Smart prosthetics are no longer just a dream. They are becoming part of real care in real hospitals. Across India and the world, clinics are beginning to use bionic limbs that not only move with muscle signals but also learn, respond, and even feel.
These changes are not just about better technology. They are about how patients heal, how therapists work, and how clinics grow. This article looks ahead. What will clinics look like when smart prosthetics become the norm? What will patients expect? What should doctors and rehab teams prepare for?
At RoboBionics, we build these devices every day. But more importantly, we work with clinics that are using them in real life. And from what we see, the future is not far—it’s already starting.
Let’s explore what’s coming, and how your clinic or practice can be ready.
The Rise of Smart Prosthetics in Clinics
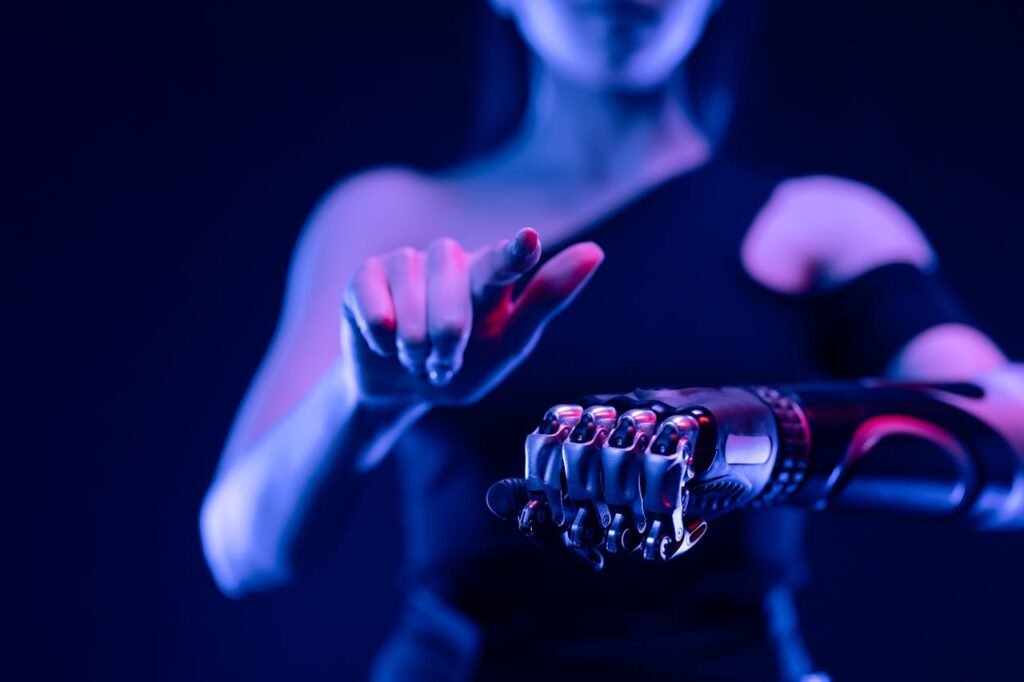
More Than Mechanical Arms

Smart prosthetics like Grippy™ now go beyond simple grab-and-release tools. They sense muscle activity, learn user patterns, and offer feedback like touch or pressure.
In clinical settings, this means the device becomes a learning partner, not just a tool. Therapists can track how the brain connects with the limb over time. They see when the signals get clearer or when control becomes smoother.
This makes therapy more precise and more personal.
Clinics Evolving into Innovation Centers
Today, ordinary clinics are becoming hubs of innovation.
Smart prosthetics have transformed rehab spaces from training areas to data-rich learning zones.
With devices that upload usage patterns and feedback, therapists can observe trends and adjust care. This means more targeted help, faster adaptation, and better use of resources.
Therapists move from guessing to guiding with real insight.
New Roles in the Clinic
The Bionic Therapists
As smart limbs enter clinics, therapists’ roles are expanding.
They are no longer just trainers; they’re coaches who interpret data, educate patients, and guide emotional adaptation.
They help users understand signal noise, adjust sensitivity, and train for feedback. They also help patients emotionally attach to their prosthetic—because that emotional bond speeds neuro-adaptation like nothing else.
Therapists become both technicians and mentors in this new age.
Clinics Need Tech-Savvy Support Staff
Smart prosthetics bring technology—and needs.
Clinics need staff who can handle firmware updates, sensor placement, charging protocols, and troubleshooting.
They don’t need full-scale engineers. But they need team members comfortable with simple settings, signal tests, and user calibration.
This support ensures patients don’t lose time over battery issues or calibration glitches.
Smarter Training, Smarter Outcomes
Data-Driven Practice Plans
Smart limbs provide data on how the device is used—hours of wear, triggers, grip dynamics, and more.
Clinics can use this data to create training plans that are customized and responsive.
Instead of generic rehab modules, therapists can build schedules based on what’s working, what’s not, and what remains challenging.
Progress becomes visible. Therapists and patients see how close they are to real-world tasks – writing, cooking, or walking with balance—and that clarity drives motivation.
Faster Brain-Device Connection
Our brains need repetition and feedback to connect with new limbs.
Smart prosthetics that deliver real-time feedback help build that connection faster.
A device that vibrates when gripping softly teaches the brain far more quickly than one that just closes. Feedback tightens the learning loop between the muscle, brain, and device.
That shorter connection path means users get better faster—and clinics can move to advanced tasks sooner.
The Real-World Impact on Clinics
Better Patient Engagement
Smart tech inspires confidence.
When patients see their progress tracked and shown visually, they engage more. They practice more. Their families ask more questions. Motivation becomes collective.
Clinics become more than treatment centers. They become places where users see tangible strides, greeted by real data, not just hope.
Lower Long-Term Care Costs
Faster adaptation means less clinic time.
Early neural connection through smart limbs reduces chances of prosthetic abandonment.
When users get value quickly, they stay committed. That reduces follow-up needs and emergency visits caused by frustration or poor control.
Clinics become more efficient and user-centered.
Overcoming Challenges in Smart Prosthetic Integration
Infrastructure Must Catch Up With Innovation

As prosthetic technology advances, one of the biggest hurdles clinics face is infrastructure that hasn’t kept pace. Many centers still operate with basic therapy rooms and general-purpose rehab tools. While these serve basic needs well, smart prosthetics demand more.
Smart devices require clean, consistent power, proper sensor calibration tools, data tracking stations, and sometimes wireless connectivity for app integrations. Even something as simple as regular software updates needs a setup that’s stable and supported.
Clinics preparing to embrace this future must gradually upgrade—not in a costly, overwhelming way, but in small, strategic steps. A designated area for signal testing. A corner with clean power backups. A basic digital logbook to track usage trends. These small changes prepare the clinic for a larger wave of smart users.
Managing Expectations Between Promise and Reality
Another challenge that’s quietly growing is the gap between what patients expect and what these devices currently deliver.
We live in a time of big promises—artificial intelligence, robotics, automation. Patients come into clinics imagining robotic arms that do everything instantly. But smart prosthetics, while advanced, still require training, adaptation, and patience. They don’t work like magic.
It’s up to clinics and prosthetic teams to guide users gently through this learning curve. Helping them understand that the limb is a tool—not a replacement, but a new beginning. Clinics that frame the journey as a partnership between human and machine—rather than a product that solves everything—tend to see better patient satisfaction and engagement.
Managing expectations is not about lowering hopes. It’s about preparing users for the real, rewarding work of rewiring their brains and reclaiming control.
Building Skill Pipelines for a Smart-Ready Workforce
Training the Next Generation of Therapists
To truly use smart prosthetics well, the people helping patients must also evolve. Traditional physiotherapy training rarely covers sensor calibration, signal testing, or interpreting myoelectric data. Yet these are now becoming everyday parts of the job.
Clinics looking to thrive in this new world should begin cross-training their teams in digital tools, basic bionic control theory, and user motivation strategies tailored to neuroplasticity.
It doesn’t need to be complex. Short workshops. Partner sessions with device makers like RoboBionics. A monthly discussion of patient case studies.
The more the clinical team understands how these smart devices behave and evolve, the more they can fine-tune therapy, troubleshoot issues quickly, and keep users motivated.
Collaboration Between Clinics and Tech Companies
Another smart move for clinics is forming long-term partnerships with prosthetic innovators.
Instead of just being customers, they become collaborators—testing updates, giving feedback, and receiving early access to new tools. These partnerships help both sides grow. Tech companies gain real-world insights. Clinics gain access to support, training, and better solutions for users.
For example, at RoboBionics, we often co-develop new training methods based on feedback from partner clinics. We listen to what patients struggle with and design simple solutions, be it grip fine-tuning, button ease, or app interface changes.
This kind of back-and-forth drives better outcomes and fosters a new standard of care—where clinics are not just users of smart tools but co-creators of smart futures.
Artificial Intelligence and Personalization in Everyday Care
AI Is Becoming the Invisible Therapist

In the next wave of smart prosthetics, artificial intelligence will not just enhance performance—it will quietly personalize care without needing constant input from clinicians.
AI in smart prosthetics can already begin to learn how a user moves, when they tire, how much force they apply, and which tasks they repeat. Over time, these systems can adjust grip sensitivity, optimize battery usage, and even suggest training exercises based on use patterns.
For clinics, this means one very big shift—less micromanagement of the device and more focus on emotional and behavioral coaching.
When a prosthetic becomes responsive on its own, therapists can spend more time helping patients build confidence, improve coordination, or return to work or school with dignity.
It’s a subtle but important evolution. AI helps remove friction from basic use so clinics can focus on what makes long-term adaptation successful: trust, consistency, and self-belief.
Tailored Prosthetic Profiles for Every Patient
Another fast-growing trend is the idea of “prosthetic profiles”—unique user settings saved across devices or platforms.
This could mean that a patient’s preferred grip speed, vibration feedback strength, or switching gestures are remembered—even if the device is serviced, replaced, or upgraded.
Clinics that offer this kind of continuity stand out. Users don’t feel like they are starting over with each visit. They feel known, understood, and supported.
This personal memory—powered by cloud sync or onboard learning—creates a smoother experience, one where every touchpoint continues the user’s progress, not restarts it.
Changing the Way Clinics Measure Success
Beyond Strength and Range
For years, prosthetic success was measured by how well someone could lift, move, or walk. Strength and range were the gold standard.
But with smarter prosthetics, the real indicators are becoming more nuanced.
Does the patient choose to use the limb daily? Do they feel confident in public? Can they make decisions without overthinking movement?
These questions point to psychological and neurological adaptation—far more telling than grip strength alone.
Clinics must begin redefining their metrics of success. They can still measure strength and control, but they must also track emotional ownership, real-world usage, and user confidence.
These are the signals that show true integration between brain and limb.
The Rise of Self-Reported Progress
More clinics are starting to use patient-reported outcomes—simple questions like:
- How many hours did you use the device today?
- Did you use the limb in a public setting?
- Were you able to complete a task without looking directly at the hand?
These questions invite honest reflection and help therapists measure brain adaptation, not just muscle performance.
Smart prosthetics support this too—devices can provide usage stats, which can be compared with self-reports to understand gaps, fears, or avoidance behaviors.
Together, this builds a fuller picture of progress—and helps clinics offer better support.
The Clinic of the Future: What Will It Look Like?
A More Integrated, Less Clinical Space

Future-ready clinics will look and feel different. Less like hospitals, more like collaborative learning labs.
Instead of rows of equipment, they may have smart zones—one for fine motor training, another for real-life task simulations like cooking or dressing, and another for digital calibration.
Spaces will be warm, not sterile. Therapy will happen in environments that mimic real life—because that’s where real success will be measured.
These clinics will offer a blend of science, emotion, and technology. They’ll serve not just to “fix” movement, but to help people feel whole again.
Digital Follow-Ups as the New Normal
As smart prosthetics continue to evolve, follow-up visits won’t always need a physical clinic. Many updates will happen via apps. Video calls will replace in-person fittings for minor tweaks.
Clinics that set up digital channels—WhatsApp lines, video guides, tele-rehab options—will keep users engaged, supported, and updated. It reduces travel, increases comfort, and keeps the prosthetic central to the user’s life, not pushed aside during gaps in care.
This hybrid care model—part in-person, part digital—is the future. And clinics that adapt now will stay ahead of the curve.
Rethinking Relationships Between Clinics, Patients, and Technology
Moving From Providers to Partners in Progress
As smart prosthetics become more adaptive and intuitive, the role of the clinic shifts from being a one-time service provider to an ongoing growth partner. In the past, fitting a limb was the peak of service. Now, it’s just the beginning.
Smart prosthetics evolve with the user. As muscle signals grow stronger, as confidence improves, and as feedback becomes more natural, the prosthetic needs tuning, retraining, and emotional support.
This means clinics must build long-term relationships with users. The goal is not just to hand over a device—it’s to help patients truly own their progress, both physically and mentally. This shift turns clinics into collaborators in a patient’s life journey, not just in their recovery.
It requires consistency, compassion, and commitment. But when done right, the clinic becomes the place where life begins again—not just where a limb is fitted.
Smart Devices Need Smart Support Systems
No matter how advanced a prosthetic is, it still depends on the systems around it.
Batteries need charging. Apps need updates. Sensors need alignment. But even more than that, patients need reassurance. They need to know someone is there when a problem arises. That someone understands how their brain is adjusting. That someone is invested in helping them succeed.
Clinics that offer this layer of intelligent support—through trained teams, easy access, and open communication—build trust faster. And trust is what helps a patient wear the device daily, keep practicing, and build emotional connection.
When the user feels backed by people who understand both the machine and the mind, adaptation accelerates. Confidence increases. Abandonment drops.
Technology alone can’t make that happen. Human support can.
A New Standard of Care: What Clinics Should Prepare For
Expect Smarter, More Demanding Patients
As information becomes easier to access, patients will arrive knowing more. They’ll have seen videos, read blogs, watched testimonials. They’ll expect sensory feedback, AI assistance, personalization, and seamless use.
Clinics must be ready—not just to meet these expectations but to guide them.
The smartest clinics won’t just answer questions. They’ll anticipate them. They’ll offer demos that explain how grip adjustments work, how brain signals improve, and how smart limbs help not just with function—but with freedom.
This patient awareness is not a challenge. It’s a gift. Because when a patient comes ready to learn, the rewiring happens faster. Progress is smoother. And success becomes shared.
Train With an Eye on Tomorrow
Prosthetics today are already reading myoelectric signals and sending haptic feedback. Tomorrow’s devices may include thermal sensors, pressure-based microresponses, or even light neural interfacing.
That’s not far off. Which means today’s clinics need to start preparing their teams—especially therapists and support staff—for what’s coming next.
Regular training sessions, partnerships with companies like RoboBionics, and exposure to early prototypes can help your clinic stay ahead. And that means when patients come in with advanced limbs, your team is ready—not learning from scratch.
Being future-ready doesn’t mean being perfect. It means being open, curious, and committed to growing as technology does.
Final Thoughts: Smart Technology, Human Hearts
The Limb Is Just the Start—The Real Work Happens in the Brain

Smart prosthetics are incredible machines. But they only change lives when they are embraced, used daily, and emotionally accepted.
That’s why clinics matter more than ever.
Because while the limb is fitted to the body, it’s the clinic that helps it connect to the brain.
Every time you encourage a patient through their first shaky grip, every time you help them understand a training routine, or comfort them after a hard session—you are helping the brain say, “Yes, this belongs to me now.”
That moment, when the brain stops resisting and starts accepting, is the true miracle. It’s not in the chip or motor—it’s in the human decision to adapt.
Your Clinic Can Lead the Future
India is on the edge of something powerful. With growing access to advanced prosthetics like Grippy™, and strong awareness of brain plasticity, more lives can be rebuilt than ever before.
But only if clinics are ready.
Ready to treat technology as part of care, not separate from it. Ready to offer emotional guidance, not just physical training. Ready to stand with patients, not just fit them.
The future of prosthetics isn’t happening somewhere else. It’s happening here—in the minds of people learning to move again, and in the hands of clinics like yours, helping them believe they can.
If you’re a rehab center, a hospital, or a care team interested in building your smart prosthetic capabilities, RoboBionics is here to support you.
Schedule a clinic session, staff training, or live Grippy™ demo at www.robobionics.in/bookdemo
Because the future is not just about smart limbs—it’s about smart, heart-led care.



