In India, thousands of amputees receive prosthetic devices each year. But fitting the device is only the first step. The real challenge begins after—when patients must learn to use it in daily life.
Training is essential, but advanced rehab tools are often too costly for many families and clinics. This gap leads to frustration, poor adoption, and in many cases, the device being left unused.
The good news is that effective training does not always need expensive equipment. With creativity, the right guidance, and simple adaptive devices, patients can practice at home and in clinics—without heavy costs.
This article explores practical ways Indian patients can train with low-cost adaptive devices. It also highlights how clinics, caregivers, and families can make rehab accessible, engaging, and effective.
Why Training Matters More Than Just the Device
A Prosthetic Without Training Becomes a Burden

When patients receive a new prosthetic hand or leg, there is excitement at first. Families hope life will return to normal quickly. But without proper training, most patients struggle.
The device may feel heavy. Movements may feel awkward. Tasks that should be simple, like holding a glass of water, can seem impossible. Frustration grows, and many patients eventually stop using the device.
The real problem is not the prosthetic—it is the lack of structured training that teaches the brain how to work with it.
The Brain Needs Time to Adjust
Every movement starts in the brain. When a prosthetic is introduced, the brain must rewire itself to control it. This process is called neuroplasticity.
Neuroplasticity allows the brain to create new pathways, but it does not happen instantly. It takes repetition, patience, and consistent effort. Training gives the brain the signals it needs to adapt.
Without regular practice, the brain does not fully accept the prosthetic as part of the body. This is why proper rehab is just as important as the device itself.
Training Builds Confidence and Independence
Patients who train regularly see progress—even in small steps. Holding an object for a few seconds longer, gripping with more control, or completing a simple task all boost confidence.
This confidence pushes them to keep trying. It also reduces dependence on family members for daily activities. Over time, training transforms the prosthetic from something unfamiliar into a trusted part of life.
Low-Cost Training Solutions Are the Key in India
In many Indian clinics, advanced rehab equipment is too expensive. Families in rural and semi-urban areas cannot afford long sessions in distant centers.
This is where low-cost adaptive devices play a vital role. Simple, affordable tools can help patients train effectively at home or in small clinics. With the right guidance, they can achieve the same brain adaptation as those using advanced systems.
Making training accessible is not only practical—it is essential for long-term success.
The Challenges Indian Patients Face in Training
Distance From Rehabilitation Centers
Many patients in India live far from cities where prosthetic centers are located. Traveling long distances for frequent training sessions is costly and time-consuming.
As a result, patients often attend only a few sessions after receiving their device. Without ongoing practice, the brain does not get enough repetition to adapt. This leads to slow progress and eventual abandonment of the prosthetic.
Limited Awareness About Neuroplasticity
Most patients and families do not know that the brain must be trained to control the prosthetic. They expect the hand or leg to work immediately, just like the natural one did.
When they experience difficulty, they think the device is faulty or that they are not capable of using it. This lack of awareness creates frustration and stops them from continuing training.
Educating patients and caregivers about neuroplasticity is the first step in overcoming this barrier.
Financial Constraints
Formal rehab programs can be expensive, especially when advanced training equipment is used. Many families in rural and semi-urban India cannot afford prolonged therapy.
Even transport, accommodation, and lost wages add to the cost of rehabilitation. This makes low-cost, at-home adaptive training devices essential for ensuring long-term success.
Emotional and Social Pressures
Amputees often face stigma in their communities. Some feel embarrassed to train in front of others. Others lose motivation because family members unintentionally compare their progress to unrealistic expectations.
Without emotional support, patients may give up even if they have the potential to improve. Building confidence is as important as physical training.
Device Discomfort and Abandonment
If the prosthetic is uncomfortable, too heavy, or difficult to control, patients avoid wearing it. Without regular use, training becomes impossible.
In India, this often leads to devices being abandoned in a cupboard—unused and forgotten. The solution lies not just in better prosthetic design but also in patient-centered training methods that build trust and ease.
Designing Low-Cost Adaptive Devices for Training
Why Simplicity Matters

In India, most patients do not have access to high-tech rehab centers or robotic simulators. If adaptive devices are too complex or costly, they will never reach the majority of people who need them.
That is why simplicity is the most important design principle. A good training device should be light, affordable, and easy to use at home. It should not require electricity, internet, or complicated instructions.
When training is simple, patients are more likely to practice daily. And daily practice is what rewires the brain.
Using Everyday Objects as Adaptive Tools
Low-cost training doesn’t always require specialized devices. Many household items can double as adaptive tools if used in the right way.
A sponge ball can help patients practice grip strength. A steel tumbler filled with water can train balance and control. A towel can be used for pressing, folding, or twisting motions that activate muscle signals.
These objects are familiar, affordable, and easy to replace. Most importantly, they connect training to real life, which makes the brain pay more attention.
Purpose-Built Low-Cost Devices
While everyday items are useful, purpose-built adaptive devices can make practice more structured. For example, a simple resistance band like BrawnBand from RoboBionics helps activate and strengthen the residual muscles that send signals to a prosthetic hand.
This kind of device doesn’t cost much, but it provides focused training that builds both muscle memory and neuroplasticity.
Similarly, lightweight training boards with objects of different textures, shapes, and weights can help patients practice fine motor skills in a more systematic way.
Gamification to Keep Patients Engaged
One of the biggest challenges in rehab is boredom. Repeating the same task every day can feel tiring, especially when progress is slow.
Gamified training solves this. With simple apps or even paper-based scoring systems, patients can track their progress like a game. For example, counting how many times they can pick up an object in one minute and trying to beat their own score the next day.
This approach makes practice fun. And when patients enjoy training, the brain stays more engaged and learns faster.
Training Devices Must Be Portable
Many Indian patients travel for work or live in small houses with limited space. If a training device is bulky or difficult to carry, it will not be used regularly.
Portable designs are key. A patient should be able to put the device in a bag, take it to work, or use it while sitting at home. The easier it is to access, the more likely they are to stick with the routine.
Safety and Comfort Cannot Be Ignored
Low-cost does not mean low-quality. Training devices must still be safe and comfortable to use. If they cause pain, skin irritation, or strain, patients will abandon them.
Soft padding, adjustable resistance, and simple instructions make adaptive devices more patient-friendly. The design should always keep the end user in mind—someone who may not be medically trained but still wants to practice on their own.
Bridging the Gap Between Clinic and Home
The biggest benefit of low-cost adaptive devices is that they extend training beyond the clinic. Instead of relying only on short therapy sessions, patients can continue practicing at home.
This bridge between clinic and home is essential in India, where regular travel is often not possible. Adaptive devices give patients independence, control, and the opportunity to train daily without added financial stress.
How Clinics Can Introduce Low-Cost Training Into Their Rehab Programs
Start With Patient Education

The first step is awareness. Most patients believe a prosthetic should work instantly, like a natural limb. When it doesn’t, they feel discouraged.
Clinics can change this by starting every fitting with a simple explanation: “Your brain controls this hand. The more you practice, the better your brain will learn.”
Even a short talk or demonstration helps patients understand that training is not optional—it is the most important part of success.
Create Basic Training Kits for Patients
Instead of sending patients home empty-handed, clinics can provide small, low-cost training kits. These could include a sponge ball, a towel, a lightweight plastic cup, and printed instructions with pictures.
Such kits cost very little to prepare but give patients the tools they need to keep practicing daily. They also remind families that rehab doesn’t stop at the clinic door.
Over time, clinics can brand these kits, turning them into a unique service that sets them apart from competitors.
Use Group Training Sessions
Individual therapy is ideal, but it isn’t always practical in busy or resource-limited centers. Group training can be an effective alternative.
When patients practice together, they learn from each other’s struggles and successes. It reduces feelings of isolation and creates a sense of community.
For clinics, group sessions also save time and allow one therapist to support multiple patients at once, making rehab more affordable and scalable.
Track Progress in Simple, Visible Ways
Patients often feel like they are not improving, even when they are. Clinics should make progress visible.
This can be done by recording short videos during early sessions and comparing them with later progress. Or by using a simple chart where each successful grip, hold, or release is marked.
When patients see improvement with their own eyes, their confidence grows. And with confidence comes consistency.
Train Families to Support the Process
In Indian households, family plays a huge role in recovery. But without guidance, relatives may unintentionally discourage patients by saying things like, “Why isn’t it working yet?”
Clinics can solve this by offering short family training sessions. Teach caregivers how to encourage without pressure, how to celebrate small wins, and how to remind patients gently to practice.
A supportive home environment doubles the chances of long-term device use.
Partner With Local Innovators
India has a growing ecosystem of startups creating affordable rehab tools. Clinics can partner with them to introduce low-cost adaptive devices to patients.
For example, RoboBionics offers products like Grippy™, BrawnBand, and gamified rehab apps designed to work in Indian conditions. These partnerships give clinics affordable, effective tools while giving patients better chances at success.
By showcasing these innovations, clinics also position themselves as leaders in modern, accessible care.
Helping Patients Stay Motivated With Low-Cost Adaptive Devices
Motivation Is as Important as Movement

Even when adaptive devices are affordable and accessible, patients may lose motivation if they don’t see quick results. Training feels slow, progress feels invisible, and frustration builds.
That is why keeping patients motivated is just as important as giving them the right tools. A motivated patient will keep practicing even on difficult days, and that consistent effort is what leads to brain adaptation.
Celebrate Small Wins Every Day
Progress in prosthetic training is often measured in tiny steps. The first time a patient picks up a spoon without dropping it. The first time they hold a glass of water for five seconds longer than before.
Clinics and families should celebrate these small wins. Saying, “That was better than yesterday,” or clapping after a small achievement makes a big difference.
These celebrations may feel minor, but they build emotional momentum. They remind the patient that every attempt counts.
Turn Practice Into a Game
Repetition is necessary, but it can also feel boring. To make training engaging, turn it into a game.
For example, challenge the patient to see how many times they can grip and release an object in one minute. Keep track of the score and encourage them to beat their own record the next day.
This playful competition adds energy to the process. It also helps the brain stay curious and attentive during training.
Involve Peers or Community Support
When patients train alongside others with prosthetics, they feel less isolated. Seeing another person succeed makes them believe they can succeed too.
Community-based group sessions or peer mentoring programs can create this effect. Even small gatherings in a clinic or village hall can give patients the motivation they need to continue.
In rural areas, local health workers or ASHAs can also organize group check-ins to track progress and encourage patients together.
Make Motivation Part of the Routine
Motivation should not be treated as an afterthought. It should be built into every training routine.
Simple practices like keeping a progress diary, setting weekly goals, or recording video milestones make patients feel proud of their journey. Families can also take photos of improvements to show how far the patient has come.
These habits remind patients that they are moving forward, even when the journey feels slow.
The Role of Technology in Low-Cost Adaptive Training in India
Smartphones as Training Partners
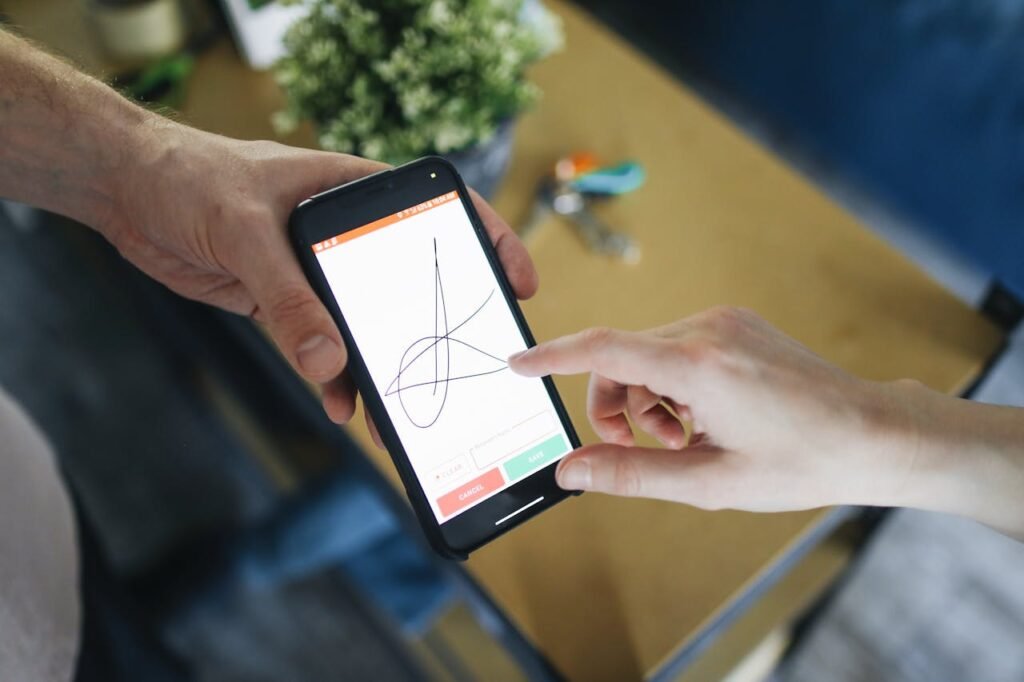
In rural and urban India alike, smartphones have become common. They can be powerful tools for prosthetic training when used creatively.
Patients can record their practice sessions and watch them later. This gives the brain extra feedback and helps patients notice small improvements they might otherwise miss. Families can also share these videos with therapists for quick guidance without long travel.
Even a simple timer or reminder app can help patients stay consistent with daily training.
Gamified Rehab Apps
Training often feels repetitive, which can lower motivation. Gamified apps turn practice into something fun and interactive.
For example, RoboBionics has developed a Gamified Rehabilitation App that allows patients to see their progress as part of a challenge. They earn points, complete levels, and get visual feedback for their effort.
This kind of digital engagement keeps patients practicing longer and more often, which strengthens neuroplasticity. It also makes rehab more exciting for younger users who may otherwise lose interest quickly.
Tele-Rehab to Reach Remote Patients
Traveling long distances to prosthetic centers is a barrier for many Indian patients. Tele-rehab provides a solution.
With video calls, therapists can guide patients through simple exercises using the adaptive devices they have at home. They can correct posture, suggest adjustments, and provide encouragement—all without the patient leaving their village.
This not only saves costs but also ensures consistent practice, which is critical for brain adaptation.
Data Tracking for Better Progress Monitoring
Digital tools can also track progress in ways that motivate patients. Apps or wearable sensors can count repetitions, measure grip time, or log daily activity.
For patients, this creates visible proof of improvement. For clinics, it provides valuable data to refine training programs and offer more personalized support.
Even simple tracking, like using a WhatsApp group where patients report daily practice, can keep engagement high.
Affordable, Locally Built Innovations
India is home to many startups creating cost-effective solutions for adaptive training. Devices like RoboBionics’ BrawnBand stimulate muscles to strengthen signals to the brain, making prosthetic control easier.
Because these tools are designed for Indian conditions, they are more affordable, durable, and practical than imported alternatives.
By combining such innovations with simple tech like smartphones and tele-rehab, clinics can bring advanced brain-based training within reach of every patient—whether in a metro city or a small rural village.
Building Sustainable Rehab Models for Low-Income Patients
Affordability Must Be Built Into the System
For many patients in India, the cost of long-term rehab is just as overwhelming as the cost of the prosthetic itself. Travel, therapy sessions, and time away from work make consistent training difficult.
That’s why sustainability depends on affordability. Clinics must design rehab models that work even for families with very limited resources. This can mean shorter but more frequent sessions, shared group training, or home-based programs that require minimal spending.
When rehab is affordable, patients stay engaged for the long term.
Focus on Home-Based Training
Most Indian patients cannot visit clinics regularly. That makes home-based rehab essential.
By giving patients simple adaptive devices and clear instructions, clinics can extend the training environment into their homes. This keeps the brain practicing daily, even when professional supervision is not possible.
Home-based models also reduce travel costs, making them more practical for low-income families in rural areas.
Build a Strong Support System Around the Patient
Patients in low-income settings often feel isolated during their recovery. They may have fewer opportunities to meet peers who are going through the same challenges.
This is where community and family support becomes vital. Clinics can create local peer groups, encourage families to take an active role, and train local health workers to provide simple follow-up support.
When the patient feels supported by the people around them, they are less likely to give up.
Use Partnerships to Lower Costs
Prosthetic centers don’t have to carry the full cost of rehab programs alone. Partnerships with NGOs, government health programs, and startups can provide resources and tools at lower costs.
For example, NGOs working in rural health can help distribute adaptive devices or train ASHAs to support basic rehab practices. Local startups like RoboBionics can provide affordable prosthetics and muscle training tools.
These partnerships make rehab more sustainable while also expanding the reach of brain-based care.
Train Health Workers to Carry Rehab Forward
Not every village will have a therapist or prosthetist. But almost every village has ASHAs or community health workers. By training them in simple neuroplasticity-based rehab methods, clinics can multiply their impact.
These workers don’t need to deliver complex therapy. They just need to guide patients in daily practice, check progress, and provide encouragement.
This approach ensures that rehab doesn’t stop when the patient leaves the clinic—it continues in the community at very little cost.
The Business Case for Low-Cost Adaptive Training in India
Reducing Device Abandonment
One of the biggest challenges for prosthetic providers is abandonment. A patient receives a device, but within months it ends up in a cupboard, unused. This hurts both the patient and the clinic.
Low-cost adaptive training directly reduces abandonment. When patients see progress through simple, consistent practice, they are more likely to keep using the prosthetic daily. For businesses, this means happier patients, stronger reputations, and higher trust in their services.
Creating Affordable Value-Added Services
Clinics often limit themselves to fitting and adjustments. But adding structured, low-cost rehab services creates new value streams. Simple rehab kits, group training packages, and digital follow-up programs can all be priced affordably while still generating revenue.
These services not only help patients but also set clinics apart in a competitive market. Families will prefer a provider who offers long-term support rather than one who simply delivers the device.
Building Loyalty and Word-of-Mouth Growth
In India, word of mouth remains one of the strongest drivers of healthcare decisions. A patient who feels supported during rehab is far more likely to recommend a clinic to others.
By offering affordable adaptive training, clinics can build deeper trust with patients and their families. That trust leads to long-term loyalty, repeat visits, and organic referrals that no marketing budget can buy.
Aligning With India’s Healthcare Priorities
India’s healthcare system increasingly emphasizes accessibility, affordability, and community-based care. Clinics that adopt low-cost adaptive training align themselves with this national mission.
This opens opportunities for partnerships with government programs, CSR initiatives, and NGOs—all of which are looking for sustainable, community-driven health solutions.
By showing commitment to affordable neuroplasticity-based rehab, prosthetic centers can position themselves as leaders in inclusive healthcare.
Conclusion: Making Adaptive Training a Standard, Not a Luxury
The True Value of a Prosthetic

A prosthetic is not just a device—it is a bridge between independence and limitation. But that bridge only works if the brain learns how to cross it.
Without training, even the most advanced prosthetic can fail. With consistent, affordable training, even simple devices can change lives.
Low-Cost Does Not Mean Low Impact
In India, success lies in solutions that are simple, scalable, and affordable. Low-cost adaptive devices are not a compromise—they are the key to ensuring that every patient, whether in a city or a small village, gets the chance to adapt and thrive.
The most powerful changes often come from small tools, daily routines, and family encouragement. When these elements come together, the brain adapts, the device becomes natural, and the patient regains confidence.
A Call for Action
For prosthetic centers, caregivers, and health workers across India, the message is clear: low-cost adaptive training must be part of every rehab journey. It is not optional. It is not secondary. It is the difference between success and failure.
At RoboBionics, we are committed to building this future. Through innovations like Grippy™, BrawnBand, and our gamified rehab app, we are making brain-friendly, affordable solutions available to every corner of India.
Let’s make sure no prosthetic goes unused, no patient loses hope, and no brain is left behind. Book a free demo with RoboBionics today.



