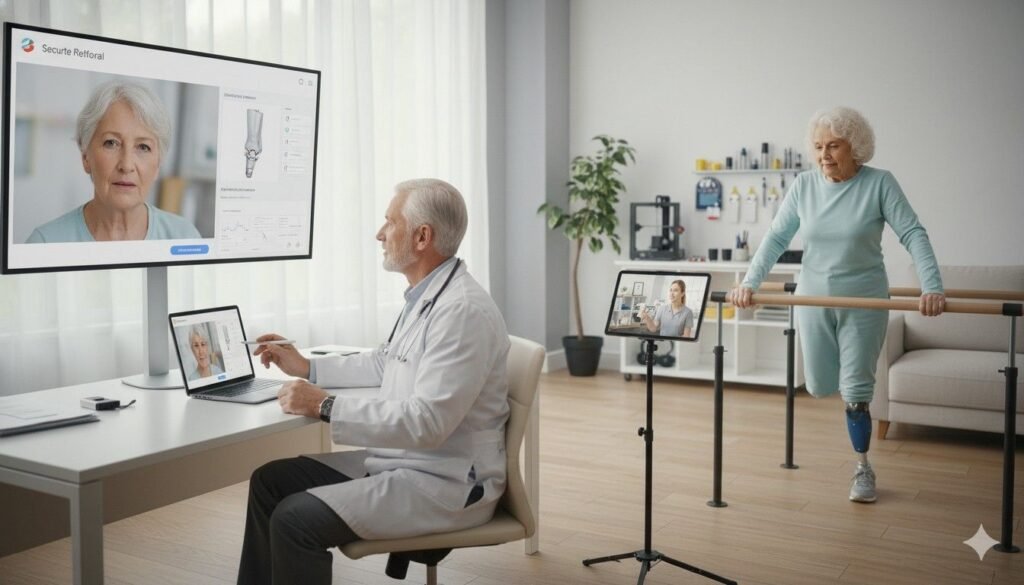
Balance shapes every part of life for a prosthetic user.
It affects how safely they walk, how steady they feel in crowds, how confidently they climb stairs, and how freely they move through their day.
Tools like the Berg Balance Scale (BBS) and Single-Leg Stance (SLS) test help doctors measure these abilities in a clear and structured way.
These tests show what the user can do, where they struggle, and how training improves stability over time.
Why Balance Matters Deeply in Prosthetic Care
How Balance Shapes Daily Confidence
Balance is not just a physical skill.
It is a quiet form of confidence that helps a person trust their body as they move through the world.
For prosthetic users, balance affects how safely they stand, how smoothly they turn, and how freely they take each step.
Good balance makes life feel easier.
It reduces fear of falling, lowers stress during movement, and encourages users to stay active.
Poor balance has the opposite effect.
It can make simple tasks feel risky and limit a person’s willingness to walk, climb, or try new activities.
This is why balance tests like BBS and SLS matter so much.
They help doctors understand how stable a user truly is beyond a quick look in the clinic.
The Link Between Balance and Prosthetic Fit
Balance does not depend only on strength or coordination.
It also depends on how well the prosthesis fits the limb.
A stable socket gives the user a steady foundation.
A loose or uncomfortable socket forces the body to work harder just to stay upright.
When balance drops, it may signal deeper issues.
Doctors may find that alignment is off, the socket is rotating, or the suspension is not secure.
BBS and SLS scores make these hidden problems more visible.
How Training Builds Better Balance Over Time
Balance improves with practice.
As users learn how to trust their prosthesis, their muscles grow stronger, their movements become smoother, and their reactions become quicker.
Training slowly shapes the way the body compensates and adapts.
These changes are easy to feel but hard to measure without structured tests.
That is where BBS and SLS help.
They capture progress in small, meaningful steps that both doctor and user can follow.
Understanding the Berg Balance Scale (BBS)
What BBS Measures
The Berg Balance Scale looks at how safely and steadily a person can perform daily standing and movement tasks.
It includes activities like standing up, turning around, reaching forward, stepping, and standing without support.
These simple tasks reveal how well a user controls their center of gravity.
Doctors value BBS because it connects directly to real-life situations.
If a user scores well on the test, they are more likely to move safely at home, in crowded rooms, and outdoors.
Why BBS Is Important for Prosthetic Users
Prosthetic users often rely on one side of the body more than the other.
This imbalance can affect posture, weight distribution, and confidence during movement.
BBS shows how well the user compensates and whether training or adjustments are needed.
A fall or stumble can quickly shake a user’s confidence.
Tracking BBS scores helps doctors identify early signs of instability before anything serious happens.
How Doctors Use BBS Scores Clinically
Doctors use BBS scores to understand the user’s current balance level and predict their risk of falling.
Low scores signal the need for focused training or socket adjustments.
Medium scores show progress but still indicate areas that need support.
High scores reflect stable, safe movement, but even then, doctors continue monitoring to ensure that stability remains strong.
These scores guide follow-up appointments and shape rehabilitation plans in a practical and personalized way.
Understanding the Single-Leg Stance (SLS) Test
What SLS Measures

The Single-Leg Stance test looks at a person’s ability to stay balanced while standing on one leg.
For most people, this movement is simple, but for prosthetic users, it is a clear window into how well they control their limb.
The test shows how stable the body is during weight shifts.
It reveals strength, coordination, and how securely the prosthesis supports the user.
Why SLS Is Valuable for Prosthetic Care
Standing on one leg is part of walking.
Each step requires the body to balance on one leg for a moment while the other leg swings forward.
If a user cannot maintain stability during SLS, it usually means they struggle during walking too.
SLS captures these challenges early, helping doctors make decisions before instability becomes a risk.
How SLS Guides Training and Adjustments
If the user wobbles quickly or cannot maintain the stance, it may mean their hip or core is weak.
It may also mean the socket does not support the limb well or the alignment is off.
Doctors use this information to guide targeted training such as hip strengthening, core control exercises, or weight-shift practice.
They may also adjust the prosthesis to improve stability during the stance.
How Prosthetic Fit Influences Balance Test Results
Socket Fit and Stability
A well-fitting socket gives the user a firm, steady connection to the ground.
It allows them to transfer weight smoothly without feeling pressure or slipping.
When the socket is loose or uncomfortable, the user instinctively shifts away from it.
This uneven weight distribution shows up clearly in both BBS and SLS scores.
Users may sway more, hesitate to stand on their prosthetic side, or lose balance during simple tasks.
Alignment and Posture
Proper alignment helps the user stand tall and balanced.
If alignment is off, the body tilts or rotates, forcing muscles to work harder just to stay upright.
These small posture changes have a large impact on balance.
They reduce SLS time and lower BBS scores.
Doctors watch for these patterns to decide whether alignment adjustments are needed.
Suspension and Confidence
Suspension systems keep the prosthesis securely attached during movement.
If suspension weakens, the prosthesis may feel unstable or unpredictable.
This creates anxiety and tension in the user’s body.
These feelings of uncertainty lower both physical performance and test scores.
Improving suspension can instantly raise confidence and balance.
How BBS and SLS Reveal Daily Life Challenges
Understanding Real-World Movements
Balance tests reflect daily tasks like stepping in and out of vehicles, climbing stairs, reaching for objects, or turning around quickly.
When users struggle with these tasks, it often becomes clear in their BBS and SLS performance.
These tests provide a structured way to measure challenges that happen unpredictably throughout the day.
Spotting Early Signs of Instability
Small changes in balance can go unnoticed by the user but become clear through a score drop.
A slight reduction in SLS time or difficulty completing a BBS task may signal a developing problem such as limb volume changes, muscle weakness, or emotional hesitation.
Doctors can act early—before falls, injuries, or loss of confidence occur.
Connecting Physical and Emotional Stability
Balance is strongly linked to emotional confidence.
When users feel unsure, they tense muscles, take shorter steps, or avoid certain movements.
These behaviors reduce balance scores.
Improving physical stability often boosts emotional stability too.
Users begin trusting their body again, which leads to smoother movement and safer steps.
Clinical Cutoffs That Doctors Should Know
BBS Cutoffs
BBS scores typically fall into ranges that predict fall risk and mobility.
Scores near the lower range often indicate high fall risk.
Middle ranges suggest moderate safety but need for continued training.
High scores show stable movement, though doctors continue monitoring for safety.
These cutoffs help doctors classify users accurately and plan personalized care.
SLS Cutoffs
SLS times also connect closely to fall risk and walking ability.
Shorter times often suggest difficulty maintaining weight on one leg.
Longer times show stronger control and body awareness.
Doctors use these cutoffs to understand how stable a user is during natural walking phases.
Why Cutoffs Matter for Prosthetic Users
Prosthetic users face more balance challenges than most people.
Cutoffs help doctors know when the user needs additional support, advanced training, or adjustments.
They also help track progress as training improves strength and coordination.
How Training Improves Balance Scores Over Time
Strength Training Effects
Training that focuses on the hips, core, and lower back helps users control their posture and weight distribution.
As these muscles get stronger, both BBS and SLS scores rise.
Users feel more stable during stepping, reaching, or climbing stairs.
Coordination and Reaction Training
Practicing weight shifts, stepping patterns, and directional changes helps users react faster during movement.
This type of training builds smoother, more controlled steps, which directly improves balance scores.
Confidence Training
Confidence grows with practice.
As users feel more comfortable with their prosthesis, they take stronger, steadier steps.
This emotional ease shows up clearly in longer SLS times and better BBS completion.
How BBS and SLS Scores Change Through Different Stages of Prosthetic Use
Early Use and the First Signs of Balance Adjustment

During the first weeks with a prosthesis, users often feel unsure about their balance.
They may take careful steps, lean toward their sound side, or avoid shifting weight onto the prosthetic side.
These hesitations are natural because the body is still learning how to distribute weight in a new way.
In this early stage, BBS scores tend to be low to moderate.
SLS times are usually short, especially on the prosthetic side.
Users may only manage a second or two before needing support.
These early results are not signs of failure—they simply reflect the beginning of the learning process.
Doctors expect these scores to rise slowly as the user gains confidence and starts trusting the prosthesis more.
Even a small increase in SLS time or one additional task on the BBS can signal meaningful progress.
Early balance changes are often subtle but incredibly important for long-term growth.
Middle Stage: When Control and Strength Improve
As users practice walking, turning, standing up, and stepping, their muscles grow stronger.
Their posture improves, their hips stabilize, and their steps become smoother.
These changes lead to visible improvements in balance tests.
BBS scores often rise steadily during this stage because users can perform more tasks without holding onto support.
They can reach forward without fear of falling and turn around with more ease.
These moments show that their center of gravity is becoming more stable.
SLS times also improve.
Users can stand on the prosthetic side for longer periods, sometimes doubling or tripling their early numbers.
This shows progress in core control and weight shift ability.
For many users, this stage is where confidence begins to grow more rapidly.
Long-Term Patterns: When Movement Feels Natural
After several months or even years of steady use, many prosthetic users achieve stable, consistent balance.
They walk with smoother rhythm, shift weight naturally, and rely less on visual cues for balance.
These improvements are reflected in higher BBS scores and longer SLS times.
Long-term users often show strong stability even during sudden movements like turning quickly or reaching to catch falling objects.
Their body learns to predict small shifts in weight and respond automatically.
Doctors look for sustained scores during this stage because consistency shows that the user has developed reliable motor skills.
If scores begin to drop suddenly, it often signals new issues such as socket loosening, alignment changes, or physical weakness due to inactivity.
Balance tests help detect these early signs long before falls or discomfort occur.
Using Balance Tests to Guide Socket and Alignment Adjustments
When Low Scores Point to Fit Problems
A sudden change in BBS or SLS performance often signals a problem with the prosthetic fit.
Users may struggle to stand evenly or shift weight comfortably.
They may wobble more than usual or feel unsure during small movements.
These issues often come from limb volume changes, which can make the socket feel tight or loose.
When the socket does not hold the limb securely, weight distribution becomes uneven.
This affects balance and lowers test scores.
Doctors use these score changes to decide whether the socket needs padding, reshaping, or a full refit.
A simple adjustment can often restore stability and bring scores back up.
When Scores Suggest Alignment Issues
Alignment plays a large role in balance.
If the prosthesis tilts slightly inward or outward, the body compensates in ways that make standing and walking harder.
Users may lean, twist, or shift weight awkwardly.
These small compensations reduce SLS time and make BBS tasks more difficult.
Users may find it hard to step forward smoothly or maintain balance during turning tasks.
By reviewing balance scores, doctors can identify whether alignment adjustments are needed.
Correcting alignment often leads to immediate improvement in balance performance.
How Suspension Affects Test Results
Good suspension gives the user a sense of security.
It keeps the prosthesis stable during movement, reducing the need for extra effort from the hips and core.
Poor suspension creates a feeling of instability that lowers both BBS and SLS scores.
If the prosthesis feels like it might slip or rotate, users become tense.
This tension affects posture and reduces their ability to shift weight naturally.
Doctors monitor SLS times closely because they reveal how confident the user feels placing full weight on the prosthetic side.
Improving suspension often leads to dramatic increases in balance performance.
How Emotional and Psychological Factors Shape Balance Scores
The Role of Fear and Hesitation

Fear of falling can significantly reduce balance performance.
Even if the body is strong enough, the mind may hold back.
Users may avoid shifting weight onto the prosthetic side because it feels unfamiliar or risky.
This hesitation shortens SLS time and reduces BBS success.
The body may sway more or move stiffly due to anxiety.
Doctors recognize these emotional signals in the scores.
They then help users build confidence through guided training, reassurance, and gradual exposure to challenging tasks.
Building Confidence Through Practice
As users practice walking, standing, and stepping, their confidence grows.
They begin trusting the prosthesis and their own ability to stay stable.
This confidence often leads to quick increases in SLS time because the user stops holding back.
BBS tasks also become easier because the user moves more freely.
They no longer rely heavily on visual cues or support, and their body reacts more naturally during movement.
Doctors encourage small daily activities to reinforce this progress—standing on the prosthetic leg while brushing teeth, shifting weight during cooking, or practicing stepping in place.
The Impact of Emotional Well-Being
Balance is closely linked to emotional health.
Stress, fatigue, or worry can reduce focus and muscle coordination, lowering balance scores.
On good days, users often perform tests with more confidence and smoother movement.
Doctors use these patterns to understand how the user is coping emotionally.
If emotional strain is lowering balance performance, they may recommend counseling, peer support, or structured guidance to rebuild comfort and stability.
How Training Programs Improve BBS and SLS Results
Strength Training for Better Stability
Hip and core strength are essential for good balance.
These muscles help the body maintain posture, shift weight, and stay steady during movement.
Training them leads to better control and smoother reactions.
As users build strength, their BBS scores improve.
They complete tasks more easily, stand up without swaying, and hold positions for longer.
SLS times rise as well, showing improved control on the prosthetic side.
Even small increases in strength can lead to big improvements in balance.
Weight-Shift Training for Natural Walking
Walking requires constant shifting of weight from one leg to the other.
For prosthetic users, this shift feels unnatural at first.
Weight-shift training helps the body relearn this movement safely.
As users practice shifting weight toward the prosthetic side, they gain trust in their limb.
BBS tasks like stepping and reaching become easier.
SLS improves because users no longer fear placing full weight on the prosthesis.
Doctors often use gentle exercises like rocking side to side, stepping in place, or shifting weight on a soft surface to improve these abilities.
Reaction Training to Improve Stability
Balance is not only about strength—it is also about reaction.
Users need quick, smooth responses when someone bumps into them, when a surface is uneven, or when they turn suddenly.
Reaction training helps the body stay ready for real-world challenges.
This training improves BBS tasks involving turning, stepping, and reaching.
It also extends SLS times because the user’s muscles respond more predictably.
Functional Training for Real-Life Movements
Training often includes activities like picking things off the floor, turning while carrying something, or stepping onto small raised surfaces.
These real-life tasks improve both physical balance and confidence.
As users perform these tasks more easily, their balance test scores rise.
They become more independent and safer in daily life.
How Doctors Can Use Balance Scores to Shape Individual Care Plans
Personalizing Training Based on Weak Points
BBS and SLS scores help doctors identify exactly where a user struggles.
If the user loses balance during stepping tasks, training can focus on gait stability.
If SLS is weak on the prosthetic side, the focus may shift to core strength and hip control.
This personalized approach helps users improve more quickly and efficiently.
Planning Follow-Ups Based on Score Changes
Steady improvement in scores shows that the current care plan is working well.
Drops in scores suggest the need for adjustments, new exercises, or socket changes.
Doctors use score trends to decide when to schedule follow-ups, when to update training, and when to intervene with refits or alignment checks.
Using Scores to Document Real Progress
Balance scores are easy to document and show clear patterns of growth.
They help doctors communicate progress to users, families, and care teams.
They also provide valuable support when applying for new devices, upgrades, or rehabilitation services.
How Balance Test Improvements Change Daily Life
Increased Independence

As users gain balance, they move through their day with more freedom.
They perform tasks without relying on support, feel safer walking outdoors, and regain confidence in crowded areas.
Reduced Fear of Falling
Better balance reduces anxiety.
Users worry less about tripping or losing stability.
This emotional comfort helps them stay active and involved in social life.
Improved Walking and Endurance
As balance improves, walking becomes smoother and less tiring.
Users can walk longer distances, climb stairs with more ease, and take on activities they once avoided.
Conclusion
Why Balance Tests Matter So Much in Prosthetic Care
Balance tests like BBS and SLS show what the user can do, how safe they feel, and how stable they are in real life.
They reveal progress, highlight struggles, and guide doctors toward the best care decisions.
When balance improves, life improves.
Users walk with confidence, move with ease, and live with greater independence.
These tests help doctors document these changes clearly and support users through every stage of their journey.



