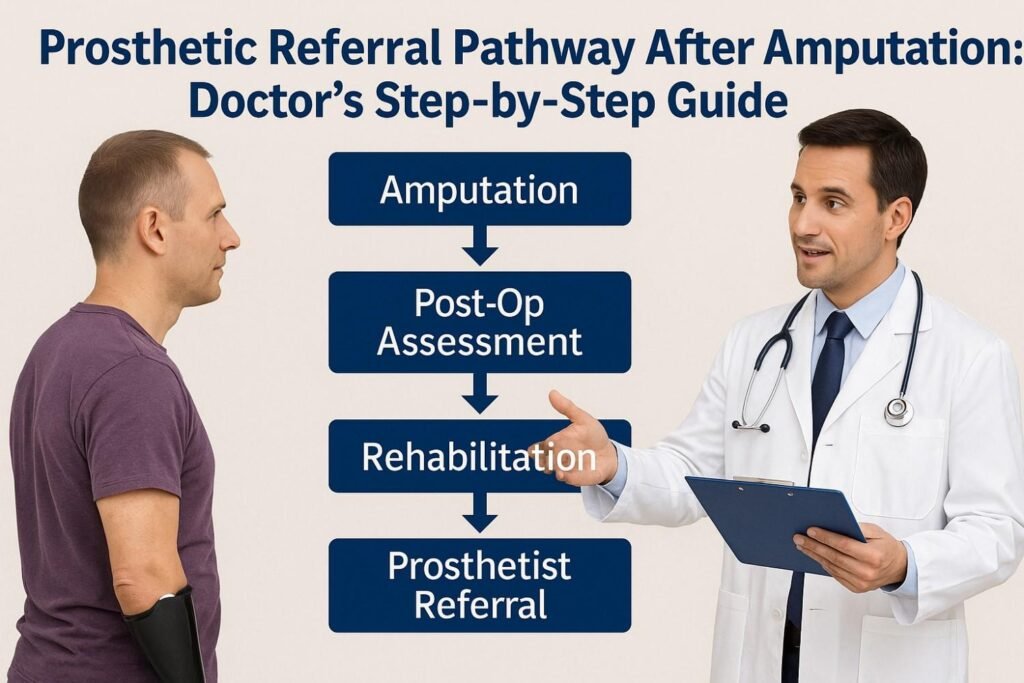
Every doctor who works with amputee patients wants the same thing: a smooth, clear, and well-coordinated path from surgery to full rehabilitation. Yet the prosthetic referral pathway is often confusing, rushed, or delayed. Patients may not know what comes next. Families feel overwhelmed. And doctors have to make quick decisions while handling complex medical needs.
A clear pathway changes everything. It helps patients heal better, move sooner, and trust the care they receive. It also makes the entire team work together with fewer gaps or mistakes.
This guide walks you through the complete prosthetic referral process step-by-step. It is written in simple words, designed for doctors, surgeons, and rehabilitation teams, and shaped by deep experience in prosthetic care in India. You will see what to check, when to act, who to involve, and how to ensure your patient gets the right prosthesis at the right time.
Early Post-Surgery Phase
Understanding the Patient’s Physical State
Right after surgery, the patient’s body is still adjusting to a major change. Pain, swelling and early healing needs often make them anxious or unsure about what lies ahead.
This is when a doctor sets the tone. How you explain their current state decides how confident they feel and how well they engage with later steps of rehabilitation.
When you walk them through what is normal and what is not, you remove fear and prepare them mentally for the next phases of recovery.
Stabilizing the Wound Area
The wound must reach a clean and stable state before any prosthetic planning begins. Doctors often notice that patients worry about how the wound looks, even before asking how long healing will take.
Clear guidance helps them stay patient during this period. When patients understand the goals of wound stabilization, they follow instructions better, which later reduces prosthetic complications.
A well-healed socket area with minimal tenderness is the foundation for a successful device fit.
Managing Pain Sensations
Pain management shapes the entire recovery experience. Patients often confuse surgical pain with phantom pain or residual limb discomfort.
Doctors who explain the difference early help the patient feel more in control. When pain is addressed in a structured way, patients move sooner, trust the care process more, and avoid unnecessary fear.
Good pain management also allows the rehabilitation team to start mobility sessions without hesitation.
Preparing the Patient Mentally
A patient’s mindset after amputation greatly influences how they handle rehabilitation. Many feel unsure about their future or worry about their independence.
Simple, calm conversations can reduce these fears. When a doctor takes a few minutes to help them understand the purpose of each stage, they feel supported rather than lost.
This early emotional preparation makes the prosthetic journey smoother and less overwhelming for everyone.
Pre-Prosthetic Assessment
Evaluating Residual Limb Shape and Volume

A proper evaluation starts with the shape, volume and condition of the residual limb. Doctors must observe how the limb settles during the first few weeks.
If swelling reduces slowly or unevenly, future socket fitting can become complicated. Early identification allows the patient to receive better limb-shaping support, which leads to better comfort with their prosthesis later.
A clear understanding of limb volume changes also helps decide when the patient is ready for casting or scanning.
Checking Skin Health and Sensitivity
Skin must be strong enough to tolerate the pressure of a prosthetic socket. Any fragile area, redness or sensitivity will become a problem later.
Doctors play a key role in advising how patients should care for their skin daily. Good hygiene and gentle massage techniques often protect the limb during the early phase.
When the skin is conditioned early, socket irritation and breakdown rates drop significantly.
Identifying Muscle Strength and Control
Muscle control is essential for stable prosthetic use. Many patients lose strength in the days after surgery due to fear of movement or pain.
Simple exercises recommended by the doctor help maintain muscle activation. Even small movements make a big difference in long-term mobility.
A strong residual limb creates a smoother transition into gait training and prosthetic alignment sessions.
Understanding the Patient’s Daily Needs
Each patient has a different lifestyle. Doctors must note their work, home environment and personal expectations before referring them for prosthetic planning.
A patient who walks long distances needs a different approach than someone who works mostly at a desk. Knowing their routine helps guide prosthetic selection from the beginning.
This patient-centered approach leads to better satisfaction and fewer later adjustments.
Discussing Medical Conditions That Affect Fitting
Some health conditions affect how quickly or comfortably a patient can use a prosthesis. Diabetes, vascular disorders, and neuropathy are common in many amputees.
Doctors need to assess these conditions carefully. Proper medical control can prevent wound issues or skin breakdown after fitting.
A stable medical profile ensures smoother progress once the patient starts rehabilitation with a prosthetic team.
Timing the Prosthetic Referral
Determining When Healing Allows a Referral
Choosing the right moment for a referral is a balance between medical readiness and patient motivation. Referring too early creates delays later, while referring too late slows rehabilitation.
Doctors should observe healing progress week by week. When the limb shows stable volume, clean skin, and controlled pain, the patient is often ready.
Good timing helps the prosthetic team start planning without unnecessary wait periods.
Preparing Documentation and Imaging
Clear documentation speeds up the prosthetic team’s assessment. Photos, wound notes, and any imaging help explain the patient’s current condition.
Doctors who provide detailed yet simple notes help avoid confusion later. It also prevents the patient from repeating their concerns multiple times.
Organized records reduce errors and give the prosthetic provider a strong starting point.
Guiding the Patient on What to Expect Next
Patients feel calmer when they know what the next step looks like. A short conversation about the referral, the team they will meet, and the timeline ahead makes everything feel manageable.
When patients feel guided, they show better cooperation during casting, testing, and training sessions.
A small moment of clarity now saves many questions later.
Communicating With Prosthetic Providers
Direct communication with the prosthetic team helps align expectations. When doctors share medical goals early, the prosthetist can match the device design to the patient’s needs.
A simple phone call or referral note prevents misunderstandings. This teamwork improves outcomes for both the patient and the rehabilitation center.
Cooperation between teams is one of the strongest predictors of long-term prosthetic success.
Working With a Prosthetic Team
Sharing Medical History and Key Concerns
The prosthetic team must understand the patient’s full medical picture. Any vascular issues, skin sensitivity, or movement limitations should be shared clearly.
When doctors provide these details early, it allows the prosthetic experts to plan safely. They can avoid socket pressure on fragile areas or choose softer liners for sensitive skin.
Clear communication also reduces the risk of delays in the fitting timeline.
Supporting the Patient During Their First Visit
The first prosthetic appointment is often emotional for the patient. They feel hopeful but also nervous, unsure, or overwhelmed by new information.
Doctors can help by preparing them mentally before the visit. When a patient arrives knowing what will happen, they feel more confident and less anxious.
This early reassurance shapes the entire experience in a positive way.
Explaining Different Prosthetic Options
Patients usually believe all prosthetic legs or arms are the same. Doctors can help them understand that different devices serve different needs.
Explaining the difference in simple terms helps patients focus on function rather than assumptions. The prosthetist then builds on this understanding during the consultation.
A well-informed patient makes better choices and feels more satisfied with the final outcome.
Answering the Patient’s Common Concerns
Patients often ask about weight, balance, comfort, and how long it takes to walk again. Doctors do not need to provide technical details but should give honest, simple explanations.
Short, clear answers build trust. Patients feel supported and prepared for the journey ahead.
When these concerns are addressed early, patients work more confidently with the prosthetic team.
Early Rehabilitation Planning
Starting Gentle Mobility Training
Early mobility helps prevent stiffness, muscle loss, and joint contractures. Doctors should guide patients to begin simple movements under supervision.
When mobility becomes a daily habit, patients recover faster. It also prepares their body for gait training once they receive the prosthesis.
Even light motion makes a significant difference during the early rehabilitation phase.
Protecting the Residual Limb From Pressure
Before a prosthesis is fitted, the limb must remain protected. Doctors need to show patients how to avoid pressure, friction, or sudden impacts on the healing area.
Proper protection prevents swelling flare-ups and skin irritation. This allows the prosthetic team to begin the fitting process sooner.
Safe handling of the limb also reduces the risk of long-term complications.
Using Shrinker Socks or Compression Techniques
Shrinkers help shape and stabilize the residual limb. Doctors should explain why they are important and how to wear them correctly.
A well-shaped limb fits more comfortably in a socket. Consistent use of compression tools helps control swelling and supports faster healing.
Patients who follow this step closely often require fewer adjustments later.
Building Confidence Through Early Exercises
Exercise routines do more than strengthen muscles. They rebuild confidence. Patients begin to feel like they are moving toward independence again.
Simple exercises like stretching, controlled lifts, or guided movements help them prepare for using a prosthesis.
When patients feel progress early, they become more motivated during later stages of gait training.
Psychological Support in the Referral Pathway
Recognizing Emotional Changes After Amputation

Amputation brings a major emotional change. Patients may feel sadness, confusion, or worry about their future.
Doctors should observe these signs gently. A few kind words and reassurance can relieve a lot of stress during this phase.
Understanding the emotional journey helps doctors guide patients more effectively.
Encouraging Honest Conversations
Patients often hide their fears to avoid troubling doctors. They may think their feelings are not important.
Encourage them to speak openly. Even short conversations help them process what they are going through.
Open communication builds trust and strengthens their engagement in rehabilitation.
Discussing the Role of Counseling if Needed
Some patients need deeper emotional support. Doctors can recommend counseling if they notice signs of depression or long-term anxiety.
Explaining that counseling is normal and helpful makes the patient more open to the idea.
Mental strength is as important as physical healing in the prosthetic journey.
Supporting Family Members During the Transition
Families also struggle to adjust. They want to help but often do not know what to expect.
Doctors can guide them with simple instructions and emotional reassurance. When families understand the pathway, they support the patient more effectively.
This family involvement improves the patient’s overall progress.
Socket Casting and Measurement
Preparing the Residual Limb for Casting
Before casting, the limb must be clean, dry, and calm. Doctors often remind patients to avoid applying creams or oils because they affect the shaping material. This small detail makes the casting more accurate and leads to a better socket fit.
Patients usually feel nervous during their first casting session. A clear explanation of the process helps them stay relaxed. When the patient knows the purpose and steps, they cooperate better and feel more confident.
Good limb preparation reduces errors and ensures the socket reflects the true shape of the limb.
Explaining the Purpose of Socket Casting
Many patients think the prosthetic leg is just chosen off the shelf. They do not realize it is built around their limb. Doctors play an important role in helping them understand why casting matters.
Once they understand that the socket is made to match their limb exactly, they become more patient and attentive. They realize that comfort depends on this stage.
This awareness often improves the quality of communication with the prosthetic team.
Helping the Patient Stay Still During Measurement
Even small movements during casting can alter the shape. Doctors can prepare patients by telling them that staying still is essential.
Some patients may feel itchy or restless as the casting material sets. Reassuring them and offering clear instructions helps them complete the process without issues.
A well-explained session builds trust between the patient and the prosthetic team.
Reviewing the Initial Shape and Measurements
After casting or scanning, the prosthetist reviews the shape. Doctors may be asked about any special considerations like sensitive areas, bone prominence, or planned medical follow-ups.
This is a good time for the doctor to share insights that may not appear in the measurements. These notes help the prosthetist create a safe and comfortable design.
Good collaboration during measurement leads to fewer adjustments later.
Selecting the Right Prosthetic Components
Understanding the Patient’s Mobility Level
Every prosthetic device is chosen based on how active the patient is. Doctors help categorize mobility levels based on their medical condition, lifestyle, and goals.
This step prevents patients from receiving a device that is too advanced or too basic for their needs. A well-matched component helps them walk safely and confidently.
Doctors guide expectations by explaining that stability comes first, and higher activity components come later.
Considering the Patient’s Weight and Strength
Weight and muscle strength affect how well a patient can manage their prosthesis. If someone has weak core strength or low endurance, the prosthesis must support stability more than speed.
Doctors help the prosthetist decide which foot, knee joint, or connector will suit the patient best. This ensures the device feels natural and safe.
The goal is to create a setup that supports long-term use without strain.
Matching Components to Work and Daily Routines
A patient who walks on uneven ground needs a different type of foot than someone who works in an office. Doctors understand the patient’s lifestyle better than anyone else in the care team.
Sharing these details helps the prosthetist choose a setup that fits the patient’s daily life. When the device matches their environment, the patient moves with more confidence.
This small alignment improves day-to-day comfort and satisfaction.
Adjusting Expectations for First-Time Users
First-time users often expect to walk like before their amputation. Doctors help them understand that the first prosthesis focuses on stability, safety, and learning.
Explaining this gently helps manage disappointment. When expectations are realistic, patients stay motivated during training and adapt more easily.
This simple step protects morale and improves overall progress.
Trial Fitting and Adjustments
Preparing the Patient for Their First Trial Fit
The first time a patient wears a test socket, they may feel excited or anxious. Doctors can explain that this is a temporary version used to find pressure points and alignment issues.
When patients know discomfort is normal at this stage, they communicate more openly. They report pressure points instead of hiding them.
Open communication helps the prosthetic team make better adjustments.
Checking for Pressure Spots and Redness
During the trial fitting, the prosthetic team checks how the limb reacts inside the socket. Doctors may also inspect the limb afterward to make sure there are no harmful pressure spots.
If redness appears in the wrong areas, it may indicate poor load distribution. Early corrections prevent long-term socket problems.
This cooperative check creates a safer and more comfortable final fit.
Improving Alignment for Balance and Stability
Alignment affects how well the patient stands and walks. Small changes can improve comfort and reduce strain on the joints.
Doctors often observe alignment during the trial phase and share feedback. If the patient feels unstable or leans to one side, adjustments can be made quickly.
Proper alignment improves walking mechanics and lowers the risk of secondary injuries.
Helping the Patient Develop Trust in the Device
The trial fit is not just about measurements. It is also the moment when the patient emotionally connects with the idea of using a prosthesis.
With calm words and steady encouragement from doctors, patients begin to trust the device. Trust leads to better engagement in training sessions.
This emotional shift is essential for long-term progress.
Education and Training for Safe Use
Teaching Basic Wear and Care Instructions
Patients are often unaware of how much daily care a prosthesis needs. Doctors help them understand the importance of keeping the socket clean and the skin dry.
Simple routines prevent infections and irritation. These routines also ensure the device lasts longer and performs better.
Clear instruction now avoids problems later.
Explaining Proper Wearing Schedules
New users should not wear the prosthesis all day at once. Doctors guide them through a gradual schedule, starting with short periods and slowly increasing duration.
This approach helps the skin adapt. If they rush this stage, they may develop blisters or soreness.
A slow and structured schedule creates long-term comfort.
Training the Patient in Donning and Doffing
Patients need to learn how to put on and remove the prosthesis correctly. Doctors help reinforce what the prosthetic team teaches.
When patients practice these actions safely, they feel more independent. Clear training reduces mistakes that could damage the device or injure the skin.
This early confidence leads to smoother mobility training later.
Encouraging Consistent Socket Checks
Patients must check their limb daily for redness, cuts, or swelling. Doctors teach them how to observe these early signs.
Small issues become big problems if ignored. Daily checks allow patients to prevent setbacks and keep the fitting comfortable.
This habit supports long-term success with the prosthesis.
Prosthetic Gait Training
Introducing the Patient to Basic Standing Techniques
Standing with a prosthesis feels very different from standing naturally. Doctors prepare patients by explaining how balance shifts and where to place their weight.
A calm introduction helps patients feel less nervous. When they understand the concept, they respond better to the physiotherapist’s instructions.
This early guidance reduces fear and improves stability.
Helping the Patient Practice Controlled Weight Shifts
Weight shifting is the foundation of walking. Patients must learn how to shift weight safely without losing balance.
Doctors reinforce this skill by explaining why it matters. Controlled weight shifts help prevent falls and improve gait mechanics.
Small steps here create strong progress later.
Progressing Toward Step Training
Once weight shifting is steady, patients begin taking small steps. Doctors remind them to stay patient, as these early steps feel unnatural.
With consistent practice and calm guidance, confidence grows. Their gait becomes smoother, and their walking pattern improves.
Progress at this stage sets the rhythm for more advanced training.
Encouraging Patients Through Slow Progress
Gait training takes time. Doctors help patients stay motivated when progress feels slow.
Simple reassurance reminds them that every improvement counts. Encouragement from a medical professional carries great emotional weight.
Motivated patients stay committed and achieve better outcomes.
Evaluating Prosthetic Fit Over Time
Watching for Signs of Limb Volume Change
Residual limb volume continues to change for months. Doctors help track these changes during follow-up visits.
If the limb becomes smaller, the socket may feel loose. Early detection prevents instability and skin problems.
Regular checks help keep the prosthesis safe and comfortable.
Checking for Discomfort During Daily Tasks
Patients may feel fine during basic walking but discomfort during long walks or uneven terrain. Doctors ask targeted questions to find specific issues.
These insights help the prosthetic team adjust alignment or padding. This ensures comfort during all daily tasks, not just clinic visits.
Complete comfort supports long-term use.
Reviewing the Patient’s Mobility Achievements
As patients regain confidence, their mobility improves. Doctors review their progress and compare it with earlier goals.
If progress seems slow, small changes in therapy or prosthetic settings may help. Regular review keeps the patient moving forward.
Every improvement adds to their independence.
Discussing When an Upgrade Might Be Needed
Over time, patients may outgrow their first prosthesis. Their mobility may increase, or their goals may evolve.
Doctors help identify when it is time for more advanced components. These upgrades improve efficiency, stability, and comfort.
A timely upgrade supports continued physical and emotional growth.
Long-Term Rehabilitation and Strength Building
Supporting Core Strength for Better Balance

A strong core helps patients maintain balance while walking with a prosthesis. Doctors encourage simple core exercises that match the patient’s ability. These movements help them stay steady and reduce the chances of falls.
Many patients underestimate how important the core is for walking. When doctors explain this connection in simple words, patients take core training more seriously. This leads to smoother gait patterns and safer daily movement.
Core strength also supports long-term stability, especially when patients begin using more advanced prosthetic components.
Strengthening Hip and Upper Body Muscles
After amputation, hip muscles often weaken because the patient avoids movement at first. Doctors guide them toward exercises that help restore power in this area.
Strong hip muscles make it easier to lift and swing the prosthetic leg. This improves step length, balance, and control. It also reduces strain on the lower back.
Upper body strength also matters. Patients use their arms for support when getting up, sitting down, or adjusting their balance. Simple strength training helps them manage daily tasks more independently.
Encouraging Safe Walking on Different Surfaces
Patients often practice walking only on flat indoor surfaces. But life outside requires them to walk on slopes, rough paths, and uneven areas. Doctors remind them that training on different surfaces builds real-world confidence.
Guided practice under supervision helps the patient learn how to place their feet, shift weight, and react to sudden changes. These skills protect them from falls and help them adapt to any environment.
This training phase is important for long-term safety and independence.
Helping Patients Establish a Daily Exercise Routine
Doctors can help patients create a simple daily routine that fits their schedule. Even five minutes of stretching or mobility training can help maintain progress.
When a routine becomes a habit, patients retain strength, flexibility, and balance. This consistency also prevents long-term complications like joint stiffness or muscle imbalance.
Patients who follow a regular routine enjoy smoother movement and better comfort with their prosthesis.
Follow-Up Appointments and Monitoring
Scheduling Regular Check-Ins
Regular follow-up visits help track progress and catch problems early. Doctors guide patients on how often they need to come back based on their healing, mobility level, and medical condition.
These visits build a long-term partnership between the doctor and patient. Patients feel supported and know they have a safe place to discuss concerns.
Timely check-ins improve safety and help maintain comfort with the prosthesis.
Reviewing Skin Condition During Each Visit
Skin irritation is common among new prosthetic users. Doctors look for redness, dryness, or small cuts during follow-up appointments.
Early detection prevents infections and serious issues. Many patients assume skin problems are normal, so they may not report them unless asked directly.
A quick skin check during each visit protects the patient and improves their overall comfort.
Tracking the Patient’s Mobility Progress
Doctors listen to how the patient feels during walking, standing, and daily tasks. They also observe posture, balance, and step pattern.
If mobility is improving, the rehabilitation plan continues as expected. If progress slows, adjustments may be needed in the prosthesis or therapy plan.
This ongoing tracking helps the patient reach their maximum potential.
Addressing New Pain or Discomfort
Pain that appears suddenly must be taken seriously. Doctors help identify whether it comes from the socket, alignment, or other medical issues.
Prompt action prevents worsening discomfort and protects the patient from developing bad walking habits.
A careful approach ensures long-term comfort and safety.
Supporting Return to Daily Life
Helping the Patient Restart Household Activities
Simple tasks like cooking or cleaning can feel challenging after amputation. Doctors guide patients on how to approach these tasks slowly and safely.
Breaking activities into smaller steps helps reduce fear and build confidence. With time, patients learn new ways to manage their routine without overloading their prosthetic limb.
Small wins at home build emotional strength and independence.
Advising on Safe Return to Work
Returning to work is a major step in the patient’s recovery journey. Doctors help evaluate whether their workplace is safe and what modifications may be needed.
Some jobs require long hours of standing, while others need frequent movement. Doctors guide patients on how to pace themselves and avoid strain.
A safe return to work increases confidence and improves overall life satisfaction.
Preparing the Patient for Social Settings
Patients may feel self-conscious when they first return to social events. Doctors can guide them on how to handle questions or attention from others.
Encouraging them to take small steps into social life helps reduce anxiety. When they feel comfortable in public, their emotional well-being improves.
Social confidence is a strong part of the rehabilitation process.
Supporting Patients Who Want to Resume Sports
Some patients aim to return to sports or physical hobbies. Doctors assess their ability and guide them on when to start.
If needed, they can recommend specialty prosthetic options designed for running, swimming, or other activities. This helps the patient stay active safely.
Returning to sports gives many amputees a renewed sense of freedom.
Handling Challenges During the Referral Pathway
Addressing Slow Healing
Some wounds heal slowly due to diabetes, circulation issues, or infections. Doctors monitor the wound closely and adjust care plans when needed.
Clear communication helps patients stay calm. When patients understand the reason for delays, they remain engaged in their care.
Slow healing does not stop progress; it just changes the timeline.
Assisting Patients Who Fear Using the Prosthesis
Fear is common, especially during early training. Doctors help by explaining each step clearly and encouraging the patient’s efforts.
Small practice goals help build confidence. With time, patients learn that the prosthesis supports them safely.
Reassurance from a doctor has a strong impact on their courage.
Managing Socket Discomfort
Socket discomfort is one of the most frequent early challenges. Doctors ask specific questions about where and when discomfort occurs.
This helps the prosthetist make the right adjustments. Quick corrections keep the patient motivated and avoid long breaks in training.
Comfort is the key to successful long-term use.
Supporting Overweight or Medically Complex Patients
Some patients need extra support due to weight, heart conditions, or other health issues. Doctors help tailor the rehabilitation plan to their needs.
Simple exercises and gradual activity help them progress safely. A customized approach keeps them moving forward without pushing too hard.
With the right guidance, these patients also achieve strong outcomes.
Educating Family Members and Caregivers
Teaching Safe Assistance Techniques

Family members often help with daily tasks. Doctors guide them on safe ways to support the patient without causing strain.
Teaching them proper lifting or support techniques prevents injuries for both the patient and the caregiver. Clear instructions make daily life smoother.
Caregiver education supports long-term independence.
Encouraging Emotional Support at Home
Patients rely heavily on their family for emotional strength. Doctors can gently remind families to offer patience, encouragement, and understanding.
These small acts make a big difference. They help the patient feel loved and supported during tough moments.
A strong support system boosts recovery.
Preparing Families for Slow Progress Phases
Rehabilitation is not always steady. There will be days of slow progress or setbacks. Doctors help families understand that this is normal.
When families know what to expect, they avoid creating pressure or frustration. This protects the patient’s confidence.
Realistic expectations improve home support.
Teaching Families About Prosthetic Care
Caregivers sometimes assist with cleaning or adjusting the prosthesis. Doctors explain the basics so they can help safely.
When families know how to check for wear and tear, small issues are identified early. This prevents device damage and discomfort.
Educated families make the journey smoother for everyone.
Choosing When to Replace or Upgrade the Prosthesis
Identifying Signs of Socket Wear
Over time, sockets become loose due to limb shape changes. Doctors help identify signs such as slipping, rotation, or pressure marks.
These early warnings help the patient get timely adjustments. A worn socket can affect walking and cause injury if ignored.
Detecting wear early protects mobility and comfort.
Monitoring Wear on Foot or Knee Components
Prosthetic feet, knees, and joints also wear out with use. Doctors listen to the patient’s feedback about clicking sounds, instability, or reduced control.
These signs help decide when a replacement is needed. Worn components increase the risk of falls.
Regular monitoring ensures long-term safety.
Evaluating the Patient’s Changing Lifestyle
Patients evolve over time. Some become more active, while others shift to new routines. Doctors help assess whether their current prosthesis still matches their lifestyle.
If their needs have changed, an upgrade may improve movement, safety, and comfort.
The right upgrade keeps the patient progressing.
Planning for Pediatric Prosthetic Changes
Children outgrow their prosthesis frequently. Doctors track their growth and mobility needs to plan timely replacements.
Early planning prevents delays and supports healthy development.
Regular updates keep children active and confident.
Coordinating With Multidisciplinary Teams
Working Closely With Physiotherapists
Physiotherapists play a major role in helping patients learn how to walk and move with their prosthesis. Doctors coordinate with them to ensure the therapy plan matches the patient’s medical condition and healing stage.
This teamwork creates consistency in instructions. When everyone follows the same plan, the patient progresses faster and feels more supported.
Regular updates between the doctor and physiotherapist also help catch issues early, such as weakness, balance problems, or gait deviations.
Communicating With Occupational Therapists
Occupational therapists help patients return to everyday tasks like dressing, bathing, and cooking. Doctors support their work by sharing medical restrictions or special concerns.
When therapists understand these limits, they design safer routines. The patient learns how to manage tasks at home and work without overloading their limb.
This collaboration makes daily life easier and reduces stress for the patient.
Involving Psychologists or Counselors When Needed
Some patients struggle with body image, anxiety, or emotional distress after amputation. Doctors identify when psychological support might help.
Early involvement of mental health professionals creates a smoother transition through the prosthetic process. Patients learn coping skills and feel more confident facing challenges.
A stable emotional state improves participation in rehabilitation.
Coordinating With Dietitians for Overall Health
Nutrition affects healing, weight control, and energy levels. Dietitians help patients maintain a balanced diet that supports muscle recovery and stable body weight.
Doctors share health insights, such as diabetes control or cardiovascular concerns. This helps the dietitian create a safer and targeted nutrition plan.
Healthy patients adapt more easily to prosthetic use.
Preventing Long-Term Complications
Protecting Joint Health During Gait Training
Improper walking patterns can harm the hips, knees, and back. Doctors monitor joints closely during follow-up visits.
If unusual stress patterns appear, adjustments to alignment or therapy may be needed. Correcting these early prevents long-term pain and mobility issues.
Healthy joints support long-lasting independence.
Managing Phantom Limb Sensations
Phantom sensations are common and can be confusing for patients. Doctors explain the difference between normal sensations and concerning pain.
Simple techniques like massage, heat therapy, or mirror therapy may help reduce discomfort. When addressed early, phantom pain becomes less disruptive.
This improves the patient’s confidence and comfort with their prosthesis.
Preventing Residual Limb Skin Breakdown
Skin breakdown occurs when pressure, friction, or sweat affects sensitive areas. Doctors help prevent this by teaching patients proper skin care and advising on correct prosthesis use.
Regular checks help catch small issues before they become serious. Dry skin, redness, or swelling should never be ignored.
Good skin health ensures consistent prosthetic use.
Avoiding Muscle Imbalance Over Time
Patients sometimes favor one side of the body after amputation. This creates imbalances that can lead to pain or limited mobility.
Doctors guide corrective exercises and posture monitoring. Strengthening the weaker areas helps restore symmetry.
Balanced muscles improve gait quality and prevent injury.
Guiding Patients Through Lifestyle Changes
Helping Patients Develop Healthy Walking Habits
Many new prosthetic users develop unusual walking habits without realizing it. Doctors guide them on proper foot placement, step length, and weight distribution.
These habits must be reinforced daily. When taught early, they prevent long-term problems and support a natural gait.
Stable walking habits also boost confidence.
Advising on Footwear Choices
Footwear affects balance and comfort. Doctors help patients choose shoes that provide good support, even weight distribution, and safe grip.
Simple changes in footwear can reduce strain on the residual limb and improve walking comfort. It also prevents falls and reduces joint pressure.
Good footwear choices protect the prosthetic components as well.
Supporting Healthy Weight Management
Weight gain adds extra strain on the prosthesis and joints. Doctors guide patients on maintaining a healthy weight through balanced eating and safe exercise.
Even small weight changes can affect socket fit. Addressing this early keeps the prosthesis comfortable and effective.
Healthy weight also improves energy levels and mobility.
Encouraging an Active Lifestyle
Activity helps maintain strength, flexibility, and cardiovascular health. Doctors motivate patients to stay active with safe and simple routines.
Walking, light stretching, and low-impact exercise help maintain stability. Over time, patients gain more confidence and feel more independent.
Activity is a key part of long-term success.
training Patients to Identify Problems Early
Encouraging Awareness of Pressure Points
Patients must learn to notice early signs of pressure issues. Doctors explain the difference between normal pressure and harmful discomfort.
Early awareness helps prevent skin damage and socket complications. Small adjustments at the right time protect long-term comfort.
This skill helps patients manage their prosthesis with confidence.
Teaching Patients to Spot Alignment Problems
Alignment issues can develop slowly. Patients may feel uneven steps, tilting, or unusual strain during walking.
Doctors teach patients to report these signs immediately. Early adjustments reduce the risk of falls and joint problems.
Timely action ensures safer mobility.
Explaining How to Monitor Component Wear
Prosthetic components like feet, joints, and liners wear down with use. Patients should learn how to observe small changes like reduced cushioning or unusual noises.
Doctors teach them what to watch for and when to return for maintenance. This prevents sudden failures or unsafe walking.
Regular checks protect the device and the patient.
Guiding Patients on When to Seek Help
Some patients hesitate to report issues. Doctors encourage them to seek help whenever something feels wrong.
Clear communication prevents problems from becoming serious. With timely guidance, the patient feels supported and safe.
Early help improves long-term success.
Caring for Pediatric Amputee Patients
Monitoring Growth and Limb Changes
Children’s bodies change quickly. Doctors track growth patterns to ensure the prosthesis stays safe and functional.
Frequent check-ins help identify when a new socket or limb length adjustment is needed. Children adapt well when changes occur at the right time.
Active monitoring supports healthy development.
Supporting Children Emotionally
Children may feel confused or scared after amputation. Doctors provide gentle reassurance and simple explanations that help them feel safe.
Emotional support helps them participate confidently in therapy and school activities. It also reduces fear during prosthetic fittings.
A calm child learns faster and adapts more easily.
Training Parents on Daily Care
Parents play the main role in a child’s prosthetic care. Doctors teach them how to clean the device, monitor skin health, and watch for alignment issues.
These skills help parents protect their child from discomfort or injury. Confident caregivers create a stable environment for recovery.
Families become strong partners in rehabilitation.
Encouraging Safe Play and Activities
Children want to play and explore. Doctors help parents choose safe activities that support physical development without harming the prosthesis.
Active play builds strength, coordination, and confidence. It also helps the child accept the prosthesis as part of daily life.
Encouraging movement helps children grow without fear.
Reinforcing Long-Term Independence
Teaching Patients How to Plan Their Day Safely
Patients learn to organize their day around safe movement, rest periods, and exercise. Doctors guide them on balancing activity with care.
Planning ahead prevents strain and keeps the prosthesis comfortable throughout the day. It also improves confidence in daily routines.
Good planning supports long-term independence.
Encouraging Self-Management of Prosthetic Care
Doctors help patients feel responsible for their prosthesis. Teaching them simple maintenance routines builds independence.
When patients handle daily cleaning, skin checks, and wearing schedules confidently, they rely less on others. This improves emotional well-being and improves engagement in care.
Self-management is a major milestone in recovery.
Supporting Long-Term Goal Setting
Patients often reach a point where they want to do more—walk longer, exercise, or return to hobbies. Doctors help them set realistic long-term goals.
These goals keep patients motivated and give them a sense of direction. Progress becomes steady and meaningful.
Goal setting transforms rehabilitation into a hopeful journey.
Reminding Patients to Celebrate Progress
Recovery takes time, and progress is sometimes slow. Doctors remind patients to appreciate every improvement, no matter how small.
These reminders help them stay positive. A hopeful mindset plays a major role in long-term success with a prosthesis.
Positive reinforcement strengthens confidence.
Supporting Amputees in Rural and Semi-Urban Settings
Understanding Access Challenges

Patients in rural and semi-urban areas often face long travel distances to reach prosthetic centers. Doctors help by planning referrals in a way that reduces travel frequency.
A clear schedule for fittings, follow-ups, and therapy helps families organize transportation. This planning prevents missed appointments and delays in care.
Understanding these challenges allows doctors to tailor treatment plans that fit the patient’s reality.
Offering Clear Home Care Guidelines
When distance is a problem, home care becomes even more important. Doctors give simple, written instructions on limb care, skin checks, and wearing schedules.
These guidelines help families manage daily care without professional supervision. Clear instructions prevent mistakes and protect the patient’s progress.
Strong home care support reduces complications.
Coordinating With Local Health Workers
Local health workers often know the patient’s environment well. Doctors can guide them on basic follow-up checks like observing skin condition or monitoring wound healing.
This local support helps catch problems early. It also reduces the pressure on the patient to travel frequently.
Collaboration with local workers strengthens the rehabilitation pathway.
Helping Families Understand the Prosthetic Timeline
Families in rural areas may have limited exposure to prosthetic care. Doctors explain the timeline in simple terms so they know what to expect at each step.
When families understand the timeline, they feel less stressed and more prepared for each visit or adjustment.
Proper awareness keeps the process smooth and organized.
Cultural Sensitivity in Prosthetic Referral
Respecting Beliefs Around Amputation
Different communities have different beliefs about amputation. Some may see it with fear, while others may see it as a sign of weakness.
Doctors approach these beliefs with patience and respect. By explaining the medical reasons in simple words, they help families understand that amputation is a step toward healing.
Respect for cultural beliefs builds trust and cooperation.
Communicating in Local Languages When Possible
Clear communication is essential. Patients feel more supported when instructions are shared in a language they understand well.
Doctors who adapt their words to the patient’s language make the experience less intimidating. This improves cooperation and helps families follow instructions correctly.
Language support creates a more comfortable environment.
Guiding Families With Sensitivity
Some families may feel overwhelmed by the idea of a prosthesis. Doctors guide them gently, addressing concerns without judgment.
A respectful approach keeps them engaged and open to learning. It also reduces emotional barriers that may slow rehabilitation.
Cultural understanding strengthens the doctor-patient relationship.
Encouraging Support From Community Networks
In many communities, extended family or neighbors play a strong support role. Doctors suggest ways to involve these networks when needed.
Community help may assist with travel, emotional support, or daily tasks. This shared support eases the patient’s transition into prosthetic use.
Community strength enhances rehabilitation success.
Building Confidence Through Peer Support
Introducing Patients to Support Groups
Meeting others who have gone through amputation can be life-changing. Doctors guide patients toward support groups or meetings when available.
Hearing real stories from others helps reduce fear. It also gives patients a sense of belonging and hope.
Peer guidance adds a powerful emotional boost.
Encouraging Interaction With Experienced Users
Seeing someone walk confidently with a prosthesis inspires new users. Doctors may connect patients with experienced amputees who can offer practical advice.
These informal conversations make the journey feel more reachable. They also prepare the patient for challenges in a realistic but hopeful way.
Peer interactions create strong motivation.
Supporting Family Members Through Peer Networks
Families also benefit from meeting others who have supported an amputee. They learn how to help without overdoing it and hear tips that reduce stress.
Doctors encourage this connection when families feel overwhelmed or confused about the process.
Strong family support is essential for long-term success.
Reducing Isolation Through Community Engagement
Isolation can slow emotional healing. Doctors encourage patients to stay connected with friends, community events, or group activities.
Social connection makes patients feel valued and active. These interactions protect their emotional well-being and boost confidence during rehabilitation.
A connected patient is a motivated patient.
Ensuring Safety in Daily Activities
Teaching Safe Use of Stairs
Stair use requires proper technique to avoid falls. Doctors explain how to balance weight and move step-by-step with the prosthesis.
Patients begin with support and gradually build independence. Knowing the right method reduces fear and improves safety.
Mastering stairs is an important milestone.
Guiding Safe Sitting and Standing
Transitions between sitting and standing can feel challenging. Doctors show patients how to position their foot, lean forward safely, and use their hands for support.
Practicing these movements helps prevent imbalance. Smooth transitions also reduce strain on the residual limb.
Safe movement builds daily confidence.
Advising on Safe Bathing and Changing Clothes
Wet floors or sudden movements can be risky. Doctors teach patients how to manage these activities carefully.
Simple tips like using a chair during bathing or dressing sitting down protect the patient from slips and injuries. These small strategies make a big difference.
Daily routines become easier and safer with proper guidance.
Helping Patients Manage Outdoor Movement
Outdoor environments are unpredictable. Doctors guide patients on walking safely on gravel, grass, slopes, or uneven pathways.
Practicing these conditions helps the patient prepare for real-life situations. Over time, they learn how to react safely and stay balanced.
Safe outdoor movement increases independence.
Travel and Transportation With a Prosthesis
Advising on Long-Distance Travel

Long journeys can cause swelling or discomfort. Doctors guide patients on taking breaks, stretching the residual limb, and adjusting the prosthesis during travel.
This prevents stiffness and improves comfort. Simple planning makes long trips much easier.
With the right steps, patients can travel safely and confidently.
Teaching Safe Car Entry and Exit
Getting in and out of a car requires careful balance. Doctors explain how to turn, sit, and lift the legs without strain.
Practicing this movement helps prevent falls and protects the socket fit. Patients gain independence in their daily travel.
Safe car movement boosts confidence.
Guiding Airport or Train Travel Comfortably
Some patients feel unsure about handling long waits, crowds, and security checks. Doctors explain how to manage swelling, adjust liners, or rest when needed.
These tips reduce anxiety and prepare the patient for smoother travel.
A confident traveler feels more independent.
Preparing for Unexpected Delays or Long Walks
Delays can force patients to walk long distances or stand for extended periods. Doctors teach them how to pace themselves and stay alert to discomfort.
Planning ahead helps them stay safe even in unpredictable situations.
Good preparation ensures safer travel.
Technology and Digital Tools in the Referral Pathway
Using Digital Measurements for Accuracy
Many centers now use digital scanners instead of plaster for casting. Doctors help patients understand that these tools make the process faster and more accurate.
Digital scans capture fine details of the limb, leading to a better socket fit. This reduces the number of adjustments needed later.
Technology improves patient comfort and efficiency.
Sharing Referral Information Electronically
Electronic records make communication faster and clearer. Doctors send medical history, images, and wound details directly to the prosthetic team.
This reduces delays and avoids missing information. It also allows the prosthetist to prepare before the patient arrives.
Digital coordination improves the care experience.
Supporting Telehealth for Follow-Up
Some patients cannot travel for every visit. Doctors use telehealth for simple follow-ups, skin checks, or questions about wearing schedules.
This saves time and prevents unnecessary trips. Telehealth also helps doctors track progress more closely.
Remote support helps patients stay consistent in their care.
Introducing Apps for Exercise and Daily Tracking
Many apps provide exercise guidance, reminders, and daily tracking tools. Doctors can recommend simple apps that help patients follow routines.
These tools reinforce good habits and make care more engaging. Patients feel more involved in their own progress.
Technology strengthens self-management.
Preparing Patients for Long-Term Goals
Helping Them Visualize Future Possibilities
Doctors help patients imagine what they will be able to do months or years later. This gives them hope and a sense of direction.
Seeing the bigger picture keeps them motivated during slow phases. With a clear vision, patients work steadily toward long-term independence.
A positive outlook supports continuous progress.
Setting Milestones for Physical Ability
Milestones make progress measurable. Doctors help patients set achievable goals like walking a certain distance, climbing stairs safely, or standing for longer periods.
Reaching each milestone builds confidence. Small wins add up and lead to strong long-term outcomes.
Milestones keep rehabilitation focused.
Encouraging Return to Community Participation
Community engagement boosts emotional strength. Doctors guide patients on rejoining local groups, events, or work activities at a comfortable pace.
This helps them rebuild identity and confidence. Being active in the community reduces isolation.
Social participation enhances quality of life.
Supporting Dreams of Sports or Specialized Activities
Some patients dream of running, cycling, hiking, or swimming again. Doctors assess feasibility and guide them toward the right prosthetic solutions.
Supporting these dreams shows patients that life after amputation can still be full of achievement.
Encouraged patients push themselves to grow.
Conclusion
Bringing Every Step Together
A smooth prosthetic referral pathway gives amputee patients clarity, confidence, and real hope. Doctors guide each stage, from early healing to long-term independence. This guidance helps the patient understand what is happening, why it is happening, and how each decision supports their future mobility.
When every step is explained in simple, calm words, the patient feels safe. They trust the process and stay engaged in their care. This trust becomes the foundation for strong rehabilitation outcomes.
The pathway works best when doctors, prosthetists, therapists, counselors, and families communicate openly. Each person plays a unique role. When these roles connect, the journey becomes far less overwhelming for the patient.
Empowering Patients With Knowledge
Education is one of the strongest tools in this journey. Patients who understand socket care, skin health, exercise routines, and warning signs become confident users. With the right knowledge, they manage challenges early and avoid serious complications.
Good guidance also reduces fear. When patients know what to expect, they stay motivated even during slow phases. This emotional stability helps them progress steadily.
Creating a Clear Roadmap for the Future
A clear referral pathway is not just a medical process. It is a roadmap that helps amputees rebuild their lives. With proper timing, strong support, and structured training, they regain independence and learn to trust their prosthesis as part of everyday life.
Each step in the pathway contributes to a future where the patient moves freely, participates fully in society, and feels in control again. This is the goal of every doctor who supports an amputee patient.