Starting your recovery after limb loss can feel overwhelming. There are so many questions, emotions, and new things to learn. One of the first steps in this journey, especially if you’re preparing for a prosthetic, is EMS therapy.
EMS stands for Electrical Muscle Stimulation. It’s a gentle, science-backed way to wake up your muscles using small electrical signals. These signals help your muscles move—even if you can’t move them on your own yet.
But what actually happens during the first month of EMS therapy? How do you know if it’s working? What should you feel? What should you do each day?
This guide is here to walk you through all of it. Day by day. Week by week. We’ll explain what to expect, how to get the most out of each session, and how to stay hopeful even when it’s tough.
Let’s get started.
Week 1: Getting Started With EMS Therapy
Your First Session
The first EMS session is more about comfort than results. It’s your body’s introduction to something new. You might feel nervous, and that’s completely normal.
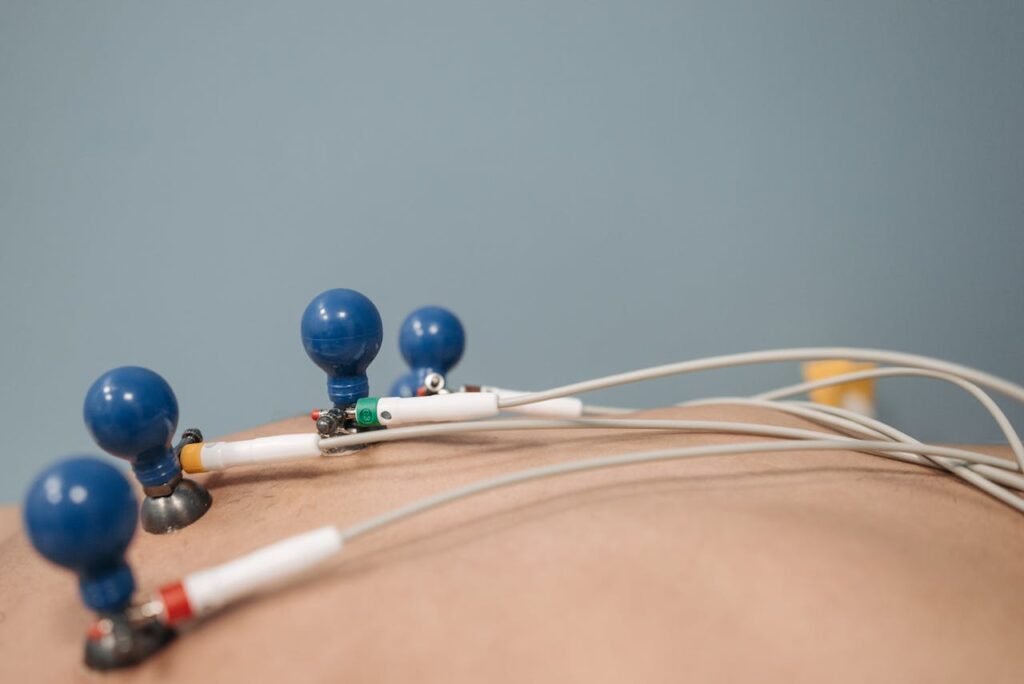
The therapist will place small sticky pads, called electrodes, on your skin. These go over the muscles you still have in your arm or leg. Then, they’ll start a low-level current. It feels like a light buzzing or tapping under the skin.
There’s no pain. Just a strange new feeling.
Some people feel a slight twitch in the muscle. Others don’t feel much at all in the beginning. Both are okay. Everyone’s body responds differently, and the first few sessions are just about helping your brain and muscles get familiar with the sensation.
The Main Goal This Week
In Week 1, the focus is simple: activation. The muscles may have been resting since the amputation. This week is about waking them up slowly.
You may have short sessions—maybe 10 to 15 minutes. You won’t do much active movement yet. It’s more about learning how to relax into the therapy and stay consistent.
Think of it like laying the first stone in a new building. Small, but important.
What You Might Feel
Some common things people feel in the first week:
- A tingling or pulsing feeling
- Mild fatigue in the area
- Slight muscle movement or no movement at all
- Emotional reactions—frustration, surprise, hope
All of this is normal. It’s okay to feel uncertain. What matters is showing up each day and trusting the process.
How to Support Yourself at Home
Between sessions, rest is key. Drink plenty of water. Gently stretch the limb if advised by your therapist.
This week is also a good time to start observing your limb. Notice how it feels before and after EMS. Keep a small notebook and write down:
- Where the pads were placed
- How strong the sensation was
- What movement or feelings you experienced
These notes will help track your progress later.
Week 2: Building Connection Between Brain and Muscle
Something Starts to Shift

In the second week, you may notice the muscle starting to respond a bit more clearly. The tingling may feel stronger, or the twitch may turn into a soft contraction.
This is a good sign. It means your nerves and muscles are talking again.
Even if the movement is small, it’s a step forward. In fact, these early twitches are the foundation of future control—especially if you plan to use a myoelectric prosthetic like the Grippy™ Bionic Hand.
Adding Intentional Movement
Now that the muscle is starting to respond, your therapist may ask you to try something new: move the muscle at the same time as the EMS pulse.
This is called active contraction. Even if you can’t see the movement, trying to move while the pulse is on helps train your brain.
For example, if EMS is stimulating your forearm, try to open or close your phantom hand as the pulse happens.
This combination teaches your brain how to send signals more clearly and helps rebuild muscle memory faster.
Managing Fatigue
You may start to feel a bit tired after sessions now. That’s a good sign—it means your muscles are working.
Listen to your body. If the area feels sore or tired, it’s okay to take breaks. Your therapist may adjust the intensity or give you shorter sessions with more rest in between.
Always tell your therapist how you’re feeling. EMS is most effective when it’s adjusted to match your comfort.
Emotional Growth
By now, you may also feel a bit more hopeful. Seeing your body respond, even in small ways, is empowering.
You may also feel more comfortable with the routine. It becomes part of your day—a signal to yourself that you’re healing, that you’re moving forward.
Week 3: Strengthening the Signal and Building Muscle Control
When the Body Starts Talking Back
By the third week of EMS therapy, something beautiful often begins to happen—your muscles not only react to the stimulation, but they begin to work with it.
At this stage, your body is no longer just being “stimulated.” It’s responding. You may start noticing small changes that seemed impossible just two weeks ago.
Maybe your arm feels warmer, stronger, or more “alive.” Maybe you see a visible flicker when you try to move. Maybe you feel a little more in control.
These are signs that your brain and muscles are connecting again, and that the electrical pulses are waking up deeper layers of muscle and memory.
Moving from Passive to Active Therapy
Until now, EMS has been doing most of the work. But in Week 3, the focus begins to shift toward muscle training. It’s no longer about just sending signals. Now it’s about how you respond to them.
Your therapist may ask you to:
- Contract your muscle just before or during the pulse
- Hold the contraction for a few seconds after the pulse ends
- Try light resistance or isometric exercises while the EMS is on
These steps sound small, but they’re powerful. They help build voluntary control—which is critical if you’re preparing for a myoelectric device.
The goal is to strengthen not just the muscle, but the communication between your brain, nerves, and muscles.
It’s like teaching your body a new language. And in Week 3, you’re finally starting to speak.
Customizing Pad Placement for Best Results
By now, your therapist will likely have a good sense of which areas respond best to stimulation. This is the time to fine-tune pad placement.
Even a shift of half an inch can make a big difference in how well your muscle contracts. Some patients respond better when pads are slightly rotated. Others need larger pads for broader stimulation.
Don’t hesitate to give feedback. If something feels stronger, lighter, or different—say it. The more your therapist knows, the better they can personalize your therapy.
Managing Expectations
While progress is exciting, it’s also normal to hit small plateaus. Maybe you felt great improvement last week, and now it feels slower.
That’s okay. The body doesn’t heal in a straight line. Some days feel like leaps. Others feel like slow steps. Both are part of the journey.
If you’re feeling discouraged, remember this: the first 30 days are not about perfection. They’re about possibility. Every flicker, every twitch, every effort counts.
Integrating Simple Movements
Along with EMS, this week may include basic functional tasks:
- Picking up soft objects
- Closing your hand around a towel
- Reaching forward during stimulation
These actions help your brain link the stimulation to real-life movement.
If you’re training to use a device like Grippy™, this is also the week to start imagining those movements in sync with EMS. Visualize using the hand. Picture the grasp. Feel the movement—even if it’s not there yet.
These mental exercises help build neurological blueprints for future control.
Keeping Track of Progress
This is a good week to start a visual log. If possible, take short videos or photos of your muscle response during EMS.
Watch how the response improves over time. Share these with your therapist. It’s encouraging to see how far you’ve come—even when the change feels small.
Also, continue noting how you feel emotionally after each session. You may be surprised to see that your confidence, mood, and sense of possibility improve just as much as your physical strength.
Week 4: Preparing for Long-Term Success
From Muscle Movement to Mindset Shift

By the time you reach the fourth week of EMS therapy, something shifts—not just in your body, but in your mindset. What once felt strange, even scary, now starts to feel like routine. You’re no longer learning what EMS is, you’re learning how to grow with it.
Week 4 is where many people move from recovery into preparation. You’re no longer just trying to keep muscles alive—you’re preparing your body for long-term control, strength, and confidence. Whether that means getting ready for a myoelectric prosthetic like Grippy™, or simply improving your quality of life, this week becomes your stepping stone.
More Control, More Responsibility
As your muscles become more responsive and your signals stronger, your therapist may start giving you more control during EMS sessions.
This could include:
- Adjusting your own intensity settings (under guidance)
- Placing pads with less help
- Choosing specific muscles to work on based on your needs
You may be asked to do tasks while EMS is active. For example, practicing light daily tasks like:
- Turning a doorknob
- Holding a pen
- Pulling a zipper
These might seem simple, but they help your brain learn how to use the muscle signals in practical ways. This is crucial, especially if you’ll soon be using a bionic hand that relies on real-time myoelectric input.
Strengthening the Foundation
At this point, EMS is not just about movement—it’s about building endurance. Your sessions might grow longer—20 to 30 minutes. The stimulation may be slightly stronger. You might hold contractions for longer or repeat more cycles.
Why does this matter?
Because using a prosthetic hand takes more than strength—it takes stamina. Just like you can’t run a marathon without training, you can’t expect to control a device for hours a day without building muscle endurance.
EMS in Week 4 helps prepare you for that.
Introduction to Biofeedback (If Available)
Some advanced rehab centers use tools like biofeedback, where you can see your muscle signals on a screen.
This allows you to track how strong or consistent your muscle contractions are. It helps you understand how small changes in posture, breathing, or effort affect the signal.
If you’re getting fitted for a Grippy™ Bionic Hand soon, this kind of feedback can be extremely helpful. It shows whether your signals are strong enough and teaches you how to adjust in real time.
Ask your therapist if such tools are available at your center. If not, even simple methods like watching your muscle contract in a mirror or recording short videos can help.
When Setbacks Happen
It’s important to be honest: not everyone sees fast, steady progress in four weeks. Some people have great muscle movement by now. Others are still waiting for their first flicker.
That’s okay.
The first 30 days of EMS are not a finish line. They’re a starting block. If things are slower than you expected, talk to your therapist. Sometimes small changes in pad placement or frequency can make a big difference.
Also, remember—recovery isn’t just about muscles. It’s about emotion, confidence, and belief. Every small win is still a win.
Starting to Think Beyond 30 Days
As you near the end of your first month, it’s time to think ahead.
Ask yourself:
- Do I want to continue EMS therapy?
- How can I make this part of my daily life?
- Am I ready for the next step, like prosthetic training?
- What questions do I still have about my recovery?
Your therapist can help you answer these questions and set a path forward. Whether that means continuing EMS, starting trials with a prosthetic, or adding new therapies—it’s all part of building your future.
Turning the First 30 Days into a Long-Term Advantage for Clinics and Rehab Centers
Why the First 30 Days Matter for You as a Provider

For prosthetic clinics and rehab centers, the first 30 days of EMS therapy aren’t just about patient recovery—they’re your most powerful window to build trust, demonstrate value, and create a repeatable system of care.
This is where patients decide whether they believe in their recovery, in themselves—and in you.
That’s why this first month should never be seen as just “introductory therapy.” It should be your signature experience. Something that builds a strong reputation and drives long-term outcomes.
Offer a Named Program
Don’t just say “EMS sessions.” Brand your first-month approach as a clear, named program. Something like:
- “30-Day Neuromuscular Kickstart”
- “Grippy™ Readiness Plan”
- “EMS PowerStart Protocol”
This makes your service easier to sell, easier to understand, and far more likely to be remembered.
Patients feel they’re enrolling in a structured, time-tested system—not just attending random appointments.
Use Session 15–20 as a Checkpoint for Long-Term Planning
As patients near the end of their first month, make Session 15 or 20 a goal-setting session. Sit down and review:
- Their muscle responsiveness
- Phantom pain status
- Progress toward prosthetic control
- Home-readiness for EMS
Then, give them a printed progress sheet and a menu of next steps—whether that’s transitioning to at-home EMS, trialing a prosthetic, or adding functional therapy.
Patients love seeing where they are and where they’re going. It builds confidence and strengthens commitment.
Encourage Patients to Document Their Journey
From a business standpoint, EMS therapy offers built-in moments that can be turned into social proof—with consent.
Encourage patients to take photos, write short logs, or even record simple videos throughout the first 30 days. Highlight their first visible twitch, first grip, or first moment of hope.
With their permission, these become powerful testimonials for your center.
You’re not just showing that you provide care—you’re showing that your care delivers real results.
Planning the Next Steps After 30 Days of EMS
The First Month Was Just the Beginning

After 30 days of EMS therapy, you’ve taken a huge first step. You’ve reconnected with muscles that were silent. You’ve trained your brain to speak to your body again. And you’ve built the habits that lay the groundwork for the rest of your recovery.
But where do you go from here?
What happens after the first month depends on your goals, your progress, and your personal journey. There is no single roadmap. But there are clear signs to help guide your next move.
Step 1: Talk to Your Therapist About Readiness
Your therapist will likely do a full review of your EMS progress. They’ll check:
- How strong your muscle responses are
- How well you can time your contractions
- Whether you’ve reduced pain or discomfort
- How confident you feel using the therapy
These indicators help them decide whether you should:
- Continue EMS as-is
- Increase intensity or frequency
- Combine EMS with prosthetic training
- Switch to home-based EMS for independent use
If you’re using EMS to prepare for a bionic hand, like Grippy™, your therapist may test your myoelectric signal strength using sensors. This helps them see if your body is ready to control a device in real-time.
Step 2: Consider a Home EMS Plan
If you’ve grown comfortable with EMS and have seen results, your therapist may recommend switching to a home EMS routine.
This means using a compact EMS device at home, on your schedule, with a plan tailored to your needs.
Home EMS gives you freedom. It allows you to stay consistent, even after formal therapy sessions slow down. It also builds independence, which is a huge part of recovery.
Make sure your plan includes:
- Clear instructions on pad placement
- Safe intensity levels
- Time limits and rest breaks
- A logbook or app to track progress
Ask your therapist to review your first few home sessions if possible. That extra support can make the transition smoother.
Step 3: Prepare for Device Integration
If EMS was part of your prosthetic training, this is when things start to come together.
Your therapist or prosthetist will likely start introducing bionic device trials. You’ll begin to test how your muscle signals work with a hand like Grippy™. These sessions may include:
- Opening and closing a prosthetic hand using your muscle
- Practicing grip and release
- Learning how to rest your muscle between signals
- Timing your movements to match real-world tasks
Everything you practiced with EMS becomes useful now. The contractions, the timing, the endurance—it all comes into play.
This is often the most exciting part of rehab. For many users, it’s the first time they feel truly in control again.
Step 4: Stay Consistent, Even When Life Gets Busy
The biggest challenge after 30 days? Consistency.
Once life picks up—school, work, family—it’s easy to let therapy slip into the background. But EMS is not just for early recovery. It continues to help long after you start using your prosthetic.
Make it part of your day. Like brushing your teeth. Keep your device nearby. Set reminders. Pair your sessions with music, a podcast, or a short meditation.
The results may not always be dramatic, but the long-term benefits are real.
Step 5: Join a Community of Support
You don’t have to go through this journey alone. Look for online or in-person groups of others using EMS, prosthetics, or bionic devices.
Share your wins. Ask questions. Learn from others.
At RoboBionics, we regularly connect users who have walked this path. We’ve seen friendships, mentorships, and support systems form—all because someone said, “Hey, I know what that feels like.”
If you’d like to be part of this network, reach out to us anytime.
Conclusion: You’ve Come So Far—Now Keep Going

The first 30 days of EMS rehab are about more than just muscle. They’re about hope, belief, and forward motion. They show you that even after limb loss, your body still has power. Your mind still has control. And your life still has endless potential.
You’ve already done something incredible—you’ve started.
Now it’s time to keep going.
Want guidance on what to do after your first month of EMS?
Book a free consultation with our team today: https://www.robobionics.in/bookdemo
We’re with you for every step of your journey—pulse by pulse, goal by goal.



