Wear time only shows how long the prosthesis stays on.
Real usage shows how much the user actually does with it during that time.
A person may wear a prosthesis all day but use it minimally because they feel unsure, afraid, or unskilled.
Another person may use the prosthesis actively for hours even if total wear time is lower.
Clinicians study both numbers together because they reveal the full truth.
Wear time tells the story of comfort.
Usage time tells the story of function.
Together, they show the real impact of the device.
How Clinicians Track Wear Time in a Meaningful Way
Asking Users Directly But Gently

Many clinicians begin with simple questions—How long did you wear your device yesterday?
How many hours did you keep it on last week?
These questions help the patient reflect on their behavior.
But answers are not always precise because users often estimate or forget.
Still, conversations help clinicians understand the emotional and practical reasons behind wear patterns.
Using Daily Logs to Capture Honest Patterns
Some clinicians ask patients to record daily wear time in small notebooks, phone apps, or printed charts.
This helps users become more aware of their progress.
It also gives clinicians a clearer view of routines, challenges, and patterns that change through the week.
Logs show details that short conversations may miss—
days with high activity, days with discomfort, or days with emotional stress.
These details guide clinicians toward better care planning.
How Connected Devices and Sensors Help
Modern prosthetic devices sometimes include sensors that track how long the device stays on or how often it moves.
These tools offer accurate, minute-by-minute wear data.
They help clinicians see exactly when the device is most active and when users stop using it.
This precise data helps clinicians make decisions based on clear evidence rather than guesswork.
It also helps compare usage across days, weeks, and months for long-term improvement.
Understanding Real Usage: Movement, Activity, and Function
How Clinicians Measure Real Activity
Real activity includes every movement the user makes with their prosthesis—lifting, reaching, gripping, walking, turning, climbing, or stabilizing themselves.
Some devices record the number of grips, steps, movements, or load bearing.
These small mechanical actions add up to a full picture of daily function.
Clinicians use this information to see whether the user is truly benefiting from the device or simply wearing it passively.
Why Activity Tracking Matters More Than Ever
Prosthetic success is not measured by appearance or occasional tasks—it is measured by how easily the user performs daily life.
If activity is low, it may reflect fear of damaging the device, difficulty controlling it, or lack of confidence in movement.
Tracking real usage helps clinicians make targeted decisions—
perhaps the user needs better grip patterns, improved strength, different training techniques, or even a socket modification.
How Functional Movement Helps Identify Problems Early
Usage data often shows early signs of trouble before the user reports discomfort.
For example, a sudden drop in grip activity may show hand fatigue or emotional discouragement.
A change in walking patterns may show alignment or suspension issues.
These early clues allow clinicians to intervene quickly and prevent bigger problems later.
Why Wear Time Drops: What Clinicians Look For
Discomfort and Pressure Points
If a socket presses too hard or rubs the skin, wear time drops sharply.
Users may remove the prosthesis to escape pain or avoid irritation.
This signals the need for minor adjustments such as trimming edges, adding padding, or checking limb volume.
Emotional Fatigue and Confidence Loss
Emotional strain also affects adherence.
Users may feel nervous wearing the prosthesis in crowded places or during work.
They may feel embarrassed or uncertain about how others see them.
These emotions quietly reduce device usage even when the physical fit is good.
Clinicians monitor these signs during conversations and check-ins to offer timely support.
Activity Barriers at Home or Work
Sometimes wear time drops because of life changes—new jobs, long sitting hours, illness, or reduced mobility.
These changes affect not only physical ability but also motivation.
Clinicians look at usage patterns to adjust training or recommend routines that fit better with daily life.
How Clinicians Use Wear Time to Guide Care Decisions
Planning Socket Adjustments Based on Usage
If wear time drops, clinicians check the socket first.
A small fit issue can lead to big changes in confidence and activity.
Adjusting the socket early keeps the user comfortable and prevents long breaks from prosthetic use.
Updating Training Goals Based on Usage
Usage data helps clinicians decide what skills the user needs next.
If usage is high but movement is limited, they may work on strength or balance.
If usage is low but grip patterns look strong, they may focus on endurance or confidence.
Knowing When a Full Refit Is Needed
Long declines in wear time often signal that the limb shape has changed.
A new socket may be needed to restore comfort and stability.
Wear-time patterns help clinicians identify the right moment for a refit.
Why Wear-Time Matters for Long-Term Success
Building Habit and Body Memory

When users wear their prosthesis daily, the body learns faster.
Balance improves, gait becomes smoother, and muscle control becomes automatic.
These habits only develop through consistent daily use.
Preventing Deconditioning
Low wear time often leads to muscle weakness, stiffness, and reduced endurance.
This makes it harder to return to regular use later.
Clinicians track usage to prevent this downward spiral.
Supporting Emotional Well-Being
Regular prosthesis use brings emotional strength.
Users feel more independent, more involved, and more hopeful.
This emotional improvement keeps adherence strong and supports long-term recovery.
How Real-Usage Tracking Helps Clinicians Understand True Daily Function
Seeing the Difference Between Wearing and Actually Using the Device
A prosthesis may stay on the body for many hours, yet be used only lightly.
This is an important distinction because real function comes from movement, not just presence.
A user may keep the device on for comfort, for balance, or simply because removing it is inconvenient, but still avoid using it for grasping, lifting, or stabilizing tasks.
Clinicians need to know the deeper story—how the device is being used, not just how long it is being worn.
Real-usage tracking gives doctors this clarity.
It shows how the prosthesis behaves when life gets busy, when tasks require effort, and when emotional pressure builds.
It reveals whether the device is part of the user’s natural motion or only a passive companion.
These small differences become visible through sensors, activity logs, and thoughtful conversations that help uncover how life unfolds beyond the clinic.
Understanding How Movement Patterns Reveal Hidden Challenges
Every prosthesis affects posture, gait, and limb coordination in subtle ways.
Real-usage tracking captures these shifts by monitoring how often the user performs certain movements, how quickly they tire, and how confidently they handle tasks that require coordination.
If usage patterns suddenly drop, it may show that something in the body or mind has shifted.
For example, a user who once reached for objects freely may start avoiding that behavior if the socket becomes tight or alignment changes.
A user who once walked confidently may shorten steps if suspension fails or pain increases.
Real-time movement data becomes a gentle signal that something needs attention before the user even realizes it consciously.
Clinicians read these signals to understand whether the prosthesis still supports the user’s natural movement or if new challenges have entered the picture.
How Usage Data Reveals Emotional Readiness
Real usage also reflects emotional comfort.
A user who feels thrilled with their prosthesis often uses it for everything—lifting, stabilizing, exploring new motions.
A user who feels nervous may perform only the safest movements, even if wear time remains high.
Emotions shape behavior in powerful ways.
A person who is fearful of dropping objects or making mistakes may limit their movements quietly, even when the clinic sees no physical problems.
Real-usage patterns help clinicians notice these emotional barriers early so they can provide reassurance, additional training, or supportive coaching.
How Clinicians Gather Real-Usage Data in Practical, Human Ways
Listening Before Measuring
Even with modern sensors, real-usage tracking begins with conversation.
Clinicians ask gentle questions about how the prosthesis fits into the user’s day.
They ask about the small daily routines—how the device feels during cooking, writing, dressing, or commuting.
These questions give context to the data and help clinicians understand the user’s feelings behind every movement.
Listening first helps build trust, which makes users more open and honest about their challenges.
It also helps clinicians avoid misinterpreting numbers without understanding the story behind them.
Using Built-In Device Sensors
Many modern myoelectric and bionic prostheses include built-in logs that capture grip cycles, movement frequency, motor activity, and periods of rest.
These logs gently record how much the user is actually doing with the device throughout the day.
They show how often the user picks up objects, how long the device stays active, and when periods of inactivity occur.
Clinicians use this information to map patterns—times of high activity, times of hesitation, or times when fatigue sets in.
These patterns guide adjustments, training focuses, and future goals.
Using Wearable Sensors and External Tracking Tools
Some clinicians offer optional wearable sensors that track motion in more detail.
These sensors follow arm swings, shoulder rotation, and limb loading.
They reveal how smoothly the prosthesis joins natural movement without interfering or causing strain.
External sensors can also highlight areas where movement is compensatory—such as when the user leans heavily on the sound side during tasks.
Clinicians use this information to adjust alignment or recommend targeted strength exercises.
Building User-Logged Activity Diaries
Not every user has access to sensors, and not every clinic has advanced tools.
In these cases, activity diaries help bridge the gap.
Users write down short notes about what they used the prosthesis for during the day, how long they used it, and what tasks felt easy or hard.
These diaries help both user and clinician understand progress without overwhelming detail.
They encourage users to reflect on their own patterns, which often increases awareness, confidence, and motivation.
Common Reasons Real Usage Declines—and What They Reveal
Physical Barriers That Reduce Activity

Real usage often drops when the body feels strained.
If a socket becomes tight due to swelling or feels loose as the limb shrinks, the user will naturally use the prosthesis less.
Even minor discomfort can reduce grip activity, shorten steps, or limit reach motions.
Clinicians use this decline as a prompt to inspect fit, suspension, and alignment.
Sometimes the solution is as simple as sock management or a small trim adjustment.
Other times, a limb-shape change may require a new socket.
Fatigue and Energy Loss
Using a prosthesis takes energy, especially during the early stages of adaptation.
If the user feels tired too quickly, they may stop using the device for active tasks.
This fatigue could come from weak core muscles, poor gait mechanics, or simple emotional exhaustion.
Tracking usage highlights when fatigue patterns form.
Clinicians then design targeted exercises, posture training, or endurance-building routines to support the user.
Skills That Feel Too Hard
Sometimes users do not use their device because they feel unsure about how to perform certain tasks.
They may avoid two-handed activities, fine movements, or reaching for objects placed above shoulder height.
This avoidance shows up clearly in reduced usage data.
Clinicians respond by teaching simpler versions of the skill first, then slowly increasing complexity.
This step-by-step support helps rebuild confidence and improve daily function.
Emotional and Social Stress
Life stress plays a big role in prosthetic behavior.
Users may avoid using their device in front of others if they feel self-conscious or judged.
They may use it less during times of sadness, anxiety, or social withdrawal.
These emotional dips often appear in usage patterns long before the user mentions them.
Clinicians can respond with compassion, reassurance, and sometimes referral to counseling or peer support.
How Clinicians Turn Wear-Time Data Into Wise Decisions
When to Improve Socket Fit
If wear time drops but usage remains high during certain hours, the socket may be uncomfortable only at specific times of day.
This often happens with morning swelling or evening shrinkage.
Clinicians interpret these patterns to refine the fit, add volume management strategies, or adjust padding.
When wear time drops steadily across the entire day, a larger change—such as a new socket—may be needed.
When to Adjust Alignment
Sudden declines in usage during walking or reaching can indicate alignment issues.
A misaligned prosthesis makes the user work twice as hard during movement.
Clinicians use usage logs to identify which movements have become harder and adjust alignment accordingly.
When to Strengthen or Retrain Movement
If wear time stays high but movement remains limited, the user may need training instead of hardware changes.
They may need help practicing weight shifts, grip patterns, or coordination tasks.
Clinicians use these clues to design training sessions that match real daily needs.
When to Address Emotional Barriers
Sometimes usage drops while wear time remains high because the user feels afraid or discouraged.
Clinicians look at these patterns with empathy.
They ask questions gently and offer reassurance, peer support, or structured exercises that rebuild confidence.
This emotional work often leads to large increases in usage without changing anything about the device.
How Increasing Wear Time and Usage Improves Long-Term Outcomes
Better Muscle Coordination
Consistent wear builds muscle memory.
The more the user moves with their prosthesis, the more naturally their muscles coordinate with the device.
This helps reduce compensatory movements and prevents strain on the back, shoulders, and hips.
Smoother, More Confident Motion
Usage increases natural movement flow.
The body learns when to activate the prosthesis, how to stabilize, and how to shift weight without overthinking.
This leads to smoother walking, better posture, and more precise hand movements.
Lower Risk of Injury
When users wear the prosthesis consistently, they develop safer movement habits.
They avoid risky compensations like leaning or overusing the sound side.
This reduces falls, joint pain, and long-term gait problems.
Greater Emotional Freedom
Regular usage helps users trust their prosthesis as part of their identity.
They feel more independent, more capable, and more willing to participate in daily life.
This emotional stability supports long-term adherence and overall well-being.
How Clinicians Use Data to Support Daily-life Independence
Helping Users Build Routine

Wear-time patterns help clinicians guide users in creating daily routines that feel natural and achievable.
They suggest small morning steps, mid-day activity bursts, and evening stretches to keep the prosthesis part of everyday flow.
Preparing Users for Work, School, and Travel
Usage data shows whether users are ready for the demands of real environments.
If activity is low, clinicians help build the skills needed for work tools, public transport, or school routines.
Anticipating Long-Term Needs
Over months, usage patterns show how the user’s life is changing.
Clinicians use this insight to plan future fittings, upgrades, and training programs that support growing independence.
Conclusion
Wear Time Is More Than a Number—It Is a Story of Daily Life
Device uptime and real usage reveal how deeply a prosthesis fits into a user’s world.
These measures reflect comfort, trust, skill, confidence, and emotional readiness.
They help clinicians understand the whole person, not just the limb.
With thoughtful tracking, early intervention, and compassionate guidance, clinicians can help every user move from hesitation to freedom.
They can support smoother walking, stronger grips, and more confident daily activity.
Most importantly, they can help transform the prosthesis from a tool into a natural part of life.



