Every amputation tells a different story.
Some happen in seconds—after a road accident, industrial injury, or sudden trauma.
Others happen slowly, as circulation weakens over months or years due to diabetes or vascular disease.
For physicians, these two stories—traumatic and dysvascular—demand completely different rhythms of care.
The pace of healing, the strength of tissue, and even the patient’s mental state all follow separate timelines.
And nowhere is this difference more critical than when deciding when to prescribe the first prosthesis.
Early prosthetic prescription is both an opportunity and a responsibility.
Done at the right time, it restores independence, prevents muscle loss, and builds confidence.
Done too soon, it risks complications, wound breakdown, and emotional frustration.
This article explores how doctors can use structured timing algorithms to determine readiness for prosthetic fitting—specifically comparing trauma-related and dysvascular amputations.
It’s written as a guide to help clinicians balance urgency with safety, science with empathy, and speed with stability.
Because in the world of prosthetics, timing isn’t just medical—it’s transformational.
Understanding the Biological Difference Between Trauma and Dysvascular Amputation
The Nature of Trauma Amputation

A traumatic amputation is sudden.
The body doesn’t have time to prepare for it.
Tissues that were healthy a moment before are abruptly damaged by force, crush, or avulsion.
In these cases, blood supply and muscle tone are often intact in the remaining limb.
Once the wound is cleaned, stabilized, and closed, the body’s natural healing process begins quickly.
Patients tend to be younger and healthier, which supports faster recovery.
The biggest challenge here is managing soft tissue trauma and infection risk.
If debridement is complete and vascular flow is adequate, wound healing can progress steadily.
This allows for early planning of prosthetic fitting, sometimes within weeks.
The Nature of Dysvascular Amputation
Dysvascular amputations are entirely different.
They don’t happen suddenly—they are the end stage of chronic disease.
Long-standing diabetes, peripheral artery disease, or infection leads to progressive tissue death.
The limb is often compromised before surgery even begins.
The surrounding skin, muscle, and vessels may already have poor perfusion.
Even after amputation, the residual limb can take much longer to stabilize and heal.
Patients with dysvascular causes are typically older and have multiple comorbidities.
Healing is slow, and even minor pressure can reopen the wound.
This means prosthetic clearance must be deliberate and timed with precision.
Biological Contrasts That Shape Recovery
In trauma, tissues are injured but capable of robust repair.
In dysvascular cases, tissues are weak, fragile, and prone to re-injury.
That’s why identical surgical outcomes can have entirely different rehabilitation timelines.
Trauma patients benefit from early mobilization, while dysvascular patients require protective observation.
The difference lies in cellular energy, oxygen delivery, and immune response—all slower in chronic vascular conditions.
For physicians, understanding this biological divide is essential before applying any timing algorithm for prosthetic prescription.
Wound Healing Dynamics and Its Impact on Prosthetic Readiness
The Healing Curve in Trauma Patients
In trauma-related amputations, wound healing follows a predictable curve.
Inflammation subsides within the first few days, followed by rapid granulation and epithelialization.
If there’s no infection or skin tension, sutures can be removed by week three or four.
Healthy circulation accelerates tissue repair.
The stump typically shows good color, firm texture, and early shrinkage—all signs that compression can begin.
This quick recovery opens the door for early prosthetic preparation.
By week six to eight, most trauma patients can tolerate shaping and early socket trials.
With supportive rehabilitation, they may begin limited prosthetic use soon after.
The Healing Curve in Dysvascular Patients
In dysvascular amputees, the healing process is far slower and more unpredictable.
Even when the wound appears closed, microcirculation beneath the surface may still be compromised.
Tissues remain fragile and prone to breakdown under mechanical stress.
Healing may stretch over eight to twelve weeks or longer.
Fluctuations in blood sugar, poor nutrition, or mild infections can cause setbacks.
These patients require repeated wound inspections before any compression or socket testing.
It’s not just about time—it’s about tissue quality.
A limb that looks healed must also feel warm, flexible, and pain-free before being considered prosthetic-ready.
Role of Circulatory Support in Healing
Vascular sufficiency determines how soon a limb can bear weight or compression.
Trauma patients usually have intact arteries, so circulation supports rapid closure.
Dysvascular patients, however, often depend on collateral flow or surgical grafts.
Physicians should use Doppler assessment or transcutaneous oxygen measurement to confirm readiness.
A residual limb with consistent warmth and normal capillary refill indicates safe perfusion.
This evaluation ensures that early prosthetic use does not compromise fragile healing.
Designing Timing Algorithms for Early Prosthetic Prescription
Why Timing Algorithms Matter
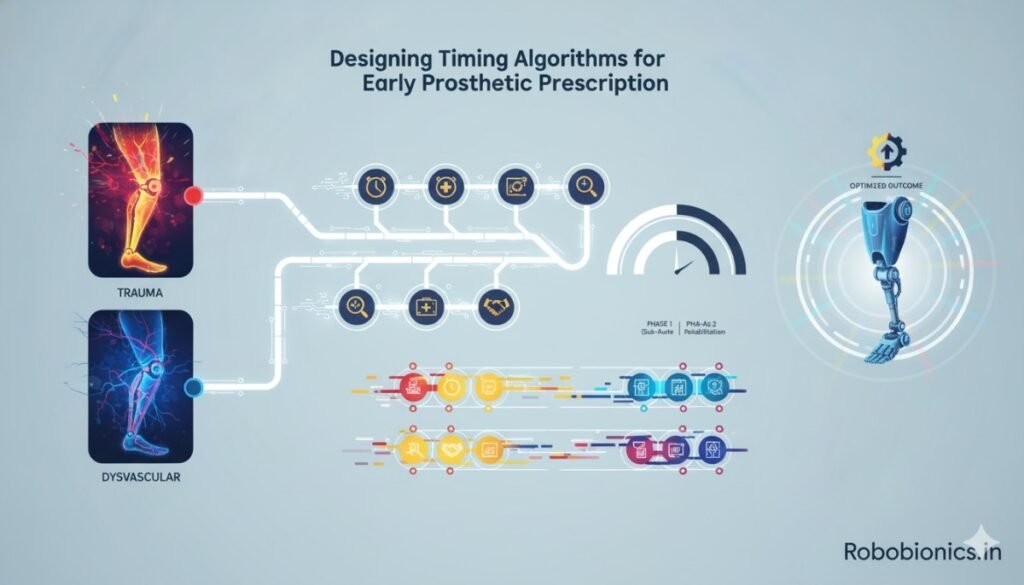
Prosthetic readiness is not just about the calendar—it’s about patterns.
Every patient’s healing follows measurable biological milestones.
Timing algorithms help physicians recognize these markers and make evidence-based decisions.
They also minimize the risk of over- or under-prescription.
By structuring decisions around objective criteria, doctors can plan rehabilitation with confidence.
For trauma and dysvascular cases, separate timing tracks ensure personalized care.
The Trauma Pathway Algorithm
The trauma pathway begins almost immediately after surgery.
Because circulation is stable, wound protection and compression can start early.
Day 0–7: Focus on infection control and gentle dressing changes.
Week 2–4: Begin light compression once the incision is dry and stable.
Week 5–6: Introduce shaping and mild weight-bearing under supervision.
Week 7–10: Conduct the first prosthetic casting or trial socket fitting.
This structured progression helps maintain muscle tone, reduce edema, and sustain motivation.
The overall goal is to ensure prosthetic introduction while the body and mind are still responsive.
The Dysvascular Pathway Algorithm
The dysvascular timeline follows a slower, more cautious curve.
Here, the physician’s focus is on systemic optimization before local intervention.
Day 0–14: Prioritize wound protection, glycemic control, and infection prevention.
Week 3–6: Begin gentle compression if perfusion and tissue color are stable.
Week 7–10: Introduce light desensitization and residual limb massage.
Week 10–14: Consider prosthetic evaluation only when circulation, skin, and systemic health align.
This slower pace prevents setbacks and builds lasting readiness.
In many cases, the first prosthetic fitting happens around the 12th to 16th week post-operation.
Using Flexible Algorithms
No algorithm replaces clinical judgment.
Each patient’s healing path depends on nutrition, activity, and emotional readiness.
Physicians must adapt these timelines based on weekly assessments.
Timing should never be rushed for convenience or delayed out of fear.
A flexible, evidence-based algorithm provides structure without rigidity.
By combining objective measures with intuition, physicians can optimize both safety and progress.
Edema, Compression, and Residual Limb Shaping
Controlling Swelling in Trauma Patients
In trauma cases, swelling is immediate and often intense.
Compression can begin earlier once drainage stops and the incision is sealed.
Uniform wrapping or early shrinker use helps maintain a smooth, conical limb.
Early edema control shortens the time to prosthetic readiness.
It also prevents redundant soft tissue that can interfere with socket fitting later.
Physicians should monitor capillary refill and skin temperature daily during this phase.
If compression is too tight, circulation may be restricted, causing discomfort or discoloration.
Managing Edema in Dysvascular Amputees
For dysvascular patients, edema management is far more delicate.
Poor venous return and fragile skin mean compression must be extremely gentle.
Overzealous wrapping can worsen ischemia or reopen surgical sites.
Start with mild elastic bandages or adjustable shrinkers only after full wound closure.
In some cases, intermittent pneumatic compression may be safer than static pressure.
Regular vascular assessments ensure that compression supports rather than hinders healing.
The Impact of Limb Shape on Prosthetic Fit
Regardless of cause, a well-shaped limb ensures comfort and stability during prosthetic use.
Conical shaping provides better suspension and load distribution.
Bulbous or irregular limbs lead to friction, sores, and poor control.
For trauma patients, achieving proper shape is straightforward with early bandaging.
For dysvascular patients, shaping is gradual and must align with vascular healing.
Rushing this phase can undo months of progress.
A steady, guided approach results in a limb that not only fits well but also tolerates long-term prosthetic use.
Psychological Readiness and Pain Management
Emotional Patterns in Trauma Amputees

Trauma amputees often face shock and disbelief.
Their amputation is sudden, unexpected, and linked to a specific event.
Pain, fear, and confusion dominate the first few weeks.
However, once healing begins, these patients typically show strong motivation to regain function.
Their bodies are young and responsive, and they crave independence.
Physicians can harness this motivation through early education and goal setting.
Pain management should combine pharmacologic support with movement therapy.
Early mobilization helps reduce both physical pain and emotional distress.
Emotional Patterns in Dysvascular Amputees
For dysvascular amputees, emotions follow a slower, more reflective curve.
Their amputation is often preceded by years of medical decline.
They experience fatigue, resignation, and sometimes guilt over disease progression.
Rehabilitation here depends heavily on trust and reassurance.
These patients need time to believe in recovery again.
Physicians should focus on hope, empathy, and small victories—standing, balance, and first steps.
Psychological readiness often lags behind wound healing, so counseling should begin early.
When emotions align with physical readiness, prosthetic training becomes smoother and more sustainable.
Managing Phantom Pain and Sensation
Phantom pain affects both trauma and dysvascular patients but for different reasons.
In trauma, nerve endings are abruptly severed, leading to hyperactive signaling.
In dysvascular cases, chronic ischemia alters nerve function long before surgery.
Early desensitization, mirror therapy, and mild tactile stimulation can reduce phantom sensations.
Proper stump handling—combined with effective pain control—sets the stage for confident prosthetic use.
Patients who understand phantom sensations as part of healing adjust better emotionally.
This understanding keeps motivation strong and prevents fear from slowing recovery.
Algorithmic Checkpoints for Physician Decision-Making
Establishing Objective Readiness Markers
A structured approach is what separates good rehabilitation from guesswork.
When physicians use measurable checkpoints, decisions about prosthetic readiness become clearer and safer.
These checkpoints act like milestones in recovery—each confirming that both the body and the mind are prepared to move forward.
The first checkpoint is wound stability.
The incision must be dry, sealed, and without local tenderness.
No redness, discharge, or temperature difference should be present around the site.
The second is limb volume stabilization.
In trauma patients, this typically happens around the fourth to sixth week.
In dysvascular patients, it may take up to twelve weeks before consistent circumference measurements are recorded.
Finally, systemic and psychological readiness are assessed together.
Pain control, circulation, and emotional stability must align before any prosthetic evaluation.
These elements together make the limb not just healed—but truly ready.
The Role of Functional Tests
Beyond the clinical markers, functional readiness tells a fuller story.
Ask patients to perform small, safe actions—like sitting balance, gentle weight shifting, or controlled limb movement.
Pain, fatigue, or skin redness during these actions can indicate that readiness is still incomplete.
For trauma amputees, these tests also measure muscle strength and coordination, ensuring they can handle early gait training.
For dysvascular patients, the same tests reveal cardiovascular endurance and postural stability.
Passing functional tests gives a green light for early prosthetic preparation, helping the team move confidently toward fitting.
Interdisciplinary Validation Before Prescription
Before clearance, coordination between the physician, prosthetist, and rehabilitation therapist is essential.
Each professional contributes insight that prevents missteps.
The physician verifies medical and vascular stability.
The prosthetist assesses limb shape, volume, and soft tissue quality.
The therapist evaluates balance, strength, and cognitive engagement.
A shared review meeting—often brief but focused—ensures every detail aligns.
This collaboration creates unified confidence, so the patient receives consistent advice and motivation.
When all three voices agree, prosthetic prescription transitions from theory to safe, actionable practice.
Prosthetic Fitting Milestones in Trauma and Dysvascular Patients
The Early Fit in Trauma Amputees
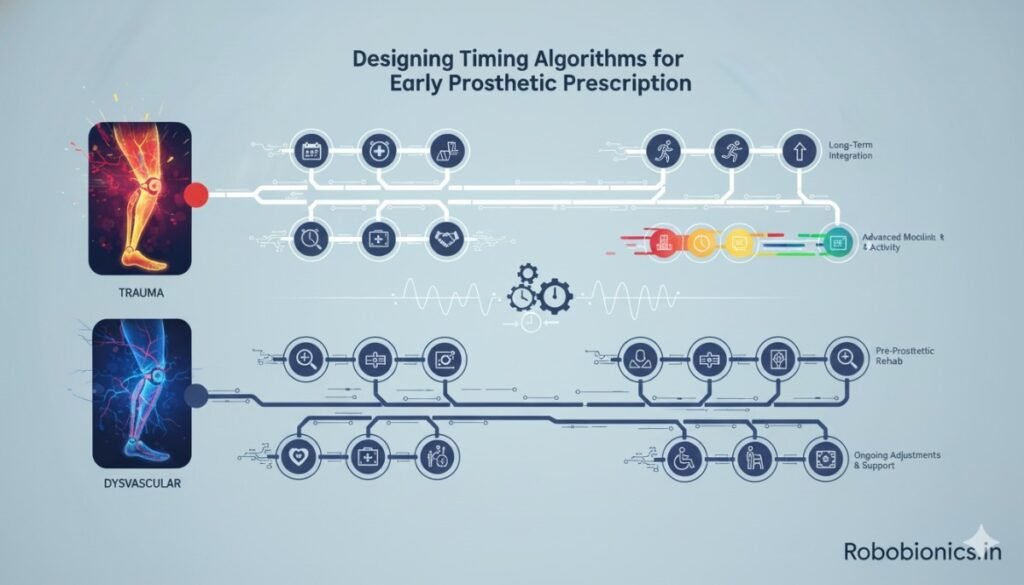
For trauma amputees, early fitting offers immense psychological and physical benefits.
Most patients can begin preparatory prosthetic casting around the sixth to eighth week post-operation, depending on wound health.
The preparatory socket phase introduces the limb to controlled pressure and motion.
It trains the skin to adapt and helps the patient regain proprioceptive feedback.
Since circulation and tissue strength are typically robust, the risk of complications is low.
Early prosthetic use maintains muscle tone and prevents contractures.
It also builds confidence—turning fear into function.
By the twelfth week, many trauma amputees can progress to definitive sockets, with gait training already underway.
The Gradual Fit in Dysvascular Amputees
Dysvascular patients demand a gentler pace.
The residual limb may appear ready, yet still harbor fragile capillaries and slow-healing scar tissue.
Even small abrasions can evolve into ulcers if prosthetic loading begins too soon.
Here, a “soft entry” approach works best.
Start with light contact through silicone liners or temporary sockets that distribute pressure evenly.
Allow short wear intervals at first—fifteen to thirty minutes—before increasing duration based on tolerance.
Prosthetic training should begin only after the patient can tolerate compression without discomfort for at least two weeks.
Patience here leads to long-term comfort and stability.
The Hybrid Timing Model
Between the two extremes lies a growing number of mixed-profile cases.
Patients may survive traumatic events but have underlying vascular disease or diabetes.
For them, neither the trauma nor the dysvascular algorithm fits perfectly.
The hybrid model adapts dynamically to the patient’s daily condition.
It starts with trauma-like momentum but pauses whenever vascular signs or metabolic fluctuations appear.
In this model, flexibility is the rule—guided by clinical markers rather than fixed time frames.
This adaptive system ensures that readiness decisions evolve alongside the patient’s healing capacity.
Comparative Outcomes Between Trauma and Dysvascular Groups
Recovery Trajectories
Trauma amputees generally progress through rehabilitation faster.
Their younger age, intact vascular health, and strong tissue integrity allow early prosthetic adoption.
Many regain near-normal mobility within four to six months of surgery.
Dysvascular patients, on the other hand, move through slower but steadier progressions.
Their primary victories are often smaller—consistent use, safe ambulation, or partial independence—but no less meaningful.
When managed carefully, they still achieve high-quality functional outcomes within ten to twelve months.
Both groups benefit most when timing is tailored, not forced.
The physician’s patience and discernment determine whether progress continues smoothly or stalls due to complications.
Complication Rates and Preventive Patterns
Studies consistently show higher complication rates in dysvascular cases.
Infection, delayed healing, and pressure ulcers occur more frequently due to compromised circulation.
However, when prosthetic introduction follows a structured, algorithmic path, these risks drop dramatically.
In trauma patients, complications are more often mechanical—socket misalignment, overuse injuries, or stump swelling.
Early detection and adjustments typically resolve these quickly.
The preventive pattern is simple: act early in trauma cases and act cautiously in dysvascular ones.
This balance maximizes safety without sacrificing momentum.
Emotional and Behavioral Differences
Emotional recovery in trauma amputees often mirrors their physical recovery—intense, fast, and determined.
They tend to express urgency in wanting to “get back to normal,” which propels rehabilitation forward.
However, physicians must temper this energy with realistic timelines to prevent overexertion.
Dysvascular amputees navigate recovery with a quieter resilience.
Years of chronic illness have already shaped their perspective on patience and adaptation.
Motivational counseling and steady encouragement work better here than aggressive goal-setting.
Recognizing these psychological patterns allows physicians to match prosthetic timelines to each personality, not just the body.
Physician-Led Strategies for Timing Optimization
Integrating Vascular Medicine and Rehabilitation
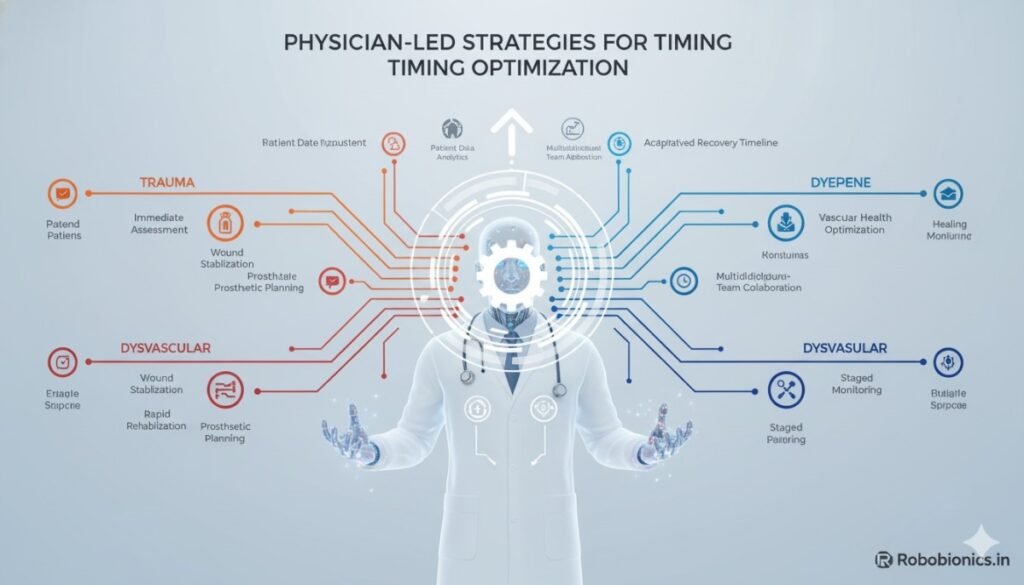
For dysvascular patients, prosthetic readiness starts long before amputation.
When vascular surgeons, endocrinologists, and rehabilitation physicians collaborate early, healing accelerates post-surgery.
Optimizing perfusion and metabolic control preoperatively creates a foundation for smoother recovery.
After amputation, ongoing vascular monitoring ensures that improvements are sustained.
Intermittent Doppler assessments and wound photography provide data-driven reassurance that the limb is ready for the next phase.
Physicians who treat vascular optimization as part of the prosthetic timeline—not as a separate process—achieve faster and safer clearances.
Continuous Patient Education
Patient awareness is a critical determinant of success.
Explain every phase clearly—why certain activities are delayed and what signs indicate readiness.
When patients understand the “why,” compliance improves dramatically.
Teach them to self-check skin temperature, swelling, and color daily.
In both trauma and dysvascular cases, this vigilance prevents setbacks between visits.
An informed patient becomes an active participant rather than a passive recipient of care.
Education should begin during hospitalization and continue through every follow-up.
Repetition reinforces confidence and ensures long-term engagement with rehabilitation goals.
Structured Pain Management and Emotional Support
Pain control directly influences timing.
Uncontrolled pain delays mobilization, disrupts sleep, and impairs motivation.
Early multimodal analgesia—combining medication with relaxation and physiotherapy—shortens the path to prosthetic readiness.
Emotional counseling is equally essential.
Trauma amputees often struggle with sudden identity loss, while dysvascular patients wrestle with long-term fatigue and fear of recurrence.
Regular psychological review ensures these hidden obstacles don’t quietly stall progress.
A pain-free, emotionally balanced patient transitions to prosthetic use far more successfully than one battling unresolved distress.
Long-Term Adaptation and Follow-Up
Monitoring the First Year
The first year post-amputation defines long-term outcomes.
Limb volume changes, socket adjustments, and muscle reconditioning are all dynamic processes.
Physicians should schedule regular reviews every two to four weeks for trauma patients and every two to six weeks for dysvascular patients.
These visits serve not just for physical assessment but also for motivation.
Each appointment reinforces the patient’s sense of progress and accountability.
Minor adjustments—whether to socket fit or compression schedule—prevent major complications later.
Managing Recurrence of Edema or Infection
Swelling or infection can reappear at any stage, especially in dysvascular cases.
Early detection is vital.
Encourage patients to report new warmth, discharge, or discomfort immediately.
If edema recurs, evaluate for underlying systemic triggers such as dehydration, poor diet, or vascular blockage.
Addressing root causes prevents the need to pause prosthetic use unnecessarily.
Proactive management keeps rehabilitation continuous and reduces the risk of regression.
Encouraging Lifelong Use and Independence
Once prosthetic training is complete, long-term engagement ensures sustained mobility.
Physicians should remind patients that consistency—not intensity—maintains independence.
Even short daily use keeps tissues conditioned and psychological well-being intact.
In trauma patients, continued activity supports strength and confidence.
In dysvascular patients, careful pacing preserves endurance without overstraining circulation.
Both groups thrive when follow-ups emphasize empowerment rather than dependency.
When patients see prosthetic use as an extension of themselves, lifelong adaptation becomes natural.
The Physician’s Philosophy in Timing Decisions
Balancing Urgency and Caution
The art of prosthetic timing lies in balancing two instincts: the urge to accelerate recovery and the duty to protect healing.
For trauma patients, urgency often benefits recovery—early action restores function before inertia sets in.
For dysvascular patients, caution preserves tissue and prevents recurrence.
Neither is superior; both are context-driven.
A physician’s intuition, shaped by observation and experience, bridges the science of healing with the humanity of care.
The Power of Hope in Medical Timing
When physicians speak about readiness, patients listen not just for information but for hope.
Timing decisions carry emotional weight—they tell patients when they can move, work, and live again.
Every clearance is both a medical judgment and a psychological milestone.
By framing readiness as progress, not permission, doctors help patients feel capable rather than dependent.
That feeling is the spark that fuels recovery long after the clinic visit ends.
Conclusion

Trauma and dysvascular amputations may share a destination, but their roads are entirely different.
Where trauma calls for early movement, dysvascular recovery demands patience and precision.
The physician’s task is to guide each journey with timing algorithms that honor both biology and human spirit.
Structured, evidence-based timelines reduce complications and accelerate recovery.
But beyond science, empathy and communication shape the true success of early prosthetic prescription.
At Robobionics, we believe in this union of care and innovation.
Our prosthetic systems—like the Grippy™ Bionic Hand and Grippy Mech Series—are engineered to complement a doctor’s timing, ensuring patients experience not just motion, but meaning in every step.
To learn how our clinically tested solutions can enhance your prosthetic rehabilitation protocols, visit www.robobionics.in/bookdemo.
Together, let’s turn timing into transformation—one patient, one step at a time.



